Metabolic bone disorders Flashcards
(38 cards)
What are the two components of bone?
- Osteoid: unmineralised bone (organic component)
- 35%
- Mainly Type I collagen fibres
- Inorganic minergal component
- 65%
- Calcium hydroxyapatite crystals (that fill the space between the collagen fibres)
What is the function of the osteoblasts?
They built boneby synthesising collagen fibres and help in osteoid mineralisation

What is the function of osteoclasts?
They resorb bone and thereby free calcium and phosphate via the release of lysomal enzymes

How do osteoclasts get activated?
They differentiatiate in response to RANKL-Receptor stimmulation of surface
The RANKL is expressed on osteoblasts surfaces–> osteoclasts get activated by osteoblasts!

How to osteoblasts get activated?
Resond to PTH & calcitriol (1,25 (OH)2 vit D)
–> regulate bone formation and absorbtion
What is the cortical part of the bone?
The hard shell of the bone
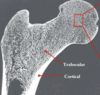
What is the Trabecular part of bone?
spongy, inner part of bone

What is meant by the term “woven” bone
disorganised collagen fibrils, weaker
–> loss of lamellar sturcture

How do you call a bone that is weaker due to unoranised collagen fibres?
Woven bone
What is the normal structure of a bone called?
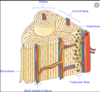
Lamellar pattern of bone :
collagen fibrils laid down in alternating orientations that makes it mechanically strong
What are the direct effects of Vitamine D deficiency on bone?
Inadequate mineralisation of newly formed bone matrix (osteoid)
How does Vitamin D deficiency present in children?
Rickets
- skeletal abnormalities and pain, growth retardation, increased fracture risk
- also affects cartilage and epiphysal growth
What does Vit D deficiency cause in adults?
OSTEOMALACIA
- affects the bone (not the epiphysal)
- skeletal pain, increased fracture risk, proxmyopathy
–> might lead to wabbeling gait and looser zones (in severe deficiency)

What is a looser zone in bone?
Fractures from inadequadly mineralised bone due to normal weight
Explain primary, secondary and tertiary Hyperparathyroidism

How does renal failure lead to vascular calcification?
Because there is reduced excretion of PO4 3-, therefore highter phosphate levels that form insoluble Calcium phosphate plaques

What does renal failure in terms of bone health lead to?
It leads to
- more bone resorbtion (to kepp calcium levels because of VitD deficiency, no Ca2+ can be absorbed)
- Leading to osteitis fibrosa cystica –> hyperparathyroid bone disease
What is osteitis fibrosa cystica?
Hyperparathyroid bone disease
leading to “Brown tumors”– >radiolucent bone lesions due to hight osteoclast activity stimmulated by high PTH to get Ca2+ up
rare now

How do you treat osteitis fibrosa cystica?
Two main issues
- High Phosphate levels
- low phosphate diet
- Phosphate binders – reduce GI phosphate absorption
- Alphacalcitriol
- to restore Vit D levels, decrease bone resorbiton due to low Ca2+
- Parathyroidectomy in 3. hyperparathyroidism
- in hypercalcaemia + hyperparathyroid bone disease
What exactly is osteoporosis?
Loss of bony trabeculae and reduced bone mass leading to weaker bone –> increase risk of fractures

What is BMD?
What does it tell you?
BMD= Bone mineral density
Can be diagnostic of osteoporosis (T-score) if it is = 2.5 below average –>
How is bone mineral density normally measured?
Via and DEXA (Dual Energy X-ray Absorptiometry ) of the femoral neck and lumbar spine
It measures the bone calcium content–> rthe more calcium, the higher the bone mineral density
What are the factors that predispone you to osteoporosis?
- Post-menopausal hormone deficiency (oestrogen is protective)
- Age-related changes in bone homeostasis (osteoclast senescence)
- Hypogonadism in young women and in men
- Different endocrine conditons
- Latrogenic
- heparin
- prolonged glucosteriods
What are latrogenic conditions?
Diseases that are caused by medical care





