Neuro Path Flashcards

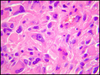
Astrocyte cells
Astrocytes are thought to perform a supportive role in the CNS
Astrocytes multiply and become hypertrophied in response to a variety of CNS injurious processes


Oligodendrocytes: produce CNS myelin
- Diseases that damage/destroy oligodendrocytes–> loss of myelin

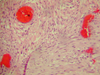
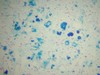
Microglial cell:
- NOT neuroepithelial, derived from monocyte macrophage lineage incorporated into CNS during fetal development
- *Below**:
- Microglial cells form network of CNS antigen presenting cells for immune surveillance
- Activation–> proliferation, migration of microglia
- Most pronounced in viral encephalitis

What type of injury occured to the brain specimen below?

- *Epidural hematoma**:
- Transtentorial herniation–> damage to vital cardio-respiratory centers in brainstem–> death due to epidural hematoma
- *Increasaed supratentorial pressure**:
- Many causes of increased intracranial pressure including intracerebral hemorrhage, tumor, liver failure, encephalitis
- Transtentorial herniation results in compression of uncus against midbrain resulting in 3rd nerve palsy
- Rostrocaudal displacement of brainstem can cause intraparenchymal (Duret) hemorrhages in brain stem
- Loss of brainstem function can result in death.
Below: compression of midbrain against tentorium–> compression of PCA–> formation of kernohan’s notch
Can also see duret hemorrhages= torsion on small blood vessels in pons/brainstem
- *Hepatic encephalopathy** can also cause herniation:
- toxic metabolites not metabolized in liver (liver failure)–> altered astrocyte function–> massive cerebral edema–> herniation

What type of injury occured to the brain specimen below?

- *Subdural hematoma**:
- Accumulation of blood in subdural space (beneath dura, above leptomeninges
- Results from torn bridging veins
- Death in 74% of cases
- Good recovery in 8% of cases
- Large clinically significant subdural hematomas almost always traumatic.
- Subdural blood does not enter the subarachnoid space. - Would not be detected as blood on spinal tap.
Ex: elderly have cerebral atrophy–> bridging veins span greater distance–> more susceptible to damage
What type of injury occured to the brain specimen below?

Subarachnoid hemorrhage
Bleeding into subarachnoid space
Due to:
- Trauma
- Rupture of saccular aneurysm (66%)
- Rupture of AV malformation (10-15%)
- Infection
- Vasculitis
- Tumor
Subarachnoid blood–> reactive vasospasm–> secondary ischemic brain injury
Below: see blood in subarachnoid space, below leptomeninges

What type of injury occured to the brain specimen below?

Impact to head–> cerebral parenchymal hemorrhage:
Intraparenchymal hemorrhage due to severe impacts
- rupture of intracerebral blood vessels
Cerebral contusions
Head impact related cerebral contusions results from the brain forcefully hitting the interior surface of the overlying skull.
- Contusions usually occur in areas of prominence of the cerebral hemispheres including the tips of frontal, temporal and occipital lobes
- *Contusion**= Bruise on the cortical surface
- Necrosis followed by phagocytosis of damaged cortex and white matter
- Coup lesions: at site of impact
- Countercoup lesion: Located at site distant from impact. Brain moves within skull due to impact to head and slams into skull at site remote from traumatic impact on head.
- *Histo:** linear hemorrhages arranged in perpendicular surface of brain where impact occurred
- Will also see macrophages in brain tissue (phagocytize necrotic tissue)
- Formation of hemosiderin stained areas on cerebral surface

A woman expires after getting into a MVA. There is no bruising visible on her skull or brain parenchyma, but the follow changes are noted in her brain tissue. What happened and what caused this?

Diffuse axonal injury:
Results from rotational acceleration of the brain within the head. (can occur in absence of impact)
Three characteristic features of the pathology of DAI in its most severe form include:
1) diffuse damage to axons
2) a focal lesion in the corpus callosum
3) focal lesions in the dorsolateral sector of the rostral brain stem adjacent to the superior cerebellar peduncles.
Can result in formation of numerous axonal spheroids
- Blocks axonal flow–> buildup in one space (indicates axonal transection)

Below is the brain specimen from a 50 year old former heavyweight boxer who died of an MI. What types of changes have occured?

Chronic traumatic encephalopathy:
= progressive neurologic deterioration related to repeated traumatic brain as can occur in number of athletic activities.
- CTE is a slowly progressive tauopathy with a trauma associated etiology
Tauopathy= increased expression of Tau, neurofibrillary tangles
A 30 year old man involved in an altercation was shot in the head. He was taken to the Emergency Department where he was still breathing and had in tact pupillary reflexes. After 10 minutes he expired- what caused his death?

Projectile brain injury
Damage occurs in areas in and adjacent to bullet path including blood vessels. The resultant increase in intracranial pressure can result in brainstem herniation and death.
The following was noted on an MRI of a patient with a headache. What is the anomaly here and what would a physician be concerned about?

AV Malformation:
Disorganized mass of abnormal arteries and veins
- Direct connection between arterial and venous circulations
- Congenital cases result from lack of development of local capillary network
- Rate of bleeding is 2-4 % per year (with high mortality due to herniation)
See disorganized arrray of abnormal blod vessels–> abnormal communication between arteries and veins–> seizures, SAH, intraparenchymal hemorrhage

What is grossly abnormal in this brain specimen of a 25 year-old patient who reported to the ED with the “worst headache of his life” and subsequently expired?

AV Malformation:
Disorganized mass of abnormal arteries and veins
- Direct connection between arterial and venous circulations
- Congenital cases result from lack of development of local capillary network
- Rate of bleeding is 2-4 % per year (with high mortality due to herniation)
- Seen more commonly in individuals age 20-40 years
See disorganized arrray of abnormal blod vessels–> abnormal communication between arteries and veins–> seizures, SAH, intraparenchymal hemorrhage
Histo: varied wall thickness and lumen caliber. Some vessels have hyalinized walls and arteries. Hemosiderin in intervening reactive brain parenchyma indicates previous bleeding. Arteries contain internal elastic lamina

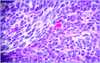
The following histologic specimen was recovered from the brain of a 70-year-old man who passed away from an MI. What types of changes are noted in the vasculature of his brain?

- *Cavernous hemangioma**:
- Venous vascular malformation
- Dilated vascular channels
- Large vascular spaces with fibrous walls and little or no intervening brain parenchyma
- Seizures, headaches or neurologic deficits
- Most are asymptomatic
- May rarely result in intraparenchymal bleed


Telangiectasias consist of an aggregate of small thin-walled blood vessels with intervening parenchyma.
They may cause seizures but rarely rupture.

A 79 year old man expires after developing gradual symptoms of dementia. The following is noted in a histologic specimen of his brain. What is his diagnosis?

Cerebral Amyloid Angiopathy:
Cortically located lobar hemorrhage
Pts older than 60 with majority (88%) > 70
Beta amyloid accumulates in media (replaces smooth muscle)- seen in adventitial tunica of arterioles, medium sized and small arteries
- *Overlap with Alzheimer’s disease**
- Both associated with Apolipoprotein e4
- CAA common in alzheimer’s dz, however, only 20-40% of CAA pts have clinical dementia
** Common cause of frontal lobe intraparenchymal bleeds in elderly (risk for intracerebral hemorrhage)
Diagnosis: Boston Criteria
- Definite: postmortem examination
- Probable with supporting pathology: Bx or evacuated hematoma c/w CAA
- Probable: MRI / CT with ≥ 2 lobar hemorrhages (microhemorrhages) in pt ≥ 55 (no other cause)
- Possible: MRI / CT with 1 lobar hemorrhage in pt ≥ 55 (no other cause)
* Microhemorrhages in deeper structure (basal ganglia)= hypertensive hemorrhage
- *Below**:
- Iron stain shows abundant iron deposition near old cerebral amyloid-related hemorrage
An 80 year old woman expires after progressive dementia-related degeneration. Additionally she had suffered from severe headaches for the last 20 years. She had been diagnosed with Alzheimer’s disease but on autopsy the following changes were found. What is notable in the histologic sample and what is her diagnosis?

Cerebral amyloid angiopathy:
Cortically located lobar hemorrhage
Pts older than 60 with majority (88%) > 70
Beta amyloid accumulates in media (replaces smooth muscle)
- *Overlap with Alzheimer’s disease**
- Both associated with Apolipoprotein e4
- CAA common in alzheimer’s dz, however, only 20-40% of CAA pts have clinical dementia
** Common cause of frontal lobe intraparenchymal bleeds in elderly (risk for intracerebral hemorrhage)
Diagnosis: Boston Criteria
- Definite: postmortem examination
- Probable with supporting pathology: Bx or evacuated hematoma c/w CAA
- Probable: MRI / CT with ≥ 2 lobar hemorrhages (microhemorrhages) in pt ≥ 55 (no other cause)
- Possible: MRI / CT with 1 lobar hemorrhage in pt ≥ 55 (no other cause)
* Microhemorrhages in deeper structure (basal ganglia)= hypertensive hemorrhage
- *Histo:** focus of old infarct with hemorrhage near CAA-related cerebral hemorrhage. See old cystic necrosis due to remote hemorrhage
- Additionally see degeneration of white matter due to decreased vascularization
MRI:
Inflammatory CAA presents with marked headaches and causes patchy or confluent bright signal on T2 weighted MRI

On post-mortem exam the following changes were noted in the circle of Willis of a patient with a family history of sudden death following painful headaches. What is noted in the arterial structure and what might have led to the death of this patient?

Saccular aneurysms:
Acquired lesions; loss of internal elastic lamina, muscularis at junction of artery with aneurysm
- Aneurysm has thinned fibrous wall vs normal muscular, elastic lamina
- Thin, dilated structure–> risk for rupture
** Rupture of saccular (berry) aneurysm–> life-threatening, 35% mortality during initial hemorrhage
- 2/3 of Subarachnoid hemorrhage are secondary to aneurysm rupture
- 10-15% due to AV malformations
- Blood in subarachnoid space–> vasospasm of cerebral blood vessels–> secondary cerebral ischemia


Atherosclerotic brain aneurysm:
Fusiform dilitations of basilar and vertebral arteries due to severe atherosclerosis
- Major complication= thrombosis
A 55 year old woman with a 30-year history of systemic lupus expires from an MI due to CAD. She had developed multiple manifestations of the disease (cutaneous, pulmonary “shrinking lung”). Additionally, according to her children her mental “sharpness” had declined in recent years. Based on the histology of her brain, what may she have developed?

Vasculitis of cerebral blood vessel:
Secondary vasculitis of the CNS (more common) can be part of a variety of systemic illnesses including generalized
autoimmune disease such as:
- SLE
- Sjogren’s syndrome
a variety of systemic vasculitides such as:
- Wegener’s Granulomatosis
- Polyarteritis nodosa
Primary CNS vasculitis (primary angiitis of CNS):
- No other disease or condition causing vessel damage
- Often granulomatous (below)

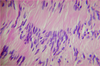
A 74 year old man with long-standing HTN who refused to take any medications or change his lifestyle comes to the ED after collapsing in his home. He is unresponsive and demonstrates R-sided paralysis and eventually expires. At autopsy there are signs of massive hemorrhage within the thalamus and the following histologic changes are found. What is his diagnosis?

Hypertensive Hemorrhage
Rupture of a cerebral blood vessel as a consequence of long standing hypertension
The most common locations for hypertensive cerebral hemorrhages are:
- the basal ganglia and thalamus (65%),
- the pons (15%)
- the cerebellum (8%).
May be related to lipohyalinosis of small vessel walls–> formation of microscopic Charcot-Bouchard aneurysms
Hemorrhage in the region of the internal capsule causes paralysis of the opposite side of the body.
- Patients are usually however unconscious
An acute hemorrhage in the pons may damage cranial nerve nuclei or result in loss of consciousness due to damage to reticular formation.
A cerebellar hemorrhage may cause abrupt ataxia, severe occipital headache and vomiting and may cause life-threatening compression of medulla.
- *Histo:** hypertensive arteriosclerosis in patient with long-standing HTN
- front: Charcot-bouchard aneurysms (mural deposition of lipid, hyaline–> damage to cerebral arterioles)

A 39 year old woman goes into labor and delivers a healthy baby, but suffers from major bleeding during delivery. During the operation to repair the bleed she suffers a stroke and expires. At autopsy the following is noted. What happened?

Watershed infarct:
Reduced blood flow to the brain –>
produce areas of ischemic injury in the watershed areas between:
- ACA–> MCA
- MCA–> PCA
A 25 year old man falls into a lake while out on a boat with his friends and knocks his head on the side of the boat. He nearly drowns but is resuscitated on the beach. Afterwards, he goes to his physician because he feels like he’s having trouble remembering things that he didn’t used to have problems with. Based on the histologic specimen below, what has occured to his brain?

Global ischemia: Sommer’s sector:
Produces damage in areas of the brain most sensitive to anoxic/hypoxic injury. These include:
1) Sommer’s sector (CA 1) of the hippocampus- front
2) Purkinje cells of the cerebellum
3) Layers IV to VI of the cerebral cortex (below)
- may see deficits in voluntary movements, associations (between visual/sensory cues and memory)
- Neuronal death seen in cell populations sensitive to anoxic/hypoxic injury

A 30 year old woman is in a motor vehicle accident where she is knocked unconcious and is found non-responsive and not breathing. Resuscitation is performed for 25 minutes and she eventually begins breathing again. After a long recovery in the hospital, her family notes that she seems to have trouble walking and is more clumsy. Based on the histologic changes below, what occured?

Global ischemia- Purkinje Fiber death:
Produces damage in areas of the brain most sensitive to anoxic/hypoxic injury. These include:
1) Sommer’s sector (CA 1) of the hippocampus
2) Purkinje cells of the cerebellum
3) Layers IV to VI of the cerebral cortex
- Neuronal death seen in cell populations sensitive to anoxic/hypoxic injury

A 65 year old woman with a history of uncontrolled hypertension and progressive coronary artery disease suffers from a stroke. Afterwards she has difficulty forming sentences and appears extremely frustrated by her inability to answer questions or express herself. Based on the imaging below, what has occured?

MCA Cerebral infarct–> Broca’s aphasia (Brodmann 44 and 45)
Cerebrovascular occlusive disease (thrombotic and embolic) remains a major cause of morbidity and mortality in the United States and worldwide.
- Atherosclerosis predisposes to vascular thrombosis and embolic events.
- Geographic location of occluded vessel defines area of infarction and clinical symptoms.
Examples:
- Occlusion of the trifurcation of the MCA results in cortical infarction with motor and sensory loss and often aphasia (front).
- Striate branch occlusion causes damage to the internal capsule with subsequent motor defects.
HTN–> Narrowing (arteriosclerosis) of brain parenchymal arteries and arterioles–>
small cystic ischemic infarcts referred to as lacunar infarcts.
Severe disease with numerous lacunar infarcts can result in the clinical entity multi-infarct dementia.
Histology:
- Coagulative necrosis with acute inflammation
- Phagocytosis of cellular debris by macrophage
- Eventual cyst formation and surrounding reactive astrocytosis.
Below: Anterior cerebral artery (ACA) infarct