Lecture 7: Hormonal Properties Flashcards
(130 cards)
What are the 3 hormone derivatives of isoprene/cholesterol?
- Steroids 2. Vitamin D 3. Retinoids
Are the 3 hormone derivatives of isoprene/cholesterol lipid or water soluble? Do they require carrier proteins?
Lipid Yes!
Where are the receptors of the 3 hormone derivatives of isoprene/cholesterol?
Intracellular
Are thyroid hormones lipid or water soluble?
Partially lipid soluble
Do the thyroid hormones require carrier proteins in the blood? To get through membrane?
Yes
Yes because only partially lipid soluble
Where are the receptors of thyroid hormones?
Nuclear
Do protein and peptide hormones require carrier proteins?
No
Where are the receptors of protein and peptide hormones?
Membrane
Do AA derivative hormones require carrier proteins?
No
Where are the receptors of AA derivative hormones?
Membrane
Are eicosanoid hormones lipid or water soluble?
Lipid
Do eicosanoid hormones require carrier proteins?
Yes
Where are the receptors of eicosanoid hormones?
Membrane (G-protein) and intracellular
How many Cs in androgens (including testosterone)?
19
How many Cs in estrogen?
18
Are estrogens aromatic of aliphatic?
Aromatic
Are androgens aromatic of aliphatic?
Aliphatic
What are the 5 classes of steroid hormones and what does each include?
- Androgens: DHEA and testosterone
- Estrogens: estradiol, estrone, estriol
- Glucocorticoids: cortisol, corticosterone
- Mineralcorticoids: aldosterone, deoxycorticosterone
- Progestins: progesterone
What 3 steroid hormones have 21 Cs?
- Cortisol 2. Aldosterone 3. Progesterone
What is specificity due to in steroid hormones?
The position of the hydrozy group on the ring structure
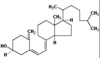
What is the ring structure of steroid hormones?
- Three 6-membered rings
- One 5-membered ring
What is this?

Progesterone
What is this?

Cortisol
What is this?

Estadiol