Lecture 15: Normal Birth Flashcards
(15 cards)
The parts of labour?
Passage
Passenger
Powers - within normal biological ranges these are the most important.
Challenges in human parturition?
- Quiescence - of uterus with growth, distenseion, pressure
- Timing - for safe birth
- Activation - uterine musclature, changes in uterine tract
- Birth - fetal-neonatal adaptations
- Involution - Haemostasis, establishing lactation
Quiescence?
Uterine muscle contrations poorly synchronised
Low amplitude (<10mmHg) and low frequency - “Braxton-hicks”
Painless with cervix firm and closed
controlled by progesterone from the corpus luteum
How is labour in humans initiated? Drugs that cause this?
Labour is triggered by withdrawal of progesterone block to labour. In humans this is a “functional withdrawal” where the serum level doesn’t really change.
Progesterone reduces prostaglandin F synthesis responsible for Oxytocin. It affects Calcium transport and also increases B adrenergic receptors.
Mifeprestone induces labour at all stages of pregnancy
Activation occurs when? Involves?
Timing - Uncertain process in humans
- 280 days from LPM (37-42weeks)
- 268 days from conception
Involves:
- Intact fetal genome
- Uterine stretch
- fetal HPA axis
- upregulation of myometrium (allows synchronised contraction)
- Melatonin and circadian rhythms
- If membranes rupture prelabour (abnormal)
Contraction associated proteins?
- increase myometrial contration (actin myosin) -clinically antagonised with Ca channel blockers like nifedipine
- Increase myocyte excitability ion channels (Ca2+, voltage gated) -Clinically block with B2 sympathomimetics
- increase intercellular connectivity gap junctions -antagonise with PG synthase inhibitors (COX1 and 2)
PGs and Labour?
Unknown pathway but the final event is an inflammatory event through prostaglandins. Known from the fact the PG can be measured in high levels and are potent inducers of labour.
They increase mypometrial contraction, lead to cervix changes, associated with membrane rupture.
Oxytocin?
- Nonapeptide from post. pituitary and genital tract
- syntocinon is synthetic version
- not essential for initiation
- like PG requires gap junctions to work
- given as primary prevention of PPH
Cervical changes allowing delivery?
The cervix that was firm must “ripen” to allow birth. Cytokines are essential, ECM breaks down and it becomes soft.
Can happen at term when E rises and P falls
Or can happen preterm due to infection (inflamatory process)
Membranes of pregnancy?
Amnion and chorion are a site of PG production and rupture is not essential for labour but rupture will cause a large release of PG resulting in labour most likely.
In the lower segment of the uterus is the zone of altered morphology that has increased receptor levels and thus increased PG synthesis.
The process of birth?
With mature fetus and the right timing:
- Pelvic ligaments soften
- uterus excitability and contractions coordinated
- Cervix becomes soft an easily dilated
- Mambranes may rupture…
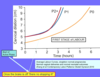
Stages of labour?
- Until full dilation (10cm)
- Contractions, cervical effacement and dilation
- descent of the presenting part
- Spontaneous, normal or premature rupture (SRM, ROM, PROM)
- Full dilation until birth of baby
- From birth until delivery of the placenta
adaptations at birth?
- Closure of the foramen ovale sending 100% RV output through the lungs accompanied by a rapid reduction in pulmonary vascular resistance
- Reduction-closure of ductus arteriosus
- Birth thermogensis: Brown fat - non-shivering thermogenesis
- Sympthetic nervous control
- (dry the baby to help reduce evaporative heat loss)
Feeding of the neonate?
Fetus - had a constant supply of nutrients
BUT
Neonate - Intermittent feeding so a risk of hypoglycaemia
(nb: suckling causes the mothers uterus to contract to reduce risk of bleeding)
Involution?
Placental separation
Cleavage through decidua basalis
Contractions to prevent postpartum haemorrhage (PPH)
Increased uterine sensitivity to oxytocin


