Neonatal Flashcards
Concerns with neonates?
- Immaturity of organ systems
- ie, myocytes not fully developed
- CO is HR dependent. fixed SV
- immature NM system
- High metabolic rate
- increased O2 consumption and decreased reserve
- Large ratio of body surface area to weight
- Ease of miscalculating a drug dose
- also easy to miscalculate fluids. pay close attention
- use buretrol, on pump etc
- Nominal amounts of air in lines can be catastrophic
- Foramen ovale functionally closed but not permanently closed
- if it opens, any air can cross over and embolize to brain, causing stroke
- very important to eliminate ALL air
- unpredictable response to drugs ie NMB
- very prone to vagal response
How do you calculate post-gestational age?
weeks gestation at birth + current age in weeks
What are some maternal health and genetic factors that can impact fetal life?
When does organogenesis happen? Organ function development? Muscle and fat?
When is extra-uterine life possible?
- Maternal health & genetic factors:
- congenital viral infections,
- exposure to drugs,
- nutritional deficits,
- issues with vascular supply to fetus (eclampsia),
- maternal illness (diabetes, etc.),
- genetic predisposition
-
Organogenesis: 1st trimester; formation within 8 weeks of conception
- Injury or stress: abnormal organogenesis
- Organ function develops in 2nd trimester
- Injury or stress: abnormal functional development of organs
-
Muscle & fat are gained in 3rd trimester
- Injury or stress: smaller organs; reduced muscle or fat mass
-
Extra-uterine life is not possible until ~22-24 weeks
- 22-24 weekers usually have significant neurocognitive impairment
How does the lung develop in the fetus?
- Lung development begins in utero at approximately 4 weeks’ gestation but lungs are functionally immature until nearing term
-
occurs in five stages:
- embryonic,
- pseudoglandular,
- canalicular,
- saccular, and
- alveolar
- growth of the pulmonary parenchyma and surfactant system occurs during the saccular phase occurring from week 24 through week 40 (36 weeks: magic # for surfactant)
- maturation & expansion of alveoli occur during the alveolar period which begins near term & continues to mature through childhood
- 24 mil alveoli at birht, 300 mil by age 8
- surfactant can be adminitered via ETT in premie infant
- maturation & expansion of alveoli occur during the alveolar period which begins near term & continues to mature through childhood
- Alveoli must transition from fluid filled state to air-filled (gas exchanging) parenchyma
What are some respiratory variations in the newborn?
Respiratory system newborn variations:
- Diaphragm is flatter;
-
more compliant chest with cartilaginous ribs;
-
poorly compliant lungs; may see paradoxical breathing;
- paradoxical breathing= inward movement of chest during inspiration
-
poorly compliant lungs; may see paradoxical breathing;
- predominantly nose breathers until 4 weeks of age;
- chest circumference very close in size to head circumference at birth
What is persistent fetal circulation?
What are some precipitating conditions?
Treatment?
Also called Persistent Pulmonary Hypertension of the Newborn
- PA pressures abnormally elevated causing the ductus arteriosus & foramen ovale to remain open (or re-open):
- leads to hypoxia due to R to L shunting
- Hypoxia & acidosis with concurrent inflammatory mediators are primary causes
-
Precipitating conditions:
- severe birth asphyxia,
- meconium aspiration,
- sepsis,
- congenital diaphragmatic hernia,
- mom’s use of NSAIDS,
- idiopathic
- Response to treatment is unpredicatable
- Initial tx: provide optimal oxygenation
- (PaO2 60-100,
- correct stressors like hypoglycemia or polycythemia
- Other tx: surfactant, inhaled nitric oxide, HFOV, ECMO
- inhaled nitric oxide only FDA approved treatment
What is a newborn? neonet?
General categories for infants?
What is preterm?
Low birth weight? Extremoly low gestational age?
What are preterms more at risk for?
- “Newborn”- 1st 24 hours
- Neonate: Birth to 30 days
- General categories: small for gestational age (SGA), appropriate for gestational age (AGA), large for gestational age (LGA)
- Weight, height, & head circumference are tracked for growth- SGA’s & LGA’s are more likely to have problems
-
Preterm <37 weeks
- <2500 grams: low birth weight
- Extremely low gestational age (ELGAN): 23-27 weeks gestation; all organs immature; most vulnerable Peds patient
-
All preterms have potential for:
- Respiratory distress,
- apnea,
- hypoglycemia,
- electrolyte disturbances (▼Mg++, Ca++) i
- infection,
- hyperbilirubinemia,
- polycythemia,
- thrombocytopenia
What is normal gestation?
Postmature?
- Normal gestation: 37-42 weeks
- All gestational ages have risk for →
- congenital anomalies,
- viral infection,
- perinatal depression,
- fetal alcohol syndrome
- All gestational ages have risk for →
- Postmature > 42 weeks
- Risks:
- irth trauma if large for gestational age (LGA)
- hypoglycemia (esp. if mom diabetic)
- meconium aspiration
- hyperbilirubinemia
What should you always evaluate about perinatal history?
Always evaluate perinatal history:
- gestational age & size at birth;
- maternal infections,
- eclampsia,
- diabetes, or drug abuse;
- prolonged or traumatic labor;
- NICU/ intubation following delivery
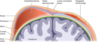
Major key points to fetal circulation?
What is pre-ductal, post-ductal?
Where is the most oxygenated blood delivered?
- (high o2 blood) Placenta → Umbilical vein (high pressure if contraction occurring)→ ductus venosus (DV) *high intrahepatic pressure* → most blood gets shunted away from liver → IVC (most blood)→ RA….
-
PREDUCTAL Circulation (Parallel circulation): IVC→ RA (high rate of flow) → Foramen Ovale (FO)→ LA (high O2 []) → LV → aorta
-
HIGH O2 blood to head, neck, and RUE drained into SVC = then MIXED (high O2-RA→ FO→ LA→ LV)
- Less oxygenated than blood that went straight to head, neck, arms
-
HIGH O2 blood to head, neck, and RUE drained into SVC = then MIXED (high O2-RA→ FO→ LA→ LV)
-
Postductal Circulation: If stayed in RA → RV → pulmonary artery *high pulm resistance* (only 12% [10-15%] blood goes to lungs) → ductus arteriosus (DA) (~85% blood from RV) → aorta → goes systemic circulation (MIXED BLOOD)
- Ductus arteriosus- keeps lungs from being overloaded by blood
OVERALL:
-
Pre-ductal: More oxygenated blood going to head, neck, RUE
- From IVC → RA → LA→LV→Aorta→ head, neck, RUE → SVC
-
Post-ductal: More deoxygenated blood going to system circulation from DA!
- Liver, kidney, lower extremities
- High pulmonary vascular resistance and low systemic circulatory resistance
- Minimal intrauterine pulmonary blood flow: only ~10% of the cardiac output
What CV changes occur at birth to transition from fetal to adult circulation, and why do these changes occur?
Changes that allow parallel circulation of the fetus to convert to the series circulation of the adult:
-
Pulmonary Vascular Resistance DECREASES
- 1st breath → expansion of lung → pulm vascular resistance DROPS → increased alveolar O2 → increase in pH
- neurohumoral mediators and nitric oxide (NO) relaxes pulmonary vasoconstriction.
-
FO closes
- When placenta separates from uterine wall:
- placental BV constrict
- SVR & left ventricular afterload increase.
-
Decrease PVR + increase SVR → increases left atrial pressure above right atrial pressure
- Pressure: LA > RA → functionally closes FO “flap valve”
- FO not close anatomically for months to years (if ever)
- Patent in ~15% adults.
- Pressure: LA > RA → functionally closes FO “flap valve”
-
Decrease PVR + increase SVR → increases left atrial pressure above right atrial pressure
- When placenta separates from uterine wall:
-
Ductus Arteriosus closes
- decrease PVR causes flow through the ductus arteriosus to reverse.
- This exposes the ductus to oxygenated systemic arterial blood + rapid decrease prostaglandin E 2 (PGE2) after birth → closes ductus arteriosus
- Anatomic closure of the ductus requires several weeks.
- D/t Increase PaO2 exposure >60 mm Hg → cause vasoconstriction → functional closure of ductus arteriosus
- decrease PVR causes flow through the ductus arteriosus to reverse.
-
Ductus Venosus Closes
- The ductus venosus closes passively with removal of the placental circulation and readjustment of portal pressure relative to inferior vena cava pressure.
- There is a further gradual decline in PVR secondary to structural remodeling of the muscular layer of the pulmonary blood vessels. During fetal life, the central pulmonary vascular bed has a relatively thick muscle layer.
- After birth, the muscle coat thins and extends to the periphery of the lung, a process that takes months to years to complete
- Expansion of the lungs at birth decreases pulmonary vascular resistance, and the entire right ventricular output is diverted to the lungs
**Overall: Increase SVR + decrease PVR → functional closure of PFO & ductus arteriosus (blood not being oxygenated by lung is NOW going through lungs to be oxygenated) **
What happens to fetal ciruclation of adeuqate ventilation/oxygenation are not established at delivery?
-
Fetal circulatory pattern persists →
- increased PVR
- decreased pulm blood flow
- Ductus arteriosus & FO remain OPEN
- Result: Large R → L intracardiac shunt of desaturated blood to periphery
- Consequences:
- Arterial hypoxemia
- Acidosis
- Consequences:
- Result: Large R → L intracardiac shunt of desaturated blood to periphery
What might cause an infant to have persistent fetal ciruclation in the early weeks of life?
-
Period of vulnerability:
- Hypoxia (acidosis)
- Hypercapnia (acidosis)
- Hypothermia
- Infection
- Prematurity
- Preterm infants: ductus arteriosus may remain open for several weeks & can cause hemodynamic instability
- tx: prostaglandin inhibitor (indomethacin)
- surgical ligation
- ex: if see sudden hypoxia < 10 days old → suspect flip flow circulation occurring
- tx: hyperventilate & hyperoxygenate – difficult to correct
- ex: if see sudden hypoxia < 10 days old → suspect flip flow circulation occurring
- Phenomenon leads to sudden increases in pulmonary artery pressure and shunting of blood past the lungs through a patent foramen ovale or the ductus arteriosus, which may reopen, particularly during the first 10 days of life
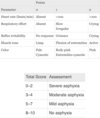
What are the components that make up APGAR scoring? What is the significance of APGAR socring?
APGAR scoring:
- five signs measured/observed in neonates 1 minute & 5 minutes after delivery
- PREDICTIVE on neonatal distress and need for intervention
- Components:
-
Most important:
- heart rate
- HR < 100 bpm: signifies arterial hypoxemia
- quality of respiratory effort
- heart rate
-
Least informative:
- color –
- healthy neonates have acrocyanosis @ 1 min from cold ambient temps (peripheral vasoconstriction)
- Persistent cyanosis- acidosis and pulm vasoconstriction most likely causes
- color –
-
Most important:
- Scores 3–7: Mild to moderately depressed function
- may respond to oxygen administration by face mask
- with or without positive pressure ventilation
- Score < 3: CONCERN
- consult NRP algorithm
Score 0-10
What are some essentials to the newborn resuscitation program (NRP)
Initial actions for newborn in distress:
- Clear infant airway
- Warm/dry them
- Stimulate
- Position- sniffing
- Evaluate: HR, respirations, color
- Ex: labored breathing and persistent cyanosis- suction
- HR < 100 bpm- assist w/ PPV
- HR < 60: intubate, PPV, chest compressions
- O2 & chest compressions not effective → IV Epi

When taking care of a neonatal patient, what are some questions to ask preoperatively?
- Birth history:
- Mom received prenatal care? Maternal infections? Gestational diabetes or chronic health disease? Maternal substance abuse?
- How many weeks gestation? Birth weight? Birth complications? Birth trauma?
- Admitted to newborn intensive care unit? Length of stay?
- Any episodes of apnea or tachypnea?
- Need for oxygen? Need for ventilation? For how long? Discharged to home on a ventilator/on oxygen?
- Infant discharged home on any medications?
- Assess for passage of meconium & urination
Essential assessment of the newborn/neonate?
-
Accurate weight critical
- Unclothed/undiapered
-
Essentials:
- Assessment of overall appearance
- skin color
- breathing pattern
- degree of alertness
-
Color: assess mucous membranes
- acrocyanosis: cool and cyanotic hands and feet
- normal finding in healthy infants
- d/t immature peripheral vasomotor tone
- central cyanosis: needs investigation
- not normal
- jaundice- hyperbilirubinemia
- acrocyanosis: cool and cyanotic hands and feet
Airway assessment in newborn
- assess mucous membranes;
- look at tongue size/ mobility- look at frenulum of tongue (impact feeding);
- a short tight lingual fenulum attached to inferior tip of tongue may impede movement of tongue and breastfeeding
- evaluate chin (retrognathia?- diff intubate);
- nasal patency/ discharge;
- intact hard and soft palate?;
- presence of natal teeth (< 1 mo old- fall out easily)?
- teeth that erupt in first month of life, typically central incisors
- similar to normal teeth but lack developed root system and may fall out
- no indication for removal unless concern for aspiration or interference with feeding
- unrestricted neck movement
- congenital torticollis- means that a baby is born with an odd position of the neck. The odd position is because of a tight, short neck muscle
Heart and lung assessment in newborn/neonate?
- assess for tachypnea, flaring grunting, retractions
- respirations may be “regularly irregular” with pauses (pauses should not last >20 seconds)
- Periodic breathing: more common in infants, particularly preterm infants; probably due to inadequate development of the medullary respiratory centers
- Assess length of pause
- assess clavicles
- Clavicular fractures are a common birth injury occurring in 0.2%–3.5% of births. Usually left untreated
- assess upper & lower extremity pulses
- risk of CHD- impact perfusion to extremities
- Murmurs common in newborns
- Systolic murmur- not as concerning
- Diastolic murmur – concerning!!
- PDA: murmur best heard along the left lower sternal border
Neuro and musculoskeletal assessment in newborn/neonate
- Neuro assessment:
- Posture,
- muscle tone,
- movement,
- seizure activity;
- head control,
- quality of cry;
- response to light and sound;
- fontanelles (Anterior and posterior)
- Back: Spinal contour; presence of cysts, sinuses, dimples, tufts of hair
- ·Musculoskeletal:
- Normal: Inward flexion resting position of upper and lower extremities
- Abnormal: rigidity or extension
*
Relevant labs for newborn?
o point-of-care glucose testing
o complete blood count or hematocrit
o blood type
o Coombs
o bilirubin
Blood and fluid requirement for newborn/neonate?
- Amount of insensible water losses are inversely proportional to gestational age
- Ex: younger pt → more insensible loses we have to account for
- Reasons:
- higher skin permeability
- higher ratio of body surface area to weight
- higher metabolic demand
- radiant warmers and phototherapy increase insensible losses** = more volume deficit!
- Reasons:
- Ex: younger pt → more insensible loses we have to account for
- Neonatal kidneys are unable to excrete large amounts of excess water or electrolytes
-
newborn daily fluid requirement: 70ml/kg/day
- gradually increases throughout 1st wk
- generally started w/ 10% glucose to prevent hypoglycemia for 1st wks of life (if going to surgery)
-
newborn daily fluid requirement: 70ml/kg/day
Considerations for fluid and blood requirement?
- Hct < 30% → risk of apnea higher (neonates and preterm infants)
- Optimize Hct to decrease postop apnea
- Crossmatching not always needed
- Weak expression of ABO antigens at birth
- Transfused blood has higher levels of hemoglobin A → (better release of oxygen to tissues)
- Better release of O2 than FetalHgb provides
- Transfusion associated graft-versus-host risk:
- **Use leukoreduced, irradiated blood is preferred (radiation destroys lymphocytes)
- Ionized hypocalcemia risk (esp w/ FFP administration in neonates- see in any blood products)
- decreased ability to mobilize calcium and metabolize citrate → depresses CV function
- monitor ionized calcium and prepare to replace
Considerations for venous access in newborn?
Peripheral access: can often be obtained once resuscitated
- Common sites: dorsum of the hand, antecubital fossa, dorsum of foot, and scalp (very common in neonates/ small infants)
- Venous cutdown may be needed in difficult access (common site is saphenous)
- cutdowns are avoided (try ultrasound first)
- Venous cutdown may be needed in difficult access (common site is saphenous)
Central lines: common sites are internal jugular, subclavian, or femoral line
- PICC lines placed in the axillary vein have low rates of complications
- IO access is preferred in urgent situations as central venous access can be time consuming
Umbilical vein: may be used in newborn for vascular access
- A small amount of the cord is cut and then umbilical tape is applied to stop the bleeding
- one large, thin-walled umbilical vein and two smaller, thick-walled arteries can be seen and are catheterized with sterile technique
- Complications: Infection, bleeding, hemorrhage, perforation of vessel, thrombosis with distal embolization, ischemia or infarction of lower extremities, bowel, or kidney, arrhythmia if catheter is in the heart, air embolus
-
Contraindications umbilical vein:
- omphalocele
- gastroschisis
- peritonitis
-
Considerations umbilical vein use:
- May be patent up to 2 wks after birth- can be used in an emergency
- Potential for accidental placement in portal vein- xray required
Consideraiton with umbilical artery catherization?
-
Umbilical artery cannulation is common in neonates
- Ability to obtain arterial blood and continuously measure arterial BP.
- Tip of catheter location:
- at or just above level of aortic bifurcation
- below the level of renal arteries (L2) (would cause hypoperf of renal arteries)
- When stable → peripheral a-line inserted and umbilical artery catheter should be removed
- Considerations:
- All arterial catheters have the potential to cause distal thromboembolic disease
- Flush gently to prevent cerebral or cardiac emboli
- Considerations:
How do you monitor pre/post ductal ABG in neonate?
What would yous see if ductus arteriosus shunting or foramen ovale shunting are present?
- Differences in A-Lines:
- Preductal ABG- RIGHT radial arterial catheter
-
Postductal ABG: umbilical artery
-
Ex: for pt w/ PDA and pulm HTN
- Pulmonary hypertension: Preductal and postductal oxygenation should be measured to assess right-to-left shunting
-
Ex: for pt w/ PDA and pulm HTN
- ABG Gas:
- Ductus ateriosus shunting suggested if:
- Preductal PaO2 15-20 mm Hg > postductal PaO2
- Foramen Ovale shunting:
- Decreased predicted value of preductal PaO2
- will not produce a gradient compared w/ post ductal PaO2
- Ductus ateriosus shunting suggested if:
- Preductal arterial oxygen saturation (SaO2 ) reflects cerebral oxygenation