Pathology of the Testis Flashcards
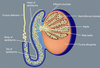
How would you be able to recognise a normal testicular sample?
- It’s smooth and soft
- you would be able to pull out a string of tissue that is very long
- the coiled seminiferous tubules
Review this image and identify key structures

What is the aetiology of Acute Epididiymo-orchitis?
- Most cases of acute epididymo-orchitis occur in men aged 20 – 39 years
- Associated with sexually transmitted diseases such as Chlamydia trachomatis and Neisseria gonorrhoea
- In older men over 40 years the most common cause is E.coli infection
- The inflammation is initially confined to the epididymis and later spreads to the testis
What is Acute Epididymo-orchitis and what are its symptoms/ presentations?
- clinical investigations
- inflammation of the epididymis
- Pain and swollen epididymis due to inflammation with a predominance of neutrophils
- Clinical investigations show
- raised C-Reactive protein
- a culture and sensitivity of urethral secretions to identify the bacterial cause
- ultrasound scan to differentiate epididymo-orchitis from torsion
What is the treatment and management for epididymo-orchitis
- Treat with antibiotics, pain relief and supportive care (scrotal elevation)
- If not resolved may require inpatient care
- May heal with scarring leading to sterility
Why does Torsion occur and how is it managed?
-
- Torsion occurs due to twisting of the spermatic cord which cuts off the venous drainage of the testis
- Presents with sudden onset of testicular pain which may or may not be related to trauma
- If untreated leads to infarction of the testis
- If ‘untwisted’ within 6 hours there is a chance that the testis will remain viable
- The contralateral testis should be fixed to the scrotum (orchidopexy) to risk reduce risk of torsion
What is this an image of?

Torsion of the Testis
Give an overview of the epidemiology of Testicular Cancer
- Most common solid malignant tumour in men 30-34 years of age
- Incidence of testicular cancer higher in caucasian men than black men
- Testicular cancer accounts for less 1% of all new cancers in the UK with 28% increase since the early 1990s
What are the causes of Testicular Cancer?
- Cryptorchidism/undescended testis increases the risk of cancer 4 – 8 times
- History of previous testicular cancer (father and brother)
- Genetic abnormality: Klinefelter’s syndrome (47XXY) & Down’s syndrome (trisomy 21)
- FH of testicular cancer – First degree relatives have a higher risk than the general population
- Men with infertility problems are more likely to develop testicular cancer
- Exposure to oestrogens (diethylstilbestrol) in utero → cryptorchidism→ increases the risk of testicular cancer
- given to women who are threatened risk of miscarriage –> increases risk of undescended testis –> increase risk of testicular cancer
How are Testicular Tumours classified?
- Germ Cell Tumours
- Seminiomatous tumours
- non-seminomatous tumours
- Sex Cord/Stromal Tumours (Less than 5% of testicular tumours)
- Leydig cell tumour
- Sertoli tumour
Give an overview of Germ Cell Tumours
- More than 90% of cancers of the testis arise in germ cells
- Germ cells produce the sperm
- Germ cell tumours are divided into seminomas and non-seminomatous
- Mixed germ cell tumours consists of seminoma and non-seminomatous components
- Germ cell carcinoma in situ or intra-tubular germ cell neoplasia is the precursor lesion (precancerous)
Explain what type of Tumours Semnomas are
- Seminomas tend to grow and spread more slowly than non-seminomatous tumours, they are a type of Germ Cell layer tumour
- There are two main sub-types:
-
Classical Seminoma:
- Constitutes more than 95% of seminomas
- Affect men between 25 and 45 years of age
- Tumours markers can be normal or raised
-
Spermatocytic Seminoma/Tumour:
- Rare tumour; affects older men; average age of 65yrs
- Grow more slowly than classical seminomas and are less likely to spread to other parts of the body
Explain what Non-seminomatous Tumours are
- germ cell tumours that usually occur in men in their late teens and early 30s
- Four main types of non-seminomatous germ cell tumours
- Embryonal carcinoma
- Yolk sac carcinoma/tumour
- Choriocarcinoma
- Teratoma
Explain what Embryonal Carcinomas are
- They are a form of Non-seminomatous germ cell tumour
- Present in about 40% of testicular tumours
- Pure embryonal carcinoma occurs in only 3% to 4% of cases
- tend to present as part of the mixed GCT
- Microscopically, looks like tissues of very early embryos
- Tends to grow rapidly and spread outside the testis (very aggressive tumour)
Explain what Yolk Sac Carcinoma/Tumour is
- a type of non-seminomatous GCT
- The cells look like the yolk sac of an early embryo
- The most common form of testicular cancer in children
- Pure yolk sac tumours are rare in adults
- Have better prognosis in children than adults
Explain what a Choricarcinoma is
- a type of non-seminomatous GCT
- A very rare and fast-growing testicular cancer in adults
- Pure choriocarcinoma tends to spread rapidly to other parts of the body, including the lungs, bones, and brain
- Usually present in mixed germ cell tumours with associated haemorrhage
- can present in women after pregnancy, due to abnormal trophoblastic proliferation
- both will have raised beta-HCG
Explain what a Teratoma is
- a non-seminomatous GCT from three layers of the embryo
- Endoderm (innermost layer)
- Mesoderm (middle layer)
- Ectoderm (outer layer)
- Pure teratomas of the testicles are rare
- No increase tumour markers
- Most teratomas are components of mixed germ cell tumours
What types of Teratomas are there?
-
Mature teratomas
- Tumours are formed by cells similar to adult tissues
- They rarely spread, can usually be cured with surgery, but may recur after treatment
-
Immature teratomas
- Are less well-developed cancers with cells that resemble those of an early embryo
- More likely than a mature teratoma to invade nearby tissues, metastasise outside the testis and recur years after treatment.
- teratomas are always malignant int the testis but not malignant in the ovaries
What are the clinical presentation of testicular cancer?
- Any painless swelling or nodule in the testis is cancer until proved otherwise
- Mass or nodule not separate from the testis
- Dull ache or heavy sensation in the lower abdomen
- Advanced cancer + mets may present with:
- Back pain due to enlarged para-aortic L nodes
- Supraclavicular lymphadenopathy
- Cough, chest pain, haemoptysis and shortness of breath due to metastases to the lungs
- Marked gynecomastia in patients with tumours secreting beta HCG as in choriocarcinoma
What imaging is used in Testicular Cancer?
-
Ultrasound scan (USS) will distinguish between:
- A tumour in the testis and external to the testis
- is it from the epididymis
- A complex cyst: most likely malignant and a simple cyst: most likely benign
- A solid tumour and a cyst
- A tumour in the testis and external to the testis
- CT scan: chest, abdomen and pelvis to assess for metastases in the lymph nodes, liver and lungs
- MRI of brain and bone if metastases suspected
- PET scan for recurrent disease after treatment lesions appear ‘hot’ when there is a viable cancer
What are the tumour markers in testicular cancer?
- Different tumours secrete specific TMs
- Alpha-fetoprotein (AFP) - yolk sac tumour, embryonal carcinoma
- Human chorionic gonadotropin (HCG) - Choriocarcinoma, embryonal carcinoma, seminoma
- Lactate dehydrogenase (LDH) - seminoma
- All TMs are raised in a mixed germ cell tumour
- TMs used for follow-up of patients after therapy
What is the treatment for Testicular cancer?
- Radical orchidectomy with isolated testicular mass followed by adjuvant chemotherapy
- If metastases are present at the time of presentation patients receive neo-adjuvant chemotherapy then orchidectomy
- There maybe no tumour in the removed testis on the pathological examination which is termed complete pathologic response to chemotherapy
- Patients are offered sperm banking prior to orchidectomy
- Patients are offered a prosthesis after orchidectomy


