Lecture 11 - Infective Endocarditis Flashcards
What is bacteraemia?
When theres viable bacteria in the blood, and are secondary to an infection/injury at a mucosal site. Bacteraemia is transient, and most of the time is removed by the appropriate localized response.
However disease can occur in a suceptible host: Osteomyelitis, meningitis, endocarditis
What is septicaemia?
Septicaemia is when theirs virulent bacterial and/or bacterial products in the blood. Septicaemia is patholgoical.
There is an innapropriate immune response to the bacteria/bacterila products. It’s unregulated, generalized, intravascular response that is pro-inflammatory.
Septicaemia can cause DIC, embolisms, thrombosis, ischaemia and necrosis.
DIC creates thrombi, which can cause infarcts, ischaemia and then organ faliure.
What are the 5 steps of sepsis?
-
Systemic inflammatory response syndrome (SIRS)
- 2 or more of:
- Hypo/hyperthermia - <36C or >38C
- Tachycardia = HR>90 bpm
- Tachypnoea = RR > 20 bpm
- Increased WBC/immature PMNs
- 2 or more of:
-
Sepsis
- ≥2 SIRS criteria + proven infection
- +ve blood culture/graim stain/PCR
- ≥2 SIRS criteria + proven infection
-
Severe sepsis
-
Sepsis + cardiac dysfunction
- Hypotension & hypoperfusion -> organ dysfunction
-
Sepsis + cardiac dysfunction
-
Septic shock
- Severe sepsis + organ dysfunction despite fluid resuscitation
-
Multi-organ dysfunction syndrome (MODS)
- Organ failuer dure to hypoxia (since they aren’t being perfused - can because they can’t oxygenate their lungs)
- Direct correlation between number of organ systems failed and mortality
What parts of the heart are affected in infective endocarditis?
Infection of heart valves & mural endocardium occurs. Formation of vegetations occurs (thrombotic materal and bacteria), and this can also occur on prosthetic valves, pacemakers etc.
What type of endocarditis acts more quickly? Acute or subacute infective endocarditis
- Acute IE: has a rapid course over days to weeks
- Destruction of previously normal heart valves
- Significant mortality
- Involves virulent pathogens
- Difficult to treat with antimicrobials - need to use surgery
- Subacute IE: has a prolonged course of weeks to months
- Affects previously damaged heart valves
- involves lower virulence organisms than acute IE
- Responds to antimicrobials
What type of bacteria (gram +ve or -ve) causes most IE infections?
>80% infections are gram positive cocci

What are the risks for IEC?
- Age
- >70 yrs
- Sex
- male
- Any sort of prosthetic or artificial valve can increase risk.
- Intravascular device/haemodialysis -> IV catheter/PICC line/CVC (anything that exposes you to a bacteraemia can put you at risk of bacteraemia.
- Immunocomprimised
- Diabetes, cancer, elderly
What are the clinical signs of IEC?
- Fever (in subacute its intermittent, low grade or absent)
- Heart murmur (new/changing murmur)
- Non-specific - e.g. chills, anorexia, arthralgia, dyspnoea, cough, abdominal pain, nausea, vomting, elevated ESR
- Neurological - strokes, intracrainial haemorrhage, microabscesses.
What are the complications of IEC?
- CHF, valve insufficiency, MI
- in ~60% IE patients
- Neurological
- Embolic strokem intracerebral haemorrhage, abscesses
- Septic emboli
- Kidneys, spleen, liver, lungs, skin, brain, gut
- 30% have septic infarcts of spleen & kidneys before diagnosed IE
- Infection
- metastatic -> osteomyelitis, septic arthritis
- Glomerulonephritis - can cause renal failure (due to deposition of antigen antibody complexes in the basement membrane of glomerulus, causing damage to the kidneys)
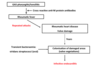
what is the pathogenesis of IEC?
Bacteria bind to platelet receptors, this activates them and upregulates expression of more receptors. fibrinogen binds to platelet integrins, leading to aggregation, which results in a fibrin clot.
This process leads to
- Infected thrombus (vegetation)
- Coagulation (DIC) (sepsis)
- Thrombocytopenia

What is the pathogenesis of subacute endocarditis?
In subacute endocarditis the valve needs to have been previously damaged in order for bacteria to adhere.
There are three mechanisms for subacute endocarditis
- Deposition of platelets/fibrin due to altered haemodynamics can cause nonbacterial thrombotic endocarditis.
- A bacteraemia can lead to there being adhesion of bacterium to the platelet.
- this adhesion can be either direct or via a bridging molecule.
- Formation of infected thrombus causes a vegettion.
- vegetations contain: platelets, fibrin, bacteria and inflammatory cells. These are protected from neutrophils.
Where do vegetative growths form most of the time, and what damage can they cause? (note: this occurs with less virulent bacteria in subacute endocarditis)
They’re most likely to form in the heart valves (mitral or aoritc)
- Bacteria is releasd into the blood stream from the vegetation, this causes bacteraemia and possibly sepsis.
- Micro/macroemboli are also released from the vegetation to give septic emboli.
- These emboli can cause occlusions, which lead to infarction/ischaemia (these are known as a septic infarct)
- The immune complexes formed can deposit in the glomerulus to cause glomerulonephritis

How do virulent bacteria cause acute IEC? e.g. staph aureus.
They bind directly to MSCRAMMS (on cell surface), and bind to SERAMS (which are excreted then re-bind).
The bacteria releases toxins, which causes inflmmation an cell death - this inflammation contributes to heart valve damage.

How does device associated endocarditis occur?
Staph. epidermidis/ staph aureus can cause a bacteraemia, and then cause a biofilm infection on the device.
Anyone with a heart valve or a pacemaker is at an increased risk.

What are diagnoses criteria for IE
- Positive diagnosis:
- 2 major
- 1 major and 3 minor
- 5 minor
- Major criteria include:
- 2-3 positive cultures
- with organisms typical for IE
- 2-3 positive cultures
- Minor criteria include
- PCR, serology -> ~10% cases blood cultures are -ve
- Echocardiogram/CXR/ECG important