Pathology-Cardiac Flashcards
A 55 year old male comes to see you for his regular check up. He complains that when he runs on the treadmill, he gets chest pain that radiates into his left arm and jaw. It goes away after 5 minutes, but is severely limiting him from running. If you took a microscopic slice of his myocardium while he was running, what would they look like?
They would demonstrate significant mitochondrial swelling, a sign of cellular injury. However, since this is a case of stable angina, injury is reversible.
A 62 year old male complains of chest pain when he is out walking his dog. He says that it goes away if he rests for a few minutes. While in the clinic, you have him walk on a treadmill until he experiences chest pain. You then administer nitroglycerine and the pain goes away. What do you expect to see on this patient’s EKG?
A depressed ST interval. This is characteristic of subendocardial damage that occurs in stable angina.
A 71 year old female presents to the ED complaining of an onset of chest pain while she was watching TV in the nursing home. You run an EKG and it shows ST segment depression and her symptoms improve after you give her nitroglycerine. What do you expect to see if you perform an angiogram? What is she at particular risk for?
This sounds like unstable angina. In an angiogram you would likely see incomplete occlusion of a coronary vessel by plaque or thrombus. The ischemia caused by the thrombus is still reversible in unstable angina; however, she is at high risk for progression to an MI.
A 47 year old male comes to see you complaining of episodes of chest pain that are not related to exertion. You give him nitroglycerine and his symptoms subside, then you send him home with calcium channel blockers. What do you expect to see on this patient’s EKG?
An elevated ST segment. This is Prinzmetal Angina, which is vasospasm of the coronary arteries that cause full occlusion of the artery. This is why calcium channel blockers were sent home with him, to prevent vasospasm.
A 61 year old female comes to the emergency department complaining of severe, crushing chest pain that radiates to her jaw. She is short of breath, sweating and symptoms are not relieved by nitroglycerine. She has a history of high cholesterol. What is most likely causing her symptoms?
She is having an MI caused by tearing away of an atherosclerotic plaque that is completely occluding a coronary artery. This complete occlusion is why nitroglycerine did not work for her.
A patient presented to the ER with an MI. He needs an angioplasty within 20 minutes of the onset of his symptoms or irreversible damage will begin to occur in his cardiac myocytes. What is the first vessel you will look at for coronary artery occlusion? If your guess is correct, which areas are at risk for infarction?
LAD. This is the most commonly occluded coronary artery and it supplies blood to the anterior wall of the LV and the anterior portion of the interventricular septum.
A patient presented to the ER with an MI. He needs an angioplasty within 20 minutes of the onset of his symptoms or irreversible damage will begin to occur in his cardiac myocytes. What is the second vessel you will look at for coronary artery occlusion? If your guess is correct, which areas are at risk for infarction?
RCA. This is the second most occluded coronary artery. It supplies blood to the posterior wall of the LV and posterior portion of the IV septum.
A patient presented to the ER with an MI. He needs an angioplasty within 20 minutes of the onset of his symptoms or irreversible damage will begin to occur in his cardiac myocytes. What is the third vessel you will look at for coronary artery occlusion? If your guess is correct, which areas are at risk for infarction?
LCX. It is the third most occluded coronary artery. It supplies blood to the lateral wall of the LV.
A 36 year old male comes to the ED complaining of chest pain. EKG shows depressed ST segments and blood tests show elevated CK-MB. He recovers and he is sent home. Four days later, he comes back with elevated ST segments. What blood markers will be helpful in developing a diagnosis in this patient?
MIs start with subendocardial infarcts that generate depressed ST segments. As they progress to transmural infarcts, the ST segments become elevated. The most sensitive and specific marker for MI is Troponin I (rises 2-4 hours after infarct, peaks at 24 hours and returns to normal at 7-10 days). CK-MB rises 4-6 hours after infarct and returns to normal after 72 hours. Combination of these two markers will show either a second infarct or continuation of the old infarct.
You are doing rounds and go into the room of a 65 year old female recovering from a heart attack. She has been there for a few days and you feel that she is able to recover at home. You tell her to take it easy because stress on the heart during the recovery period can be catastrophic. What drugs would you send her home with to assist in decreasing the overall stress on her heart?
Aspirin (reduce clots), supplemental oxygen (reduce ischemia), nitrates (vasodilate and decrease afterload), beta-blocker (decrease heart rate and contractility) and ACE inhibitor (decrease after load).
A 46 year old male is brought to the ED after complaining of severe chest pain and dyspnea. CK-MB and Troponin I levels are very high and you decide to administer heparin for fibrinolysis. What type of myocyte injury are you putting the patient at risk for? Why might his CK-MB and Troponin I levels continue to rise after fibrinolysis?
Contraction bands (reperfusion of Ca2+ to dead myocytes causes contraction of anucleate cardiac myocytes). Reperfusion injury (returning O2 results in generation free radicals and further injury to cardiac myocytes).
A 42 year old female presents to the ED suffering from an MI for the last 4 hours. What do you expect her cardiac myocytes to look like histologically and grossly during the first four hours? After 1 day? 4 days? 1 week? 1 month? What are major complications associated with each time period?
< 4 HOURS = no gross or histologic change, cardiogenic shock, acute heart failure and arrhythmias. 1 DAY = coagulative necrosis (pyknosis, karyolysis, karyohexis, dark discoloration, arrhythmias. 4 DAYS = inflammation (neutrophils = fibrinous pericarditis, monocytes = rupture), yellow pallor. 1 WEEK = granulation tissue, red border emerging from edge of infarct. 1 MONTH = scar formation.
A patient of yours comes to see you for a follow up visit after a heart attack he had a three days ago. He says that he still has some chest pain. You listen to his heart an note a friction rub. What can you infer from this finding?
He had a transmural infarction that has resulted in fibrinous pericarditis, thus the friction rub and chest pain.
A patient of yours comes to see you for a follow up visit after a heart attack he had a week ago. He says that he feels shortness of breath while sleeping at night. You listen to his heart an note a holosystolic murmur at the apex. In what coronary artery did this man likely have an infarction?
The right coronary artery. At about one week post-infarct macrophages are disposing of necrotic tissue and the infarcted area becomes very weak. Since the RCA supplies the papillary muscles, it is likely that a papillary muscle has torn, causing severe mitral regurgitation.
A patient of yours comes to see you for a follow up visit after a heart attack he had a week ago. He says that he feels rapidly increasing shortness of breath and dizziness. You listen to his heart an note a decreased heart sounds. What do you do next?
Get out the ultrasound and look for cardiac tamponade. It is likely that macrophage activity has weakened his heart causing a rupture through the ventricular wall and blood is filling the pericardial cavity.
A patient of yours comes to see you for a follow up visit after a heart attack he had a year ago. He says that he feels great. You look at his heart in an echocardiogram and note a significant transmural thrombus. What is this patient at high risk for?
Formation of mural thrombi indicate a significant scar within the ventricle. Large scars in the ventricles are also prone to aneurism.
A patient comes to see you for a followup visit 7 weeks after an MI. He complains of severe chest pain. You run a blood test on him and his WBC and CRP values are elevated. What rare condition might this patient have developed?
Dressler syndrome. This happens when the damaged myocardium is exposed to the immune system and you have an autoimmune reaction to the myocardium causing an acute pericarditis.
How long post-infarction and what type of infection do you see in this image?

*

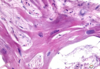
A biopsy of a patient’s infarcted tissue is shown below. How long has it been since the infarction?

4-24 hours. Note absence of nuclei and neutrophils.

What is this patient at risk for if the infarcted tissue was a transmural infarction?

Fibrinous pericarditis. Note the neutrophil infiltrate indicating it has been less than one week since the infarction?

When are post-MI patients at particular risk for the event seen below?

4-7 days. This is when macrophages are eating up necrotic tissue and the heart is weakened and prone to rupture.

What post-MI process causes the ventricular aneurism seen below?

Deposition of dense type I collagen that is weaker than the rest of the myocardium, putting the heart at risk for aneurism.

You get a call from your neighbor saying his wife suddenly passed away. She showed no prior symptoms and dropped dead on the spot. You determine she died from sudden cardiac death. What was the most likely cause of her death? What less common factors can cause sudden cardiac death?
90% of people have preexisting atherosclerosis and ischemia can be the cause of death. Other factors inlude mitral valve prolapse, cardiomyopathy and cocaine abuse (vassal spasm).
A 7 year old female comes to your clinic after a 2 week bout with flu-like symptoms. She is now having symptoms of lightheadedness while running. You suspect rheumatic fever-induced damage to her mitral valve. What is the molecular basis of her disease and how could you test to confirm it?
Molecular mimicry of beta-hemolytic strep A’s M protein. You can test for beta-hemolytic strep infections with ASO (anti-streptolysin O) or anti-DNase B titers.