MI: Antivirals Flashcards
Describe two approaches to antiviral treatment.
- Viral-encoded proteins are a major target (e.g. protease inhibitors) - these are directly-acting antivirals (DAAs)
- Helping the immune system to clear the virus with the use of immunomodulators (e.g. interferon)
How are viral infections normally detected by the immune system?
Viral replication is detected by pattern-recognition receptors which trigger an innate immune response leading to the production of factors (e.g. IFN)
List some limiting factors for antiviral therapy.
- Host immune response
- Adherene to treatment
- Antiviral drug resistance
- Drug toxicity
What is a possible complication of shingles?
Post-herpetic neuralgia
How might shingles present differently in immunocompromised patients?
Multi-dermatomal distribution or invasive disease
What is the main treatment option for VZV infection?
Aciclovir (PO or IV)
Outline the mechnism of action of aciclovir.
- Nucleoside analogue that is incorporated into growing viral DNA and blocks further elongation
- Requires activation by viral thymidine kinase (which is only present in host cells that are infected by the virus)
- Aciclovir has a higher affinity for viral DNA polymerase than host DNA polymerase
What is the prodrug of aciclovir?
Valaciclovir (PO)
What are two 2nd line treatment options for aciclovir-resistant VZV infection?
- Foscarnet
- Cidofovir
NOTE: they inhibit viral DNA synthesis
HSV encephalitis is a medical emergency. How should it be treated?
- IMMEDIATE treatment with IV aciclovir 10 mg/kg TDS without waiting for test results
- If confirmed, treat for 21 days
What is HSV meningitis and how should it be treated?
- Usually self-limiting
- Immunocompromised patients and those who are unwell enough to require hospital admission require treatment
- IV aciclovir for 2-3 days followed by oral aciclovir for 10 days
List some indications for treatment of VZV.
- Chickenpox in adults (high risk of pneumonitis)
- Shingles in adults > 50 years (risk of post-herpetic neuralgia)
- Infection in immunocompromised patients
- Neonatal chickenpox
- If increased risk of complications (e.g. underlying lung disease)

What is CMV?
Opportunistic virus that causes severe disease in immunocompromised patients
In which cells does CMV lie dormant?
Monocyte and dendritic cells
List some consequences of CMV infection in immunocompromised patients.
- Bone marrow suppression
- Retinitis
- Pneumonitis
- Hepatitis
- Colitis
- Encephalitis
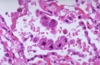
What is a characteristic histological feature of CMV infection?
Owl’s eye inclusion
What is the 1st line treatment option for CMV infection?
Ganciclovir (IV)
How is ganciclovir activated?
Requires activation by viral UL97 kinase enzyme
NOTE: ganciclovir is used in conjunction with IVIG in patients with CMV pneumonitis
What is a major side-effect of ganciclovir?
Bone marrow toxicity
NOTE: therefore, its use is limited in bone marrow transplant patients
What is the pro-drug of ganciclovir?
Valganciclovir (PO)
What is the mechanism of action of foscarnet?
- Non-competitive inhibitors of viral DNA polymerase
- NOTE: foscarnet does NOT require activation
- Tends to be used in CMV infections if ganciclovir is contraindicated
What is a major side-effect of foscarnet?
Nephrotoxicity
What is the mechanism of action of cidofovir?
Competitive inhibitors of viral DNA synthesis (nucleotide analogue)
NOTE: does not require activation
What is a major side-effect of cidofovir?
Nephrotoxicity (requires hydration and probenecid)


