Malabsorption, Celiac disease, irritable bowel syndrome, IBD, Diverticular Disease Flashcards
What is the hallmark of malabsorption?
Steatorrhea
Malabsorption breadly refers to problems absorbing?
- fat
- fat/water sol. vits
- proteins
- carbs
- lytes
- minerals
- H20 loss
What are the most commonly encountered malabsorption syndromes in th US?
- Pancreatic insufficiency
- Celiac disease
- Crohn Disease
Malabsorption results from disturbance in at least one of the phases of nutrient absorption, which there are four of. What are they?
- Intraluminal digestion
- Terminal digestion
- transepithelial transport
- Transport into lymphatics
Whipple disease blocks nutrient transport into lymphatics, and is a •Chronic, relapsing multisystem illness involving the GI tract (diarrhea, steatorrhea, malabsorption) and distant sites (arthritis, lymphadenopathy).
The disease is characterized by what three symptoms?
What causes whipple disease?
- Disease characterized by weight loss, diarrhea, and polyarthritis; occur together at presentation in 75% of cases
- Gram positive bacillus - Tropheryma whippleii
What population is whipple disease most common in?
How do we treat?
- Usually white males ages 30-49 years (10:1 male predominance)
- Treat successfully with antibiotics
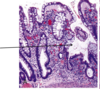
What are the three characteristic symptoms associated with the attached finding of a 40 y/o white male?

Whipple disease - note the distended foamy macrophages in lamina propria that contain T. whippelii.
- weight loss
- diarrhea
- polyarthritis
On inspection you note the distended foamy macrophages in the lamina propria of this image, and you know that this, combined with the patients weight loss, diarrhea and polyarthritis means the patient has?
Which means we are looking at what part of the GI tract that this organism commonly infects?

Whipple disease
small intestine (usually proximal)
What stain have you used to deted these T. whippleii?

PAS-D
Celiac disease is an inflammatory disease of small bowel in genetically susceptible individuals. What are the genetic predispositions identified?
strong association with certain HLA types
- HLA-DQ2
- DQ8
In addition to a genetic predisposition to celiac disease, there must also be an inciting agent exposure. What types of exposures are we talking about here?
- gluten (technically the etoh-soluble gliadin)
- from wheat, barley, oat, rye
What mediates the inflammation in celiac disease?
T-cells: Altered peptides are presented to CD4+ T cells in mucosa, leading to an increase in CD8+ intraepithelial lymphocytes that produce proinflammatory cytokines
Celiac is most common in the following age ranges…
- Adults present usually between the ages of 30-60
- Children present usually between the ages of 6 and 24 months.
What are two conditions in which a patient can have it but not see symptoms?
- Silent
- Latent
What defines a silent celiac disease?
- Positive serology
- Positive villous atrophy
- No symptoms
What defines a latent celiac disease?
- positive serology
- no villous atrophy
- may have symptoms
Celiac disease presents typically with systemic signs of malapsorbtion. What will 10% of these patients also have?
dermatitis herpetiformis
The vague abdominal discomfort and abdominal bloating can lead to a mistaken diagnosis of?
Irritable bowel syndrome
What are two things that celiac disease increases the risk for?
- enteropathy-associated T-cell lymphoma
- small intestine adenocarcinoma
In the past, we referred to a clinical presentation with weight loss, steatorrhea, diarrhea and nutritional deficiency as?
Typical celiac disease
In contrast to typical celiac disease, now atypical celiac disease is more common. What are the ssx associated with atypical celiac disease?
- anemia
- fatigue
- abdominal bloating/discomfort
- osteoporosis
- infertility
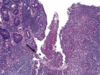
What is shown in each image?

Left: normal mucosa with villi
Right: atrophic mucosa without villi, d/t celiac disease
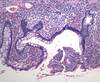
Your patient presents with the attached skin lesions, your tissue sample is shown also. What is this called?
What is causing the lesions?
What condition does this person likely also have?

- Dermatitis herpetiformis is a chronic blistering intensely itchy skin condition, characterised by blisters filled with a watery fluid.
- Deposition of immunoglobulin A (IgA) in upper papillary dermis
- Celiac disease - 15-25% develop this
Tropical sprue is of an unknown etiology and typically affects adults. What is the typical presentation?
- Diarrhea
- soreness of tongue (B deficiency)
- Weight loss
- Steatorrhea
Autoimmune enteropathy is rare, and presents with what two main things?
•Intractable diarrhea and malabsorption associated with circulating gut autoantibodies and a predisposition to autoimmunity
Autoimmune enteropathy affects infants, young children and (rarely) adults evidence suggests a hyperactive immune state due to a defect in?
Regulatory T-cells.
toimmune enteropathy diagnostic criteria includes the presence of chronic diarrhea and malabsorption along with what five other criteria?
- Partial or complete villous blunting
- minimal intraepithelial lymphocytosis
- deep crypt lymphocytosis and apoptotic bodies
- Antienterocyte antibodies
- anti-goblet cell antibodies
Does the absence of antibodies rule out autoimmune enteropathy?
No
Dissacharidase (lactase) deficiency can be either _______________ or __________________.
Congenital or acquired
What is the inheritance pattern of congenital lactase deficiency?
AR
Acquired lactase defiiency is common, particularly among what populations?
Native americans
african americans
In dissacharidase deficiency, incomplete breakdown of lactose leads to what?
Osmotic diarrhea from unabsorbed lactose
•Abetalipoproteinemia is a rare, _______________ disorder, characterized by fat malabsorption.
autosomal recessive
Abetalipoproteinemia is a rare, autosomal recessive disorder, characterized by fat malabsorption, and involves a mutation in what?
What is the consequence of this mutation?
•Mutation in the microsomal triglyceride transfer protein (MTP)
-Failure to assemble and export lipoproteins
What steps should be taken in the treatment of abetalipoproteinemia?
Dietary modification
replacement of fat soluble vitamins
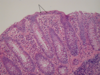
Based on the findings shown here, what is the likely mutation involved in this disease process affecting the small intestine?

Abetalipoproteinemia - microsomal trigylceride transfer protein (MTP) is mutated.
IBS is characterized by the presence of chronic abdominal discomfort or pain associated with changes in bowel habits. In GI practices one third of patients have functional GI disorders, IBS being the most common diagnosis.
What is the cause?
Not known
Peak prevalence of IBS is between 20 and 40 years of age and demonstrates a significant female preponderance. What must you do to make the dx?
Rule out other causes such as enteric infection or IBD
What are the criteria that need to be met for IBS?
At least 3 days/month in the last 3 months associated with 2 or more of the following:
- Improvement with defecation
- Onset associated with a change in frequency of stool
- Onset associated with a change in form (appearance) of stool