Neoplastic hematopathology Flashcards
Most common site of extranodal B cell lymphoma
stomach
B cell neoplasm demographics
- Low grade more common in older adults; high grade in kids and young adults
- Most B cell neoplasms have male predominance
- exceptions showing female predominance:
- primary mediastinal lymphoma
- follicular lymphoma
- MALT lymphoma
- exceptions showing female predominance:
- DLBCL > FL > CLL > mantle cell lymphoma
- CLL most common leukemia
CLL/SLL
- genetics
- age
- presentation
- morphology (SLL and CLL)
- immunophenotype
- molecular and cytogenetics
- transformation to
- CLL has strongest genetic influence of all B cell neoplasms
- Familial clustering in 5%
- Risk in 1st degree relatives is 5x baseline
- Median age = 65
- Presentation
- Adenopathy, splenomegaly, PBL and BM involvement
- autoimmunity; positive DAT in 30%
- immunodeficiency; hypogammaglobulinemia in 30-50%
- M protein occasionally
- Morphology
-
SLL
- Diffuse nodal involvement
- small lymphs, occasional prolymphocytes
- proliferation centers; many prolymphocytes (light and dark areas)
-
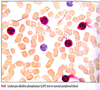
CLL
- small lymphs
- prolymphs < 11%
- 11-55% prolymphs = CLL/PLL
- smudged cells in EDTA; not seen in heparin smears
- lymphocyte count > 5 x 109/L (monoclonal B cell lymphocytosis under this number)
- small lymphs
-
SLL
- Immunophenotype
- positive for
- CD19
- CD20 (dim)
- CD22
- CD5
- CD43
- CD23
- sIg (dim)
- CD79a
- CD11c (dim and variable)
- bcl-2
- Negative for
- FMC-7
- CD10
- bcl-6
- CD38 and ZAP-70 expressed in half
- positive for
-
Molecular and cytogenetics
- most common cytogenetic abnormality is trisomy 12
- # 1 FISH abnormality: del 13q (good)
- others: tri 12, del(11q), del(14q), and del(17p)
- 20% have normal FISH
-
Transformation:
- most common form is PLL
- Richter (large cell lymphoma)
- rarely transforms to Hodgkin
CLL prognosis adversely affected by
- B symptoms
- Diffuse pattern of marrow involvement
- peripheral lymphocyte doubling time < 1 year
- high initial lymphocyte count (>30,000)
- unmutated Ig heavy chain gene variable region (IgVH)
- resemble pregerminal center B cells
- likely to progress
- candidates for treatment
- CD38 and ZAP-70 in > 30% of cells correlates with unmutated status
- Chromosomal status by FISH
- Good: normal karyotype or del(13q) only
- Poor: 11q or 17p deletions
Mantle cell lymphoma
- presentation
- morphology
- variants
- immunophenotype
- molecular and cytogentic
- prognosis adversely affected by
- Presentation
- adenopathy
- tends to involve Waldeyer ring and GI tract (lymphomatous polyposis)
- Morphology
- diffuse or vaguely nodular lymph node effacement
- small to medium sized lymphocytes, irregular nuclear contour, small subtle nucleolus
- mitoses frequent
- admixed histiocytes and hyalinized vessels
- neither proliferation centers nor prolymphocytes
- variants: blastoid, pleomorphic, small cell, marginal zonelike
- blastoid composed of large cells with high mitotic rate
- blastoid and pleomorphic more aggressive
- small cell variant resembles SLL; marginal zone like variant resembles MZL
- Immunophenotype
- positive for: CD19, CD20 (bright), CD22, FMC-7, CD5, CD43, sIg (bright), bcl-1 (cyclin D1, prad 1), blc-2
- negative for: CD23, CD11c, CD10, CD99
- Molecular and cytogenetic
-
Positive for t(11;14)
- rearrangment of JH region of IgH (14q32) to the CCND1 (11q13)
- results in cyclin D1 (bcl-1) amplification
- FISH is most sensitive
- most have additional abnormalities, often in chromosome 13
-
Positive for t(11;14)
- Prognosis adversely affected by mitotic rate > 10/HPF and Ki-67 > 40%
Follicular lymphoma
- presentation
- morphology
- grading
- diffuse growth
- FL variants
- in the marrow
- immunophenotype
- molecular and cytogenetic
- prognosis adversely affected by
- Presentation
- isolated lymphadenopathy without constitutional symptoms
- Morphology
- nodular lymphoid proliferation: back to back, fused follicles with attenuated mantles
- often overruns capsule
- follicles lack polarity, tingible body macrophages, plasma cells, and have few mitoses
- 2 cell types: small cleaved cells (centrocytes) and large noncleaved cells (centroblasts)
- Grading
- proportion of centroblasts in 10 fields
- grades 1 and 2 are low grade
- Grade 1: 0-5/HPF
- Grade 2: 6-15/HPF
- Grade 3
- 3A: >15/HPF + some residual centrocytes
- 3B: >15/HPF and no centrocytes
- Diffuse growth
- lack of follicles and dendritic cells by CD21 and/or CD23 IHC
- when low grade, called FL with focal diffuse growth
- when high grade, called DLBCL
- lack of follicles and dendritic cells by CD21 and/or CD23 IHC
- FL variants
-
Intrafollicular FL (FL in situ)
- intact interfollicular zones and open sinuses
- follicles have cytologic features of FL: purely centroblasts and centrocytes that express bcl-2
-
Isolated cutaneous FL
- good px
- lacks CD10 and bcl-2 expression
- bcl-6 positive
- lacks BCL2 rearrangement
-
Isolated GI FL
- good px
- duodenum
- Pediatric FL is usually grade 3
-
Intrafollicular FL (FL in situ)
-
In the marrow
- focal paratrabecular aggregates
- may be discordant with low grade in marrow and high grade in lymph node
-
Immunophenotype
- Positive: CD19, CD20 (bright), FMC-7, CD22, CD10, sIg (bright), bcl-2, and bcl-6
- Negative: CD5, CD43, CD11c, CD23
- Higher grade are less CD10 positive
- Ki-67 <20% in grades 1-2 and >20% in grade 3
- Background FDC express CD21 and CD23
- Molecular and cytogenetic
-
t(14;18)
- FISH is most sensitive
- Rearrangement of BCL2 on 18 with the J region of IgH on 14
- Results in overexpression of bcl-2 protein with antiapoptotic properties
- translocation not unique to FL and is most common encountered in B lineage lymphoma
- bcl-2 overexpression also not unique to FL; bcl-2 overexpression in non-FL usually not associated with t(14;18)
-
t(14;18)
- Prognosis adversely affected by
- higher age, stage, and serum LDH
- bone marrow involvement
- B symptoms
- low performance status
- anemia
Marginal zone lymphoma (MZL)
- presentation
- morphology
- immunophenotype
- molecular and cytogenetic
- Presentation
- Nodal
- Extranodal (MALT)
- Splenic
- Morphology
-
Nodal
- nodular or diffuse proliferation
- small lymphs, rounded to indented nuclei, abundant pale cytoplasm (monocytoid)
- associated with chronic antigenic stimulation
- most common site is GI tract (especially stomach)
- clonal plasma cells often present
-
Extranodal (MALT)
- variably destructive and/or tumefactive proliferation
- monocytoid B cells and clonal plasma cells
- lymphoepithelial lesions
- reactive polyclonal germinal centers can be present
-
Splenic
- expansion of white pulp
- involves splenic hilar lymph nodes often
- liver sinusoids involved
-
peripheral blood involvement
- splenic lymphoma with villous lymphocytes (SLVL)
- resembles HCL but SLVL more likely to
- display nucleoli
- display polar villous projections
-
Nodal
- Immunophenotype
- Positive: CD19, CD20, CD21, CD79A, FMC-7, bcl-2, sIg (IgM)
- Negative: CD5, CD23, CD10, CD103, annexin A1, CD11c
- plasma cells contain monoclonal cytoplasmic light chains
- CD43 is negative generally, but positive in 30% of MALT lymphoma
- Molecular and cytogenetic
- t(11;18) - rearrangement of API2 and MALT1 genes in stomach and lung
- t(14;18) - MALT1-IgH fusion: ocular, parotid, and cutaneous
- t(3;14) - FOXP1-MALT1 in ocular, thyroid, and cutaneous
- t(1;14) in lung and small bowel
- +3 and +18 in all sites
- A monoclonal gammopathy is present in 30-50% of cases
Hairy cell leukemia
- Presentation
- Morphology
- Immunophenotype
- Molecular findings
- Presentation
- neutropenia, monocytopenia, or aplastic anemia
- splenomegaly
- 4:1 male:female
- Morphology
- blood smears
- large lymphoid cells 2x the size of normal lymph
- nuclei round to reniform with smooth contour
- chromatin ground glass with indistinct to absent nucleoli
- hairy projections are circumferential
- Tissue
- Fried egg morphology
- reticulin fibrosis, blood lakes, and mast cells
- in spleen, cells infiltrate the red pulp
- in liver cells are in sinusoids
- Ultrastructure
- ribosome lamellar complexes
- Histochemistry
- cells contain tartrate resistant acid phosphatase (TRAP)
- weak TRAP nonspecific, but strong TRAP staining is specific
- blood smears
- Immunophenotype
- Positive: CD19, CD20, CD22, sIg, CD11C (bright), CD25 (bright), CD103, DBA.44, annexin A1, cyclin D1 (dim, nuclear)
- Negative: CD5, CD43, CD23, CD10
- 10% are CD10+
- No reproducible molecular findings
Prolymphocytic leukemia
- presents abruptly with a very high white count > 100,000/uL, B symptoms, cytopenia, and splenomegaly
- Definition: > 55% prolymphocytes (prominent nucleoli and a moderate quantity of cytoplasm)
Lymphoplasmacytic lymphoma/Waldenstrom macroglobulinemia
- how to diagnose LPL
- how to diagnose Waldentrom
- associated with
- morphology
- molecular and cytogenetics
- Lymphomas wtih plasmacytic features
- SLL/CLL, MCL, and MZL
- LPL diagnosed when these are excluded
- Waldenstrom macroglobulinemia is LPL with an IgM monoclonal gammopathy and marrow involvement
- Associated with HCV and cryoglobulinemia; may respond to anti viral therapy
- Morphology
- small lymphs to plasma cells
- Dutcher bodies possible
- Lymph nodes
- architecture may be normal or effaced
- PAS+ material in sinuses
- Immunophenotype
- Positive: CD19, CD20, CD38, sIg (bright), cIg (plasma cells)
- Negative: CD5, CD23, CD43, CD10
- Molecular and cytogenetic
- t(9;14) involving PAX5 and C region of IgH
Heavy chain disease
- only IgH are produced
- Most common form is alpha H chain disease
- a form of MALT lymphoma also called immunoproliferative small intestine disease (IPSID) or Mediterranean lymphoma, associated wtih C. jejuni
- gamma heavy chain disease (Franklin H chain disease) found in some cases of LPL
- mu heavy chain disease found in some cases of CLL
Diffuse large B cell lymphoma
- presentation
- morphology
- immunophenotype
- molecular and cytogenetic
- prognosis
- Presentation
- rapidly enlarging lymph node or extranodal site
- localized at presentation, bone marrow involvement uncommon (10%)
- Morphology
- diffuse nodal effacement by predominantly large cells (larger than a macrophage nucleus)
- Immunophenotype
- positive: CD19, CD20, CD22, CD45, often bcl-2
- variable: CD10, CD5, and bcl-6
- CD5 expressing cases must be distinguished from blastoid MCL (bcl-1+)
- Ki67 60-99%
- Molecular
- BCL2 and BCL6 rarrangements present in 20-30%
- BCL6 gene, 3(q27), rearranges with variety of partners, commonly t(3;14)
- rearrangements of BCL6 more common in the ABC type
- rearrangement of BCL2, t(14;18), more common in the GCB type
- BCL2 and BCL6 rarrangements present in 20-30%
- Prognosis
- germinal center-like has better response to treatment than activated B cell like (ABC)
- Germinal center-like type:
- CD10+ BCL6+ MUM1 -
- CD10+ BCL6 - MUM1-
- CD10- BCL6+ MUM1-
- Non germinal center type
- CD10 - BCL6+ MUM1+
- CD10 - BCL6- MUM1+
Stepwise evaluation of DLBCL subtypes by IHC
- CD10
- if positive, then it’s GC type
- if negative go to #2
- BCL6
- if negative, then non GC type
- if positive, then go to #3
- MUM1
- if positive, then non-GC
- if negative, then GC type
Primary DLBCL of the CNS
- median age
- location in brain
- presentation
- micro
- FISH results
- median age 60 years
- supratentorial mass with radiographic features that mimic GBM
- may present or recur as intraocular lymphoma
- tumor cells often in perivascular cuffs and express pan B antigens
- most cases have BCL6 rearrangement and overexpress bcl-6; BCL2 rearrangement is rare
T cell/histiocyte rich large B cell lymphoma (TCRBCL)
- median age
- micro
- IHC
- marrow
- median 40 years (children to old age)
- diffuse proliferation of small lymphocytes and histiocytes with scattered large B cells
- Small lymphocytes are a mixture of CD4+ and CD8+ T cells
-
absent are
- CD57+ T cells
- T cell rosettes
- small B cells
- CD21+/CD23+ FDC meshwork
-
absent are
- Large B cells express pan B markers and bcl-6; some are EMA+
- Can be positive for CD10
- negative for CD15, CD30, and EBV
- Involves marrow as paratrabecular lymphoid aggregates
Primary mediastinal (thymic) large B cell lymphoma
- gender, age
- micro
- IHC
- molecular
- young adult women, F:M = 2:1
- a sclerosing lymphoma with large B cells entrapped within bands of sclerosis
- Positive: CD45, CD19, CD20, CD79a, CD30
- NEGATIVE FOR surface Ig, CD10, CD5
- Altered MAL gene, gains in 9p (locations of JAK2)
- No rearrangement of BCL2 or BCL6
ALK+ large B cell lymphoma
Rare; immunoblastic/plasmablastic cells that express ALK
Plasmablastic lymphoma
- IHC
- patient population
- site of involvement
- rare; immunoblastic/plasmablastic cels
- Positive: CD38, CD138, IRF4/MUM1, cIg, EBV
- Negative: CD45, CD20, CD56 (in contrast to plasmayctoma)
- Found in HIV+ adults and arises mostly in extranodal sites such as oral cavity mucosa
Intravascular large B cell lymphoma
- aka
- symptoms
- aka angioendotheliomatosis, angiotropic lymphoma, and intravascular lymphomatosis
- symptoms related to small vessel obstruction by large B cells
- lymph node involvement rare
Primary effusion lymphoma
- associated with
- presentation
- micro
- IHC
- Associated with HHV8 and HIV
- Presents with effusion (pleural, pericardial, peritoneal)
- contains large B cells with immunoblastic/plasmablastic/anaplastic morphology and cytoplasmic vacuolization
- negative for B/T/myeloid antigens (CD20, CD79, CD19, CD10, CD3, CD5, CD13, CD14, CD33)
- Positive for CD45, CD30, CD38, CD138, EMA, HHV8
Leg type primary cutaneous DLBCL
rare; affects elderly women
EBV+ DLBCL of the elderly
- affects what population
- other EBV positive large B cell neoplasms
- rare; affects elderly Asian adults
- Other EBV+ large B cell neoplasms
- plasmablastic lymphoma
- PEL
- lymphomatoid granulomatosis
- DLBCL associated with chronic inflammation
- EBV+ DLBCL of the elderly
- EBV+ DLBCL, NOS
Lymphomatoid granulomatosis
- Large B cells destructively invade vessel walls resembling vasculitis
- many reactive T cells, plasma cells, histiocytes
- granulomas are uncommon
- most commonly affects lungs, upper aerodigestive tract, brain, kidneys, and liver
- associated wtih EBV and immunodeficiency
DLBCL associated with chronic inflammation
- forms within sites of longstanding inflammation (e.g., pyothorax)
- EBV+
Lymphoproliferative disorders arising in primary immunodeficiency
- Primary immunodeficiencies
- ataxia telangiectasia
- Wiskott Alrdich
- CVID
- X linked LP disorder (Duncan)
- Nijmegen chromosomal breakage syndrome
- Most common LPDs
- DLBCL, LG, and T cell neoplasm
Most common lymphomas in HIV
- BL
- DLBCL (especially CNS)
- PEL
- plasmablastic lymphoma
- HL
Posttransplant lymphoproliferative disorder
- occurs how long after transplant?
- heralded by?
- risk factors
- PTLD clone comes from donor or recipient?
- does it involve the allograft?
- Usually <1 year after transplant
- EBV implicated in most (especially in 1st year)
- Heralded by elevated EBV viral load
- Late (>5 years out) PTLD is most aggressive and EBV-
- Risk factors
- allograft
- renal and BMT have lowest risk
- heart-lung and liver-bowel have higher risk
- children
- EBV- at time of transplant
- allograft
- PTLD clone usually of recipient origin
- often involves the allograft itself
Burkitt lymphoma/leukemia
- Types
- Morphology (tissue and blood)
- Immunophenotype
- vs DLBCL, NOS
- vs B-LBL/B-ALL
- molecular
- 3 clinicopathologic types of Burkitt lymphoma are recognized
- African (endemic): jaw mass in child, EBV+
- Western (sporadic): nodal, abdominal, less associated with EBV; kids and adults
- Burkittlike lymphoma: nodes, IC hosts
- morphology
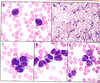
- tissue
- diffuse proliferation; medium sized nuclei with 2-5 nucleoli
- many tingible body macrophages, high rate of mits/apoptosis
- Wright stained blood
- deep blue cytoplasm with lipid containing vacuoles
- tissue
- Immunophenotype
- positive: CD19, CD20, CD22, CD10, bcl-6, sIg, C-myc
- negative: CD5, CD23, Tdt, CD34, bcl-2
- Ki67 >99%
- vs DLBCL, NOS
- BL positive for c-myc, negative for bcl-2, and Ki67 >99%
- BL unlikely if CD10 negative, bcl-6 negative, or bcl-2 positive
- BL unlikely if either BCL2 or BCL6 rearrangements are present
- vs B-LBL/B-ALL
- BL is Tdt negative, CD20 positive, and sIg positive
-
Molecular
- rearrangement of C-MYC on chromosome 8
- t(8;14)
- Igkappa t(2;8)
- Iglambda t(8;22)
Lymphoblastic leumkemia and lymphoma categories
- B-ALL/LBL, NOS
- B-ALL/LBL with recurrent cytogenetic abnormalities
- T-ALL/LBL
LBL vs ALL
- LBL: lesions involving tissue and sparing blood and marrow
- ALL: marked involvement of marrow (>25%) and blood (>20%) regardless of tissue involvement
- ALL: B lineage in 80%
- LBL: T lineage in 80%
Clinical presentation and morphology of ALL/LBL and morphology and cytochemistry
- B-ALL is most common malignancy in children; peaks at 3 years of age
- T-LBL presents as anterior mediastinal mass; hypercalcemia is common
-
Morphology
- undifferentiated blasts
- cytochemically negative for MPO and SBB; PAS+ in blocklike/coarse granular pattern
B-ALL/LBL, NOS
- immunophenotype
- prognosis
- hematogones vs ALL
- molecular and cytogenetic
- Immunophenotype
- positive: CD19, CD10, PAX5, CD34, CD99, HLA-DR, nuclear TdT
- Usually negative for CD20 and sIg
- absence of CD10 suggests MLL anomaly
- 30-50% express at least 1 myeloid antigen (CD13 or CD33)
- Prognosis
- Good
- lower initial white count
- 2-10 years old
- female
- complete remission (day 14 marrow) following induction chemo
- Good
- Hematogones vs ALL
- hematogones disperse, both in CD34 stained marrow sections and in flow plots
- blasts cluster
- by flow cytometry, hematogones display a range of expression of CD10, CD20, Cd34, Tdt, sIg
- blasts express a relativly uniform strength
- hematogones disperse, both in CD34 stained marrow sections and in flow plots
- Molecular and cytogenetic
- 6q
- 9p
- 12p
- “recurrent genetic abnormalities” absent
B-ALL/LBL with recurrent genetic abnormalities
- Most common structural abnormality is t(9;22)(q34;q11)
- unfavorable
- minor breakpoint (m-bcr) rearrangement, chimeric protein of 190kD most common
- t(v;11q23), usually t(4;11)
- MLL
- infants
- unfavorable
- overexpress FLT3
- t(12;21)
- TEL-AML1 (ETV6-RUNX1)
- 25% of children
- good
- Hyperdiploid
- >50
- 25% of children
- good
- Hypodiploid
- <46
- <5% of children
- unfavorable
- t(1;19)
- E2A-PBX1 (TCF3-PBX1)
- 5% of children
- unfavorable
- t(5;14)
- IL3-IGH
- <1% of children and adults
- usual prognosis
- eosinophilia
T-ALL
- immunophenotype
- molecular
- T-LBL vs thymoma
- Immunophenotype
- positive: CD99, CD7, CD2, CD5, CD3 (cytoplasmic), and TdT (nuclear)
- CD34 variable; HLA-DR is usually negative
- CD4 and CD8 often both positive or both negative
- some express myeloid antigens (CD13 or CD33)
- T-LBL vs thymoma
- Thymoma is EMA positive
- By flow, similar to distinction of hematogones and B-ALL
- Thymoma: dispersal plots of CD4 vs CD8 and CD45 vs CD3
- T-LBL: tight clustering in plots of CD4 vs CD8 and CD45 vs CD3
Plasma cell myeloma
- age
- race
- gender
- forms
- renal manifestations
- median 70 years
- blacks > whites
- males >females
- forms
- symptomatic
- smouldering
- renal manifestations
- hypercalcemia and/or hyperuricemia induced tubular injury
- AL amyloidosis most commonly found with lambda light chains
- Light chain deposition disease most commonly with kappa light chains
- myeloma cast nephropathy
Multiple myeloma
- paraproteins
- isotype (heavy chain) is most commonly IgG
- IgA (22%)
- none - light chain only (18%)
- IgD (1-2%)
- biclonal (1-2%)
- IgE (1-2%)
- idiotype (light chain) is most commonly kappa
- nonsecretory myeloma is found in 5% of cases
Multiple myeloma immunophenotype
- positive: CD38, CD138, CD56, cytoplasmic lambda or kappa, and PCA1
- negative: CD45, CD19, CD20, CD21, CD22, sIg
- some are cyclin D1+ (bcl-1), correlating with t(11;14)
- 10-30% express myelomonocytic markers (CD117, CD33, CD13, CD11b, CD15)
- 10-50% express CALLA (CD10)
- occasionally EMA and CD30+
Molecular and cytogenetics of multiple myeloma
- most common abnormality is in IgH (14q32)
- 14q32 rearrangement found in >70% of myeloma and 50% of MGUS
- t(11;14) produces CCND1/IgH fusion
Multiple myeloma prognosis (adverse)
- adverse:
- higher levels of beta2 microglobulin
- high plasma cell labeling index
- high stage
- chromosomal abnormalities by FISH
Plasma cell leukemia
- >20% or >2 x 109/L plasma cells in the peripheral blood
- 1/2 of cases present de novo
- present abruptly and follows an aggressive course
- high incidence of monosomy 13
- plasma cells often CD56 negative
Solitary cell leukemia
- solitary osseous plasmactyoma arises most often in vertebrae, ribs, and pelvis
- 1/2 have detectable M protein
- Most develop MM within 10 years
- Solitary extraosseous arises most commonly in the nasal cavity, oropharynx, or larynx
- most do not have a detectable M protein
- most do not develop MM
MGUS
- prevelance
- classification
- risk for development of MM or other PCN
- present in 3% of adults over the age of 50 years and 5% of adults over the age of 70 years
- 60% of patients with an M protein are classified as MGUS
- 1% progression per year to MM or another PCN
- after 20 years, 1 in 3 develops overt myeloma
T cell neoplasms
- 5% of lymphoid neoplasms
- incidence highest in Asia
- enteropathy associated T cell lymphoma strongly associated with Welsh and Irish ancestry
- Most common T cell neoplasms, in decreasing order: PTCL NOS, AITCL, ALCL, ATCL
Peripheral T cell lymphoma
- Any T cell neoplasm that does not fit any other clinicopathologic entity
- Most common T cell lymphoma
- Morphology
- diffuse proliferation of polymorphic small and large lymphoid cells
- neoplastic lymphs may have cloverleaf nuclei
- admixed eos, plasma cells, and/or histiocytes
- postcapillary venules may be prominent
- Immunophenotype
- CD4+
- CD8-
- Loss of one or several pan T cell markers
- CD25-
Adult T cell leukemia/lymphoma
- Caused by
- Clinical presentation
- Morphology
- Immunophenotype
- Caused by HTLV-1
- endemic in southwest Japan, Oceania, and the Caribbean
- rare in North America
- Lifetime risk of ATCL in HTLV-1 positive people is 5% (greater for men than women)
-
Clinical presentation
- LAD and HSM
- visceral involvement (CNS, lungs, GI tract)
- rash
- hyperCa
- lytic bone lesions
-
Morphology
- nuclear irregularity with cloverleaf or flower forms
-
Immunophenotype
- positive: CD2, CD3, CD5, CD4, and CD25
- negative: CD7 usually and CD8
Angioimmunoblastic T cell lymphoma (AITCL)
- associated with
- age
- presentation
- morphology
- immunophenotype
- EBV associated neoplasm affecting older adults
-
Clinical presentation
- abrupt onset
- constitutional symptoms: fever, night sweats, weight loss
- generalized LAD
- pruritic rash
- pleural effusion
- Coombs+ autoimmune hemolytic anemia
- cold agglutinins
- anti-smooth muscle antibody
- RF
- polyclonal hypergammaglobulinemia
-
Morphology
- diffuse nodal effacement with prominence of postcapillary venules
- immunoblasts, lymphs, plasma cells, eos, aggregates of cells with clear cytoplasm
- deposition of PAS+ extracellular material, and a mixed lymphoid infiltrate
- absence of apparent follicles; CD21 displays hyperplastic follicular dendritic cells
- Immunophenotype
- positive: CD4, most pan T markers (CD2, CD3, CD5, CD7) and TFH markers (CD10, bcl-6, CXCL-13)
- negative: CD8, loss of one or several pan T cell markers (CD2, CD3, CD5, CD7)
- EBV is present in B cells
Anaplastic large cell lymphoma
- population
- morphology
- prognosis
- immunophenotype
- molecular
- children and young adults
- 50% of childhood high grade lymphomas
- morphology
- diffuse proliferation with many large lymphs, some of which are anaplastic
- anaplastic cells cluster near blood vessels
- small cell variant is composed of large, but not anaplastic lymphoid cells; may be mistaken for PTCL
- prognosis depends on expression of Alk; Alk+ has best prognosis
- WHO classification has separate categories for Alk+ and Alk- ALCL
- Alk- ALCL has worse prognosis than Alk+ but better than PTCL NOS
- Immunophenotype
- positive: CD30 (membranous and golgi), clusterin, EMA, CD45
- often positive for myeloid antigens (CD13, CD33)
- often positive for T cell antigens (CD4)
- Alk expression correlates with t(2;5)
- with usual t(2;5) NPM-ALK, Alk is expressed in cytoplasm and nucleus
- variant translocations result in various patterns of Alk expression
- negative for B cell antigens, CD15, and EBV
- Molecular and cytogenetics
-
t(2;5) in >95%
- ALK (anaplastic lymphoma kinase) gene on 2p23 and NPM (nucleophosmin) on 5q
- clonal TCR rearrangement in 90%
-
t(2;5) in >95%
Large granular lymphocytic leukemia (LGL leukemia)
- define
Tc cytotoxic LGL leukemia:
- presentation (clinical, labs)
- immunophenotype
- cytogenetics
-
> 6 month increase (>2 x 109) in LGL
- may be T cells or NK cells
- Tc cytotoxic LGL leukemia
- neutropenia
- splenomegaly
- polyclonal hypergammaglobulinemia
- older men
- associated with rheumatoid arthritis
- usually indolent; more aggressive if CD56+ blast-like cells present
-
Immunophenotype
- positive: CD2, CD3, CD8, CD16, CD57, granzyme M, granzyme B
- negative: CD4, often negative/dim for CD7 and or CD5
- TCR rearranged
NK cell LGL leukemia
- presentation
- IHC
- molecular
- neutropenia, anemia, fever, jaundice, HSM
- EBV negative (in contrast to aggressive NK cell leukemia)
- Immunophenotype
- positive: CD2, CD16, CD56
- variable: CD7, CD8, CD57
- negative: surface CD3 (cytoplasmic epsilon chain of CD3 is positive) and CD4
- TCR germline
Aggressive NK cell leukemia
- aggressive EBV associated neoplasm
- Asians
- mean age 40
Nasal type NK/T cell leukemia
- extranodal, usually nasal, EBV associated neoplasm
- angioinvasive growth pattern
- more common in Asians, Native Americans
Enteropathy associated T cell lymphoma
- associated with
- sites affected
- MHC type
- immunophenotype
- high grade T cell lymphoma in patients with longstanding celiac sprue
- often preceded by refractory sprue with mucosal ulceration (ulcerative jejunoileitis)
- jejunum and/or ileum
- like sprue, Welsh and Irish ancestry common
- most have the HLADQA1*0501, DQB1*0201 genotype
- CD3+, CD30+, and usually CD4-/CD8-
Hepatosplenic T cell lymphoma types
-
gamma-delta type
- young males
- B symptoms
- HSM
- cytopenias
- CD8+ cytotoxic T cells that express gamma delta TCR and isochrome 7q
-
alpha-beta type
- female
- wider age distribution
Cutaneous T cell lymphoma
- IHC
- micro
- define MF
- define Sezary
- CTCL is a CD4+ T cell neoplasm with epidermotropic growth pattern
- small to large lymphoid cells with cerebriform nuclei
- MF is CTCL which involves lymph nodes
- Sezary syndrome is CTCL involving peripheral blood
Nodular lymphocyte predominant Hodgkin lymphoma
- morphology
- NLPHL vs TCRBCL
- NLPHL vs CHL
-
morphology
- nodular or vaguely nodular
- RS cells rare to absent
- L&H cells with large vesicular convoluted (popcorn) nucleus
- progressive tranformation of germinal centers thought to be precursor lesion
-
NLPHL vs TCRBCL
- Meshwork of follicular dendritic cells, highlighted by CD21 or CD23 IHC
- predominance of CD20+ B cells
- wreath of CD3+/CD57+ T cells
-
NLPHL vs CHL
- neoplastic cell in NLPHL
- L&H cells express CD45, CD20, surface Ig, bcl-6, and EMA, OCT2, BOB1 (latter two stains incorrectly described in Compendium)
- L&H cells negative for EBV
- neoplastic cell in NLPHL
Classic Hodgkin lymphoma
- Immunophenotype
- Age
- Presentation
- Bone Marrow
- Immunophenotype
- positive: CD15, Cd30
- often positive for fascin, IRF4/MUM1, PAX5 (weak), EBV, antigens (LMP-1, EBER1/2)
- negative: CD45, CD20, bcl-6, ALK, EMA
- 10-20% are CD20+
- background lymphs predominantly T cells
- Incidence: bimodal (15-25 years and after age 50)
- Clinical presentation:
- localized LAD
- cervical lymph nodes most often, followed by mediastinum
- spread via contiguous lymphatic sites; noncontiguous spread in LD
- B symptoms
- localized LAD
- Bone marrow
- LD and HIV-associated have highest involvement
- 10% overall
- atypical mononuclear CD30+ cells
Nodular sclerosis HL
- site affected
- micro
- variant
- ISH
- background
- Mediastinum
- Micro
- nodular with bands of sclerosis
- RS cells, Hodgkin cells, and lacunar cells
- lacunar appearance due to formalin fixation artifact
- syncytial NS an aggressive form of CHL that presents at high stage with bulky mediastrinal disease, composed of sheets of RS cells and RS variants; may have necrosis
- 25% EBV positive
- background is mixed
Mixed cellularity HL
- site affected
- age
- associated with
- micro
- ISH
- peripheral nodes
- 25-45 years
- HIV associated
- developing nations
- diffuse proliferation of lymphs, eos, histiocytes, and plasma cells with varying numbers of classic RS cells and mononuclear Hodgkin cells
- 75% EBV positive
Lymphocyte rich CHL
- compared wtih NLPHL
- site affected
- age
- micro
- ISH
- similar NLPHL but has typical immunophenotype of CHL
- peripheral nodes
- 35-55 yo
- Micro
- R-S cells
- Hodgkin cells
- popcorn cells
- 50% EBV positive
Lymphocyte depleted HL
- site affected
- percentage of CHL
- age
- associated with
- micro
- ISH
- prognosis
- retroperitoneum
- <1% of CHL
- 30-40 years
- HIV associated
- Developing nations
- RS cells and variants > 15/HPF
- Pleomorphic cells
- mixed background
- 50% EBV positive
- relatively aggressive
Blast equivalents
- promonocyts in diagnosis of acute monocytic or myelomonocytic leukemia
- promyelocytes in APL
- erythroblasts in pure erythroleukemia
MDS and splenomegaly
Usually splenomegaly is not present in MDS
Secondary MDS caused by
- chemotherapy (alkylating agents)
- associated with 5q or 7q
- radiation
- benzenes
- Fanconi anemia
MDS morphology
- general marrow findings
- blast %
- dispoiesis in erythroid, myeloid, and meg lines
- Marrow is usually hypercellular; sometimes abnormal localization of immature precursors
- blasts < 20%
- dyspoiesis present in at least one cell line
-
erythroid
- PB: anemia, basophilic stippling, poikilocytosis, and macrocytosis
- Marrow: megaloblastoid change and/or nuclear lobation, internuclear bridging, multinuclearity, karyorrhexis, ringed sideroblasts (at least 5 siderosomes surrounding at least 1/3 nucleus), cytoplasmic PAS+, cytoplasmic vacuoles
- Functional: increased susceptibility to complement mediated lysis, increased HbF, abnormal expression of red cell antigens, acquired enzyme defects (e.g., pyruvate kinase deficiency), acquired thalassemia
-
Granulocytic (myeloid)
- PB: neutropenia, abnormal cytoplasmic granulation, or abnormal nuclear segmentation (including pseudo Pelger-Huet anomaly)
- Marrow: megaloblastoid maturation, abnormal cytoplasmic granulation
- Functional: increased susceptibility to bacterial infection
-
Megakaryocytic dyspoiesis:
- PB: thrombocytopenia, variable size, variable granulation
- Marrow: micromegs, multinucleated megs, hypolobated megs
- Functional: abnormal platelet aggregometry
-
erythroid
- Heathly marrow contains dyspoietic cells (<5% of any cell line)
- Dyspoiesis must be >10% in a cell line to diagnose dysplasia
Secondary causes of dyspoietic morphology
- B12 and folate deficiency
- alcohol
- HIV
- lead
- arsenic
- copper deficiency/zinc intoxication (prominent erythroid vacuolization and iron laden plasma cells are clues)
- medications
- INH
- chloramphenicol
- chemo
MDS molecular and cytogenetic findings
- 30-40% of low grade (RA, RARS) have cytogentetic abnormalities
- 70-80% of high grade have abnormalities
- most common is complex karyotype (2 or more clonal abnormalities)
- 2nd most common is isolated 7 or 7q-
- 3rd most common is isolated 5q-
- disproportionately affects elderly women
- anemia, normal to elevated platelets, micromegs in bone marrow
- indolent clinical course
Chronic myelomonocytic leukemia
- features
- types
- molecular
- primary features
- persistent absolute monocytosis (>1 x 109/L)
- marrow dysplasia
- <20% blasts (blasts + promonocytes)
- absence of Philadelphia chromosome
- HSM
- anemia
- thrombocytopenia
- abnormal monocyte morphology
- 2 types
- CMML-1: blasts and promonocytes < 5% in PB and <10% in marrow
- CMML-2: 5-19% in PB , 10-19% in marrow
- Molecular and cytogenetic
- JAK2 mutation in some
- if eosinophilia is present, rearrangement of PDGFRA and PDGFRB should be excuded
Atypical chronic myelogenous leukemia
- neutrophilia
- spectrum of neutrophils, metamyelocytes, myelocytes, and promyelocytes
- marrow dysplasia
- <20% blasts
- absence of Philadelphia chromosome
- most have cytogenetic anomalies, especially +8 or del(20q)
- some have JAK2 mutations
Juvenile myelomonocytic leukemia
- monocytosis and/or granulocytosis
- HSM
- B symptoms
- may have anemia, thrombocytopenia, increased HbF
- may have monosomy 7
- in vitro spontaneous formation of granulocyte macrophage colonies that are hypersensitive to GM-CSF is confirmatory
- nearly 10% of patients have NF-1
Chronic myelogenous leukemia definition
- genetics
- smear
- t(9;22)
- ABL locus at 9 and BCR at 22
- chimeric Bcr-Abl protein with enhanced tyrosine kinase activity
- major breakpoint cluster p210 fusion protein
- uncommonly occurs at mu-BCR breakpoint with p230 fusion protein
- associated with thrombocytosis and more mature leukemic neutrophils
- uncommonly m-BCR breakpoint with p190 fusion protein associated with
- CML with marked monocytosis
- Ph+ ALL
CML chronic phase
- indices
- smear
- marrow
- clinical presentation
- other labs
- Indices
- leukocytosis with neutrophilia, monocytosis, basophilia, eosinophilia
- thrombocytosis common
- neutrophils immature, and myelocyte proportion is high
- marrow
- hypercellular with high M:E ratio and small hypolobated dwarf megs
- mild reticulin fibrosis and thickening of paratrabecular generative cuffs
- splenomegaly
- low leukocyte alkaline phosphatase (LAP) score
- elevated B12
CML accelerated phase is marked by at least on of the following
Marked by at least one of the following:
- progressive basophilia (>20%)
- progressive thrombocytopenia (<100 x 109/L) or thrombocytosis (<1000 x 109/L)
- clonal cytogenetic progression (+8, i17q, +19, 2nd Ph chromosome)
- increasing blasts: > 10% (but less than 20%)
CML blast phase
- >20% blasts in blood or marrow, a tissue infiltrate of blasts (chloroma), or a prominent focal accumulation of blasts in the marrow biopsy (filling an intertrabecular space)
- 70% AML, 30% ALL
- often additional cytogenetic abnormalities
CML prognosis
- Most powerful prognostic factor is response to TKI therapy as measured by RT-PCR
- imatinib resistance present in 5% of cases
- resistance often result of mutations within BCR-ABL gene; tyrosine kinase domain and the P loop
Polycythemia vera
- presentation
- phases
- cause of death
- molecular
- presentation
- HTN
- thrombosis
- pruritis
- plethora
- erythromelalgia
- headache
- splenomegaly
- Phases
- Proliferative (chronic)
- erythrocytosis, sometimes with neutrophilia, basophilia, and/or thrombocytosis
- marrow hypercellular, usually with megakaryocytic hyperplasia; iron decreased
- Spent phase (postpolycythemic myelofibrosis with myeloid metaplasia)
- peripheral myelophthisic pattern, marrow reticulin fibrosis, and extramedullary hematopoiesis
- Proliferative (chronic)
- Cause of death: thrombosis is #1, acute leukemia is #2
- JAK2 mutation
- >90% of PV and over 50% of ET and PMF
- involved in stimulating the STAT pathway
- most common mutation is G to T at nt 1849 resulting in val to phe at codon 617
- 2nd activating mutation within JAK2 exon 12 in some cases
- mutations in MPL is present in some PMF and ET, but are not seen in PV
Essential thrombocythemia
- age
- prognosis
- presentation
- marrow findings
- bimodal ages: 30 and 60
- longest survival of the MPNs with the lowest transformation to acute leukemia
- presents as isolated thrombocytosis
- marrow:
- large, hyperlobated megs that are paratrabecular and display emperipolesis
- iron usually present (helpful to exclude iron deficiency)
Primary myelofibrosis phases
- Cellular phase (prefibrotic)
- anemia, mild leukocytosis, thrombocytosis
- marrow hypercellular
- megs abnormal (aberrantly lobulated with clumped, inky chromatin) in clusters adjacent to sinuses and trabeculae
- Fibrotic phase
- leukoerythroblastic pattern in PB
- marrow is inaspirable
- reticulin fibrosis, intrasinusoidal hematopoiesis
- abnormal clustered megs
Chronic eosinophilic leukemia (CEL)
- gender
- age
- define
- stains
- morphology
- must exclude
- molecular
- Male:female = 9:1
- ages 25-45
- PB eosinophilia (>1.5 x 109/L) with tissue infiltration and damage
- heart
- GI
- lung
- CNS
- eos may be hypogranular, but granules highlighted by cyanide resistant MPO stain
- must exclude allergic reaction, parasitic infection, collagen vascular disease, mastocytosis, other hematolymphoid neoplasms (PDGFRalpha, PDGFRbeta, and FGFR1 rearrangement)
- must have evidence of clonality, such as increased blasts or clonal cytogenetic abnormality; without this the diagnosis is hypereosinophilic syndrome
AML
- most common in what ages?
- presentation
- diagnosis established by
- immunophenotype
- major classification categories
- Most common type of acute leukemia in adults and infants < 1 year of age
- median age 65 years
- Presentation
- leukocytosis or pancytopenia or soft tissue mass (chloroma)
- blasts usually present in PB
- leukocytosis or pancytopenia or soft tissue mass (chloroma)
- Diagnosis
- blasts >20%
- blasts <20% if there is pure erythroleukemia, myeloid sarcoma, or defining genetic abnormalities
- blast count may include promyelocytes in APML or promonocytes in acute monocytic leukemia
- Immunophenotype
- positive: CD13, CD33, HLA-DR, CD34, and CD45 (dim)
- some express CD7 or CD19
- Classfied:
- AML with recurrent genetic abnormalities
- AML arising secondary to therapy
- AML with myelodysplasia related changes
- AML, NOS
AML with t(8;21)
- population
- treatment
- genes involved
- morphology
- prognosis
- immunophenotype
- young adults
- very chemosensitive
- involves AML1 (RUBX1) and ETO (RUNX1T1) genes
- AML1 encodes alpha chain of core binding factor (CBFalpha)
- blasts have azurophilic granularity, sometimes with large granules (pseudo Chidiak Higashi) and Auer rods
- favorable prognosis
- Immunophenotype:
- positive: CD34, CD13, CD33, CD56, HLA-DR, CD19
- high rate of activating KIT mutations in relapsed cases
AML with inv(16) or t(16;16)
M_-like
- involves what genes
- morphology
- indices
- immunophenotype
- population affected
- treatment
- prognosis
- M4-like
- increased/abnormal eosinophils
- involves MYH1 (myosin) and CBFBeta genes
- blasts with myelomonocytic differentiation and abnormal eosinophils
- eos with large granules with alpha napththyl acetate esterase
- usually no eosinophilia in PB
- Immunophenotype:
- positive: CD13, CD33, CD14, CD64, CD11b, HLA-DR, lysozyme, and CD2
- younger adults
- chemosensitive
- favorable prognosis
AML with t(15;17)
- morphology
- presentation
- treatment
- Immunophenotype
- genes involved
- variant translocations
- age
- prognosis
Acute promyelocytic leukemia
- promyelocytes
- cytoplasm varies from intensely granulated to agranular (microgranular variant)
- microgranular variant has occasional Auer rods and is strongly MPO positive
- often have DIC
- respond to tranretinoic acid (ATRA)
- Immunophenotype:
- positive: CD33, CD13, CD15 (DIM)
- negative: HLA-DR and CD34
- t(15;17) results in RARalpha next to PML
- variant translocations: t(11;17) and t(5;17)
- insensitive to ATRA
- middle age
- favorable prognosis
AML with t(9;11)
- population
- genes involved
- M_ -like
- differentiation?
- immunophenotype
- prognosis
- common in children
- MLL anomalies
- monoblastic differentiation (M5-like)
- immunophenotype:
- positive: CD4, CD14, CD64, CD11b, lysozyme
- negative: usually CD34
- intermediate prognosis
AML therapy related
- multilineage dysplasia
- RS
- increased platelets
- erythroid hyperplasia
- Topo II: 11q23 (MLL) or 21q22 (RUNX1)
- Therapy + 5 years
- poor prognosis
t(6;9) AML
- any morphology, especially M4 with basophilia
- DEK/NUP214
- children and adults
- poor prognosis
- immunophenotype:
- positive: CD34, HLA-DR, CD13, CD33
- Tdt +/-
AML with t(1;22)
- megakaryocytic (M7-like)
- RBM15/MKL1
- infants
- intermediate prognosis
- immunophenotype:
- positive: CD13, CD33, CD41, CD61
- negative: CD34, HLA-DR
AML with inv(3) or t(3;3)
- M0, M1, or M7-like
- thrombocytosis
- giant agranular platelets
- RPN1/EVI1
- adults
- poor prognosis
AML, NOS, minimally differentiated
-
Agranular cytoplasm
- <3% blasts stain with SBB, MPO, and NSE
- myeloid differentiation demonstrable only by immunophenotyping (or ultrastructural cytochemical reactions)
- Immunophenotype
- positive: CD13, CD33, CD117, CD34, HLA-DR
- negative: CD14, CD15, CD11b
- Tdt+ in up to 30% of cases
- Poor prognosis
AML, NOS, without maturation
- 3-10% of blasts show maturation (stain with MPO, CAE, or SBB)
- rare Auer rods and/or granulation
- usually express CD34, CD13, CD33, HLA-DR, CD117
- poor prognosis
AML, NOS, with maturation
- maturation in greater than 10% of blasts
- monocytic differentiation in <20% of nonerythroid cells
- cytoplasmic granulation and Auer rods frequent
- rule out t(8;21)
- immunophenotype:
- positive: HLA-DR, CD13, CD33, CD117, CD15
- may or not be CD34 positive
- Variable prognosis
Acute myelomonocytic leukemia
- define
- immunophenotype
- prognosis
- at least 20% of nonerythroids have monocytic differentiation
- at least 20% of nonerythroids have neutrophilic differentiation
- immunophenotype
- positive: CD13, CD33, CD4, CD14, CD64, CD11b
- smaller population may be CD34+
- variable prognosis
Acute monoblastic/monocytic leukemia
- define
- monoblastic versus monocytic leukemia
- immunophenotype
- population
- sites
- prognosis
- monocytic differentiation in over 80% of nonerythroid cells (including monoblasts, promonocytes, and monocytes)
- acute monoblastic leukemia
- >80% of monocytic cells are monoblasts
- acute monocytic leukemia
- <80% monoblasts
- Immunophenotype
- postiive: HLA-DR, CD4, CD14, CD64, CD11b, lysozyme
- variable expression of CD13, CD33, CD117
- variable but usually negative CD34
- younger people
- often have soft tissue infiltration (gingival, CNS)
- poor prognosis
acute erythroid leukemia
- subtypes
- peripheral blood shows
- marrow shows
- immunophenotype
- other category
- prognosis
- 2 subtypes
-
erythroleukemia
- >50% of all nucleated cells are erythroids and >20% of nonerythroids are myeloblasts
-
pure erythroid leukemia (true erythroleukemia, acute erythremic myelosis)
- >80% of all nucleated cells are erythroid precursors; without excess myeloblasts
-
erythroleukemia
- peripheral anemia, not erythrocytosis, with numerous circulating nucleated RBCs
- marrow erythroids dysplastic and megaloblastoid
- erythroid cytoplasm may have vacuoles and PAS positivity (like ALL blasts)
-
Immunophenotype
- Myeloblasts variably positive for CD34, HLA-DR, CD13, CD33, CD117
- Erythroids: HLA-DR, CD34, glycophorin (CD235a), and CD71 (may be aberrantly dim)
- cases wtih >50% erythroids but <20% myeloblasts may be classified as MDS (RAEB)
- poor prognosis
acute megakaryoblastic leukemia (M7)
- define
- associated with
- prognosis
- >50% of blasts megakaryocytic, either by platelet peroxidase (PPO) technique (electron microscopy with staining for peroxidase), or by immunophenotyping (CD41 or CD61)
- associated with
- mediastinal germ cell tumors (Isochromosome 12p)
- often AML and transient myeloproliferative disorders in Down syndrome are often megakaryoblastic
- poor prognosis
Acute leukemia in Down syndrome
- types (when, who, symptoms, immunophenotype)
- genetics
- 1/2 ALL and 1/2 AML
-
DS associated ALL
- generally similar to non-DS ALL
-
DS associated AML
- increased chemosensitivity, particular to MTX
- relatively favorable prognosis
- peaks between 1-5 years of age
- blasts express CD11b and CD13; negative for CD34
-
Transient myeloproliferative disorder (TMD)/transient abnormal myelopoiesis (TAM)
- 10% of neonates with DS
- 1st week of life usually
- may be trisomy 21 mosaic or confined to the clone itself
- marked leukocytosis and HSM
- difficult to distinguish from congenital acute leukemia
- in most cases, complete resolution without therapy
- still at high risk for AML during childhood
- TMD blasts negative for CD11b and CD13, positive for CD34
- somatic mutations in the GATA1 gene in blasts of both TMD and DS associated AML
Congenital acute leukemia
- define
- must be distinguished from
- most common type
- presentation
- FISH abnormality
- arbitrarily defined as an acute leukemia presenting before 4 weeks of age
- must be distinguished from a leukemoid reaction and TMD (need FISH/cytogenetics)
- most commonly myeloblastic (AML)
- vast majority are monocytic/monoblastic
- commonly with leukemia cutis, often described as “blueberry muffin” babies
- 10% have abnormalities of 11q23 (MLL) gene
Mast cell neoplasms
- presentation (sites affected)
- elevated markers
- morphology
- immunophenotype
- molecular
-
systemic mastocytosis
- skin
- spleen
- bone marrow
- GI tract
- elevated
- serum tryptase
- urine N-methylhistamine (NMH)
- urine prostaglandin D2
- histamine (hypereosinophilic states can also increase histamine)
- Morphology
- in marrow, spindled or round cell infiltrates, often with fibrosis and eosinophils
-
Immunophenotype
- positive: LCA, CD11c, CD33, CD43, CD117, FceRI
- unlike benign mast cells, malignant mast cells express CD25 and CD2 with decreased CD117
- CD25 expression correlates with CKIT mutation
-
molecular
- CKIT mutation, most commonly D816V