Liver Disease in SA Flashcards
Evaluation of the Liver
(3)
- can look at these different aspects and any changes
Enzymes Indicating Hepatocellular Damage
(4)
- these are the classic ones- leakage enzymes
- tell us there is damage to the hepatocytes

Hepatocellular damage - “leakage”
- these enzymes are readily available from the cytosol of the hepatocytes
- if there is damage to hepatocytes and it dies, the enzymes in hte cytoplasm will be released
- or some degree of damage to hepatocyte causes wall to release a little bit of cytoplasmic material
- blebosome: will have a bit of cytoplasmic material in it
- if you even just have a lot of blebbing from a large amount of hepatocytes, will still see an increase of these specific enzymes

Hepatocellular Enzymes: ALT and GLDH
- will increase about 12 hours after injury
- last for about 1-2 days
- more common in SA
large animals: ALT activity is very low!
*

Hepatocellular Enzymes: AST and ALT
- if you have marked muslce damage, you may see increase in AST
- need to differentiate if it is liver damage or liver damage
- CCK can help in this
- (echo)
- need to factor in how specific certain enzymes are to a tissue
Liver vs. Muscle
- CK can be a good indicator of muscle cell damge, but has a very short half life
- so the measurement of this parallel is not full proof

Enzymes Indicating Cholestasis
(2)
- we have lots and lots of hepatocytes, can see increases with little or large damage
- key enzymes of cholestasis: ALP and GGT
*

Alkaline Phosphatase
(ALP)
Derived from bile duct epithelium
- cholestasis will irritate bile duct epithelial cells and this ALP will be released
- but it also comes from other places too (young dogs- bone isoform of ALP) –> need to be aware
- any dog that is stressed or given prednisolone over time will likely have a notable ALP increase (steroid induced isoform)
- in cats it has a VERY short half life, any increase is significant (could be hepatic lipidosis, or if not yellow- hyperthyroidism) –> the dynamic of the changes can be very important in cats
- dogs can get an increase for stress and other things

Induction vs. Leakage
ALP is an induction enzyme: they are present on some of the biliary epithelium but can also have induced production of these enzymes –> trascription and translation induced
- different to the leakage enzymes which are present in the cytoplasm
- may see these enzymes 6 or 7 days later after the induction process occurs and then are released –> ex: steroid induced

Gammaglutamyltransferase (GGT)
- other cholestetic enzyme we look at
- nursing animals will have a high GGT as it is in colostrum
- If renal tubular cells get damaged, they will release this into the urine, BUT NOT THE BLOOD, need to be aware

Measures of Hepatic Function
(7)
- key enzymes
- leakage: dmaage to hepatocytes
- cholestasis: blockage present
- these are generally on biochem panel
- these are measure of liver FUNCTION where as other enzymes show damage
- can have damage but the functional capacity of the liver is rather large
- damage and function of the hepatocyte does not have to coincide but can also go hand in hand

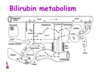
Bilirubin Metabolism
- we have a regular turnover of RBC’s (110 days) and we want to conserve ironand conserve Hb –>happening in spleen
- bilirubin is not solube in water- trafficked using albumin
- conjugated in the hepatocyte –> makes it water soluble (can then float in fluid without carrier)
- conjugated bilrubin will be converted urobilin or stercobilin or can be excreted in the urine
- WATCH THE VIDEO
Bilirubin

Bilirubinemia- Hemolysis
- if you have excess break down of RBC’s
- the hepatocytes can only conjugate so much
- the key limiting step though is the EXCRETION INTO THE BILE
- there will be back up into the system, you will start to leak out the conjugated bilirubin which is soluble and you will see it being released in urine

Bilirubinemia - Cholestasis
- Break down of RBCs is normal, the hepatocytes will conjugate the bilirubin
- there is blockage: bilirubin in the blood and in the urine
Bilirubinuria
Ammonia and Urea
(what is ammonia converted into?)
- when you eat a proteinaceous meal, there is ammonia present and will be detoxified in the liver into urea (still toxic but not as toxic) and then can excrete urea into the kidneys
- If you have a filing liver, you will have a decrease in urea in the blood
- ammonium will increase

Ammonia and Urea
(role of urea and what is seen in hepatic disease?)
- bilirubin will increase in the blood if the liver is failing because the liver cant process it and get it into the biliary ducts
*
Glucose
- If the liver is fialing you may see a decrease in glucose as the liver cant synthesize it
- but glucose is so important that this is not an early sign as it is conserved until desparate
- failing liver–> would see decrease in albumin

Cholesterol
(synthesis and increase/decrease)

Cholesterol
- If the liver fails to build cholesterol, it will go down in the blood
- If there is blockage there may be an increase
- or you can have both happening and not really see a change (could still be liver failure)
- essentially cholesterol levels are not PARTICULARLY helpful
- post prandial- post meal (be aware of cholesterol increase there)
*

BIle Acids
- echo
- why do we need bile acids? emulsify fat in digestion, need to have it coming into the gut
- liver builds bile acids and excretes into bile ducts, but it is expensive to build bile acid!
- NEED TO RECYCLE
once bile does its job, it is reabsorbed by portal vein and is taken up by hepatocytes to be excreted again - in healthy animal: should see bile acids in duct or bile
- but shouldnt see in circulation!
BIle Acid Concentration [BA]
- want to feed the animal after initial reading
- will cause the gall bladder to contract, can see if the liver is not uptaking the bile acid correctly

increase [BA] in serum or plasma
- either a decrease in clearance from portal blood or lower excretion via bile
- portosystemic shunt: abnormal vessel that connects the portal blood to a vessel –> can be congenital or acquired (hepatocytes are functioning well but the blood might be channeled away from the hepatocyte)
- Obstructive cholestasis: bile acids cannot be excreted (backed up toilet effect)
- If bilirubin is high due to cholestasis then you know bile acids are high, but only do the bile acid test when necessary (if they arent really icteric)

Bile Acid Challenge Test
*

Ammonium (NH4+) concentration
- we are going to have ammonium in the intestine and ideally want to channel to hepatocyte and then be excreted

Ammonium Concentration
(analytical concepts and samples)
- not really a good thing to sample and it is very unstable
- needs to be on ice and analyzed in 30 min
- cant have smoke or sweat on hands as it may increase levels in the sample

Hyperammonemia
- ammonia can have access to large circulation
- or can have a post prandial increase after meal (protein)

Other lab findings to consider - CBC
(Acanthocytosis, Anemia, Codocytosis, Microcytosis)

Other lab findings to consider - UA

Other lab findings to consider -others
(PTT or PT, Fecal Exam Results, Peritoneal Fluid analysis)
- all of the COAGUALTION ENZYMES are built in the liver- can be another way to indicate the liver

Liver
(diagnosing a lesion)
- what causes the damage? - you will need to do imaging
- aspirate
- biopsy
- gives a more morphological idea of what is happening


- portal triad=P
- C= central vein
- hexagon = liver lobule
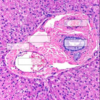


- PSS

Neurological signs in a case of Liver Failure


NUTMEG LIVER
- can be caused by RHS heart failure by venous congestion
Describe the lesion

- orange/yellow color
- capsular
- swollen
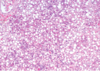
fatty liver

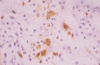
- Immunochemistry or Immunohistology
- immunoperoxidase to demonstrate cells containing viral antigen

Equine Herpes Virus

- Multifocal haemorrhage

- Intracellular viral inclusion body
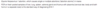
Describe the lesion

- white
- multifocal
- encapsulated
- distributed throughout parenchyma

- neutrophils


- malignant
- secondary
- haemangiosarcoma

Why would pancreatic hypoplasia lead to emaciation?