Pathology: Cardiomyopathy Flashcards
1
Q
What causes Cardiomyopathies?
A

2
Q
- Three clinical, functional, and pathologic patterns are recognized.
- What are they?
- Which one is most common, which is the least common?
- Which are associated with diastolic dysfunction and which are associated with systolic dysfunction?
A

3
Q
For this type of Cardiomyopathy
- Describe the LC ejection fraction
- Mechanism of heart failure
- General Causes
- Secondary Myocardial Dysfunction
Dilated
A

4
Q
For this type of Cardiomyopathy
- Describe the LC ejection fraction
- Mechanism of heart failure
- General Causes
- Secondary Myocardial Dysfunction
Hypertrophic
A

5
Q
For this type of Cardiomyopathy
- Describe the LC ejection fraction
- Mechanism of heart failure
- General Causes
- Secondary Myocardial Dysfunction
Hypertrophic
A

6
Q
Dilated Cardiomyopathy
- What are the two main characteristics?
- What is it usually concurrent with?
- Why is early dx important for this disease?
A

7
Q
- Genetic and epidemiologic studies suggest that at least five pathways can lead to end-stage Dilated Cardiomyopathy
- List them
A

8
Q
Genetic Causes of Dilated Cardiomyopathy
- What percentage of cases are genetic?
- What kind of inheritance is usually the case?
- What mutations are involved?
- What protein is associated with the X-chromosome?
A

9
Q
Mutations in what protein accounts for approximately 20% of all dilated
cardiomyopathy?
A

10
Q
Pathogenesis of Dilated Cardiomyopathy
- Infection with what virus is most common in late-stage DCM?
- What condition is a common precursor to DCM?
A

11
Q
Pathogenesis of Dilated Cardiomyopathy: Toxic exposure
- What are some of the toxic agents that can cause DCM?
- Which agent is a chemotherapy drug?
- What is heart disease is associated with chronic alcohol abuse and its related consequences?
A

12
Q
Peripartum Cardiomyopathy
- When does this occur in pregnancy?
- What can cause this condition? (5)
- What is the primary defect in this condition, and what does it lead to?
A

13
Q
- How does Iron Overload lead to DCM?
- What genetic condition can lead to iron overload?
- What other type of cardiomyopathy can it cause?
A

14
Q
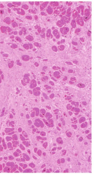
Morphology of Dilated Cardiomyopathy
- What are the general changes that occur to the heart?
- What type of thrombi are often present?
A

15
Q
- In DCM
- What happens to most myocytes?
- What areas of the heart show fibrosis?
- In DCM secondary to iron overload,
- What accumulates in cells
A