Lecture 4 - Ventilation/Alveolar gases Flashcards
What is the function of ventilation?
Delivers O2 and removes CO2 that is exchanged across the respiratory membrane.
What is defined as the work of breathing?
Elastic recoil in lung (and chest wall) to change volume
AND
Airways resistance (friction) to get airflow
So we need to overcome the elastic recoil of the lung, and the resistance of the airways.
What is the elastic recoil of the lungs?
And what factors affect this?
The elastic recoil can also be called compliance.
Compliance is a measure of the elastic properties (“stiffness”) of the lung.
Compliance varies with:
- Lung volume - as the lung gets larger it’s harder to stretch
- Age - lungs are more compliant with age (but chest wall is stiff, and the resp. muscles are weaker - decreased VC)
- Alveolar surface tension - depends on surfactant (surface tension of water molecules constitutes 2/3rds of effort to expand the lung).
Describe what factors affect airways resistance (physics), and is air flow laminar during quiet breathing?

Why are the bronchi the main site of airways resistance?
Since there is a reduced cross sectional area
In relation to diameter, what physiological factors determine airway resistance?
Bronchoconstriction: can be caused by activity in vagal parasympatetic fibers (reflex from stimulating irritant and cough receptors in airways). Or caused by local mediators (histamine, leukotrienes)
Bronchodilation: Activation of B2-adrenoreceptors via circulating adrenaline or administration of sympathomimetics (e.g. isoprenaline and salbutamol)
Dynamic Compression of airways: when we breath out really hard we can close off airways
When does dynamic compression of airways limit airflow?
And how to patients counteract this?
Limits air flow in subjects during a forced expiration.
Counteract with “purse-lipped breathing” - maintain airway pressure with “splints” airway open
What happens to the work of breathing in restrictive lung disease, obstructive lung disease and pulmonary oedema?
Restrictive: There is an increased work due to decreased lung compliance
Obstructive lung disease: Increased work due to increase in airways resistance
Pulmonary oedema: Increased work due to decreased lung compliance
What does the work of breathing equate to?
Work of breathing is pretty much change in intrapleural pressure.
A fall in intrapleural pressure during inspiratio equates with WORK done to move air.
Descibe the dashed line (1, 2) and the curved line (1, 2, 3)
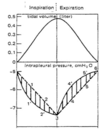
Line 1, 2 is when the work of breathing includes only the compliance of the lungs. The graph becomes non-linear when air ways resistance also needs to be overcome.
What do pressure volume loops give us an indication of?
Give us an idea of work of breathing.
The slope of line AC indicates amount of lung compliance, and width of loop is proportional to airway resistance.

Describe this

When we inspire we have to do work of breathing, which is the energy require to overcome the compliance of the lungs and the airways resistance - this work is represented by the entire figure. AECDA is the energy stored in the elastic tissue in the lungs (ABCA not included since you can’t store energy thats required to overcome airways resistance).
AECFA is the work of respiration, and since this fits with AECDA expiration is a passive process, since work is done by energy stored in stretched lung tissue.
We only have to overcome airways resistance as exhaling, the energy for this is from elastic recoil.
Why is the width of this pressure volume loop wider in this patient with asthma?

The width of the circle is proportional to the airways resistance - we do the extra work to overcome this extra resistance by using secondary respiratory muscles

What is the typical O2 consumption?
And CO2 production?
O2 consumption: 250-300ml/min
CO2 Production: 200-250ml/min
Need to exchange these across the alveolar membrane to maintain homeostasis, and needs to be able to increase during exercise (Due to increases O2 consumption and CO2 production).
What is the respiratory exchange ratio?
VCO2/VO2
200/250 = 0.8 (depends on diet)
Gas exchange is driven by what?
Partial pressure gradients of PAO2 and PACO2
These set the alveolar ‘end’ of the partial pressure gradient.
What are the partial pressures “PAO2 and PACO2 determined by?
- Composition of inspired air
- Alveolar ventilation
- O2 consumption or CO2 production
- Matching of alvolar ventilation to pulmonary capillary blood flow

How can we use PACO2 to calculate alveolar ventilation
Assume VCO2 = 200ml/min @ resting metabolism
863 factor corrects for pressures and allows for combination of volume and pressure values
shows that VA in inversely proportional to PACO2

How can we calculate PAO2
“the alveolar gas equation”
the typical PiO2 si 150mmHg

What use does measuring PAO2 and PaO2 have?
If there is a difference between these two that is too large then it indicates a problem with gas exchange
This difference is the A-a gradient, which is normally <10mmHg
Increased A-a gradient indicates decreased gas exchange (difference between PAO2 and PaO2)

How do you calculate the A-a gradient
Substitute alveolar gas equation, then take away PaO2 to get difference



