Observational Studies in CVD Flashcards
What are descriptive studies?
- describe a particular risk factor or disease
- e.g. observational studies: cases, ecological, cross-sectional
What are analytical studies?
- study cause and effect
- e.g. observational: case-control, cohort; interventional: clinical trials
Non-longitudinal studies
Measures at one point in time with no follow up
e.g. case, ecologcial, cross-sectional, case-control
Longitudinal studies
Have a follow-up after a period of time
e.g. cohort, clinical trials
How is data collected for CS studies?
- questionnaires
- examinations
- investigations
- produce mostly descriptive outputs related to prevalence
What is the limitation of a CS study?
- associations among variables, not temporal relationships
- weak evidence of causality
- hypothesis generating rather than supporting
- cannot determine cause and effect
What is an example of a CS study?
AusDiab: The Australian Diabetes, Obesity and Lifestyle Study
2000, 11000 people, CHD, diabetes and other diseases
prevalence data
Case control studies compare
Previous exposure status to a particular risk factor between cases and controls
In retrospective study designs
- cohort or case-control studies
- outcome of interest has already ocurred at initiation of the study
- looking to the past to identify a commong risk factor
What are the benefits of case-control studies?
- explicit knowledge of temporal relationships between exposure and outcome
- useful for rare outcomes
What are the drawbacks of case-control studies?
- Cannot investigate the true temporal relationsjip between the exposure and the outcome
- cannot infer incidence
What is an odds ratio?
- approximation of relative risk of outcome conferred by exposure
- output of case-control studies
What is the key output of a case-control study?
The odds ratio: an approximation of relative risk
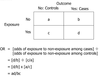
How is the odds ratio calculated?
OR= [odds of exposure to non-exposure among cases]/[odds of exposure to non-exposure among controls]
What is an example of a case-control study?
The INTERHEART study
- effect of modifiable risk factors associated with MI differs across coutnries
- e.g. smokers have 2.87x risk of MI
What are the hallmarks of a cohort study?
- longitudinal (w/follow-up)
- incidence data
- comparison of outcomes between/subgroups (e.g. exposed vs non-exposed)
- derive relative risk
What is a prospective cohort study?
- people classified by exposure (risk factor) prior to outomce
- allows knowledge of temporal relationship between exposure and outcome
What is a retrospective cohort study?
- use data already available for a cohort and the cohort has developed the outcomes
- more cost-effective
- e.g. registered patient data at a heart failure clinic
What are the advantages to a cohort study?
- Study multiple exposures and outcomes can be assessed
- Can research hypotheses post-hoc (i.e. retrospective)
What are the disadvantages of cohort studies?
- difficult for rare outcomes
- not cheap or easy
Example of a cohort study?
Framingham Heart Study
- 5000 people, 1948
- est. risk factors for CVD (lipids, somking, BP, etc.)
- incidence of CVD, coronary HD, and stroke
- recruitment of offspring continued the study
What is active outcome ascertainment?
Passive?
Physical validation of an outcome by assessment (e.g. hospital visit)
Obtained from databases of hospital, clinic visits etc.
What is bias?
Unintentional error that causes a systematic difference between or among groups
What is selection bias type I?
systematic difference in people selected vs. not selected
- ‘worried well’ are more likely to participate but are usually more active and motivated in some way
- results are tf not generalizable
What is selection bias type II?
- Systematic differences in subjects within groups being compared
- may attribute to differences observed in results rather than exposure
- e.g. recruiting all cases from the hospital and all controls from outside
What is information bias?
- systematic differences in the way information is collected between/among groups being compared
- differences (partly) responsible for results
- e.g. BP cuffs on healthy and obese pt - cuffs are tighter on obese and tf influence BP measurements
Recall bias is
- a type of information bias
- people with the condition of interest are more likely to remember exposure to a risk factor
What is confounding?
- mistaken attribution for the relationship between two variables
- a confounder can independently alter the outcome
- it can be related to the exposure
- e.g. age, sex

How can confounding be minimized?
- match by confounders (e.g. age, sex)
- restriction criterea (e.g. only males)
- stratification analysis (by sub-groups)
- multivariate analyses


