Microbes and Immune System Flashcards
(166 cards)
What are 4 life strategies?
Photoautotrophism
- Sunlight
- Carbon Dioxide
- Organisms that use this strategy are plants, algae and cyanobaccteria
Photoheterotroph
- Sunlight
- Pre-formed organic compounds
- Purple/green non-sulphur bacteria
Chemoautotroph
- Chemical oxidation
- Carbon dioxide
- Extremophiles
Chemoheterotroph
- Chemical oxidation
- Pre-formed organic compounds
- Humans, animals
Give a brief overview of the Marine environmnet
It’s dominant!
- Covers 2/3 of the surface
- Several km deep
Highly diverse
- Various environments within marine environment
- Habitat to bacteria, fungi and algae
Physical parameters
- Salinity
- temperature
- Pressure
- Nutrients
Describe the different zones within the marine environement
Neritic zone
- Mild temp, low pressure, nutrient rich
- Diverse marine life
- Photosynthetic organisms
Oceanic zone
- Pressure increases with depth
- Chemotrophs
- Not as unstable as once thought

What organisms do the dead sea house due to its salinity?
The Dead Sea
- Microscopic life only
- Photoheterotrophs
- Halophiles
How do halophiles stop the flow of water from low internal salinity?
- Halophiles need to stop flow of water from low internal salinity
- Production of compatible solutes increase internal salinity, preventing outflow of water
- Maintenance of the water-salt balance in halophiles
What are compatible solutes?
Osmoprotectants or compatible solutes are small molecules that act as osmolytes and help organisms survive extreme osmotic stress. Examples include betaines, amino acids, and the sugar trehalose. These molecules accumulate in cells and balance the osmotic difference between the cell’s surroundings and the cytosol.
What are Piezophiles and the different types?
Piezophiles (barophiles) are organisms whose survival and reproduction is optimized to high pressures, such as those in deep sea environments.
Piezotolerant
- Grow at atmospheric pressure but can also tolerate increased pressure.
Piezophile
- Optimal growth above atmospheric pressure.
Extreme piezophile
- Need high pressure for survival. Unable to survive at sea level.

What is the difference between extreme piezophile and piezotolerant membranes?
The membrane of the extreme piezophilic organism is highly unsaturated making it extremely fluid.
As opposed to the membrane of the piezotolerant organisms which have highly saturated membranes making them as rigid as possible.
Why are humans anomolous when it comes to withsatnding high oressures compared to other eukaryotes?
Humans are anomolous because we are not able to withstand high pressures like most other eukaryotes.
Why would extremophiles be found in caves despite them being a relativley stable enviornment?
Extremophiles also inhabit caves and mines which is associated with high level of salts, mineral-rich, extreme temperatures and no light.
How do organisms play a role in shaping mines and caves?
Organisms often play a role in the formation of these structures through:
- Acidification of water, resulting in sculpture of caves
- Changing the composition of rock and precipitate out chemicals:
- Iron/sulphur oxidising minerals
- Produces sulphuric acid
- Removes sulphur from minerals
- Negative pH values!
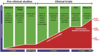
Different tyoes of thermophiles
Psychrophile
- Optimum growth <15ºC
- 90% ocean is <5ºC
- Chlamydomonas nivalis, Listeria monocytogenes
Thermophile
- Spores used as a biological indicator, measuring sterilisation
Hyperthermophile
- Survival at >70ºC
- Not only tolerate, but require for survival
- Thermus aquaticus
Mesophile
- Optimum growth at body temperature
- Human pathogens

How do Psychrophiles and Hyperthermophiles survive their respective environments?
Psychrophiles
- Low temperature, membrane is too solid
- Keep interactive and fluid
- Increase unsaturated fats
Good fat = liquid
Hyperthermophiles
- High temperature, membrane becoming too liquid
- To maintain integrity, solidify fats
- Increase saturated fat content
Bad fat = solid
What are the Oxygen requirements of different organisms?
Aerobes
- Growth in oxygen
- Rhizobium spp - soil
- Neisseria spp
- Meningitis, gonorrhoea
Anaerobes
- Death in oxygen
- Clostridium spp - HAI
- Actinomyces spp – soil
Facultative Anaerobes
- Survive +/- oxygen
- Staphylococcus spp.
- E. coli
Aerotolerant
- Can survive in oxygen but metabolise anaerobically
- Rhizobium spp.
- Streptococcus spp.
Microaerophile
- Prefer reduced oxygen, can’t respire anaerobically
- Lactobacillus spp.
- Campylobacter spp.
What is the Rhizosphere?
Rhizosphere is an area of soil containing a diverse population of microorganisms that utilise plant secretions e.g. proteins and sugars. Microbes consume the minerals and feed them back to the plant, promoting growth
Give a brief overview of P. syringae
- P. syringae allows ice formation at higher temperatures
- Plants normally survive at -2°C to -8°C through internal proteins, changing freezing temp of water
- Bacteria produce ice nucleation active (INA) proteins, increasing freezing temp
- Punctures plants cells, allowing bacteria to penetrate
Define symbiosis, parasitism, mutualism and commensalism.

Hawaiian Bobtail Squid and the Aliivibrio fischeri have a mutualist relationship, describe how this is the case.
The Hawaiian Bobtail Squid provides a selective environment exclusively for A. fischeri. The A. fischeri produce fluorescent light which casts a light shadow from the squid. This is beneficial to the squid because it is nocturnal and the moon above the squid would cause a night shadow to be cast by the squid which would alert predators below of its presence and subsequently kill them. The light from the A. fischeri cancels out the moon shadow and shields the squid from predators.
How does the Hawaiian Bobtail Squid utilise the A. fischeri?
- Light is omitted specifically from the light organ within the mantle of the squid.
- The light organ has epithelial cells which form a ciliated surface on its structure, beating water into the light organ.
- Water passes over tiny, microscopic pores in the light organ.
- A. fischeri accumulates in the deep crypts on the squid.
How does the Hawaiian Bobtail Squid specifically accumalate A. fischeri?
- Water passes through the anterior appendage (ciliated cells) and over the pores.
- Bacteria travel down the light organs and colonise the deep crypts.
- This is where we see specific colonisation of A. fischeri.
How does the the Hawaiian Bobtail Squid specifically allow A. fischeri to colonise?
- Peptidoglycan is a structure specific to bacteria and acts as a signal to epithelial cells.
- Ciliated cells secrete mucus, trapping bacteria from passing freely.
- Squid produces compounds which have an antibiotic effect against Gram +ve
- A. fischeri is Gram –ve
- A. fischeri outcompete other microbes and becomes dominant by activating chitinolytic enzyme within the squid, digesting chitin in the environment.
- Broken down chitin (chitobiose) acts as an attracted for A. fischeri, specifically.
- Acts as an attractant for more A. fischeri to more over the pores.
- Only A. fischeri left, colonising the deep crypts of the squid. A. fischeri becomes non-motile, induces host-epithelial cell swelling and eventually releases light.

Diagram showing the stages of colonisation of a newborn Hawaiian bobtail squid’s deep cysts
- Sterille - The crypts of a newborn squid are sterile within the first 30 min.
- Permissive - Initial mixed bacterial population in the crypt. Mucus is shed to attract bacteria.
- Restrictive - Antibiotic production to inhibit certain types of bacteria. A. fischeri has immunity to these mechanisms.
- Specific - Specific A. fischeri colonisation due to chitobiose secretion

Diagram detailing squid and A. fischeri stages of colonisation

What is the Diel Cycle?
Cycle of colonisation of A. fischeri every day and night in the squid.
DAY
- Nocturnal squid buries in the sand, doesn’t need to omit light.
- Removal of most A. fischeri from the light organ into the environment.
- Remaining bacteria begin to replicate throughout the day, to reach peak density.
NIGHT
- Light organ is full of fresh A. fischeri.
- Bioluminescence enables hunting.
- Removal of bacteria from squid.
Fresh population of A. fischeri generated.
Seeding of the environment with A. fischeri for the next generation of squid.