MB14 Obstetric and Perinatal Infections Flashcards
Learning Outcomes (for general perusal)
Be able to describe
•Immune factors which play a role in susceptibility to infection in pregnancy.
•Targets of the antenatal infectious diseases screening programme.
•Important bacterial and viral causes of congenital and perinatal infection.
•Choosing which specimens to test
•Contact with a rash in pregnancy
- rubella and parvovirus B19 and VZV
Why is immune tolerance a vital component of pregnancy?
What does the placenta act as?
Fetus and placenta are allografts (NON-SELF)
An immunological barrier

Placenta
How does it act as an immunological barrer?
- Reduced expression of class 1 MHC antigens on placental cells
- Syncytium blocks transit of immune cells
- Inhibition of T cells
Maternal Immune System During Pregnancy
- In which cells are there changes?
- What are the consequences of these changes for disease?
- What would happen if the maternal immune system was fully functional?
- Less Th1 and NK cells
- –increased likelihood of severe symptomatic poliovirus or hepatitis A virus
–Rheumatoid arthritis often ameliorates
–systemic lupus erythematosus can flare up.
- ‘Graft’ rejection
Fetal Immune System
- When are fetal IgM and IgA antibodies first produced in significant amounts?
- Which antibody synthesis is lacking?
- What is absent?
- The second half of pregnancy
- fetal IgG antibody synthesis
- Fetal CMI (cell mediated immunity)
Name the infections that are more severe in pregancy
Effects on mother and foetus
Malaria
Inflluenza
UTI
Candidiasis (thrush)
Listeriosis
Varicella (VZosterVirus)
Mother to Baby Transmission
- Define INTERUTERINE infection
- Define PERINATAL transmission
- During pregnancy
- During birth
Congenital infections
- Name congential infections acquired by ntrauterine transmission (via placenta)
- Name congential infections passed by perinatal transmission
- –Rubella
–Parvovirus B19
–CMV
–Syphilis (Treponema palidum)
–Toxoplasma gondii
–Varicella zoster virus
- –HIV (very occasional intrauterine transmission)
–HBV
–Group B streptococci
–Listeria monocytogenes (can also be intrauterine)
- –Chlamydia trachomatis*
- –Neisseria gonorrhoeae*
What are the categories of motor to baby infection by Transmission, and give examples
Intra-uterine
Rubella, CMV, Toxoplasma
Peri-natal
HIV HSV
Post-Natal
HTLV - human T-lymphotropic virus (breast milk)
Rubella
- What is the incubation period?
- What are the symptoms?
- Why is it rare in the UK?
- 14-21 days
- mild disease - fever, malaise, irregular maculopapular rash which lasts 3 days. Lymph nodes behind the ear, arthralgia. Infection is commonly subclinical.
- Part of MMR vaccination - live attentuated vaccine
Congenital Rubella Syndrome
- When does this occur?
- What do the infected children suffer from?
- Why is the child very infectious for several months?

- Maternal infection
- ~ 80% suffer from sensorineural deafness.
~ 25% develop insulin-dependent diabetes mellitus later in life
Cataracts, brain and heart problems
- infant sheds virus into the throat and urine for many months

Erythrovirus // Parvovirus B19
- What are the symptoms?
- When is there are particular danger in maternal infection of B19? Why?
- Febrile illness in children & maculopapular rash on face, (‘slapped cheek syndrome’), AKA ‘erythema infectiosum’ or ‘fifth disease’. Symptomless infection is common
- weeks 10 – 20. Will cause fetal anaemia, heart failure, hydrops foetalis (swollen macerated foetus), fatal. (Risk about 10%) (B19 as a cause of non-immune hydrops)
- What are the worries when coming into contact with a rash in pregnancy?
- What should be done?
- How can B19 be treated?
- What if rubella is positive?
- Focus is on B19 and rubella
- Take sample of blood from mother, IgG and IgM to both viruses. Looking for immunity AND current infection
If non-immune repeat 4 weeks after contact to check if she has B19. (test for immunity, if not immune, follow up and intervene)
- Intrauterine blood transfusion
- termination options – further tests can help define risk
Case
12 weeks gestation: household contact with slapped cheek syndrome
Developed rash but reassured no action necessary
23 weeks gestation: US – showed fetal hydrops.
Parvovirus B19 IgM positive and PCR positive
2x intrauterine blood transfusion in Glasgow.
25 weeks gestation: showed resolution of ascites but borderline cardiomegaly
35 weeks gestation: emergency CS for premature labour and breech presentation
CMV (Cytomegalovirus)
- How is it diagnosed?
- What are the risks with Maternal infection? How is it diagnosed?
- How can a baby be affected in Congential CMV?
- urine CMV PCR positive at birth
- Reactivation and Primary infection (higher risk). –Serology, seroconversion, using booking blood.
- 1 in 100 babies born with congential CMV
- Spectrum from mild asymptomtic infection to unilateral sensineural deafness, to severe end: CMV INCLUSION DISEASE (liver, spleen, blood, eyes, brain)
Syphilis
- What consequences can maternal infection have?
- What symptoms does the congential syndrome have?
- How is the mother treated?
- miscarriages, premature births, stillbirths, or death of newborn
- Affects teeth, brain, ears, bones, Hepatosplenomegally, jaundice, anaemia
- Penicillin
Toxoplasma gondii
- What is it, where is it from?
- When is infection risky to the foetus?
- Generally, what does it cause?
- Protozoan parasite, undercooked meat and cat faeces
- In all three trimesters of gestation
- Spectrum of symptoms, from aymptommatic to very severe, can be treated with drugs

Varicella – Chickenpox
- When does Congenital Varicella Syndrome occur?
- What will it cause?
- What risks are there to the mother?
- What actions should be taken if a pregnant woman has been exposed to chickenpox?
- What should be done if the mother isn’t immune?
- <20 weeks gestation
- limb deformities, and serious brain & eye abnormalities
- Can cause serious infection: maternal pneumonitis
- Test for immunity (VZV IgG). (90%+ are immune) - But lots of people have no remembered history of chickenpox
- Offer VZIG (Varicella zoster Immunoglobulin)
•Human antibody product IM injection
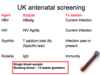
UK Antenatal Screening
Consider the following agents
- HBV
- HIV
- Syphilis
- Rubella
What are their analyte and what can they assess?
- How are these assessed?
- HBsAg - current infection
- HIV Ag/Ab - Current infection
- T Pallidum Total Ab (specific test) - infection past or present
- IgG - Immunity
- Single blood sample (booking blood at 13 weeks gestation)

What are the 4 components of the UK Antenatal Screening program?
HBV, HIV, Syphilis, Rubella
- What does the analyte HBsAG test for?
- What DNA markers are likely to be present?
- What interventions can be taken if this is a positive test?
- How effective are the interventions?
- HBV
- –E antigen positive more likely to transmit
–High DNA more likely to transmit
- HBV vaccine for baby, +/- Specific Immunoglobulin
- (95% of E antigens will transmit mother to baby if no intervention)
- ~100% effective in preventing MTB transmission
- How can HIV be tested?
- What are the interventions?
- How effective are the interventions?
- What follow up will be needed?
- Combined antibody and antigen test, HIV viral load can be tested
- Antiretroviral drugs for mother and baby
Elective caesarean section (unless VL undetectable) and No breast feeding
- No interventions = 25% MTB transmission, this decreases to less than 1% with interventions
- Need to follow up baby regularly with PCR and antibiody – all clear @18months
- What will positive syphilis serology show?
- What are the interventions?
- Anti T. pallidum IgG
- Treat mother with penicillin (possibly baby too)
- Follow up baby - antibody - look for falling levels and eventual disappearance. If congentially infected, then the antibodies will be initially high then fall away
What steps need to be taken if the mother is not immune to Rubella? (Rubella IgG <10 iu/ml)
Offer MMR vaccination AFTER pregnancy
–I.e. To protect next pregnancy


