Lecture 10 -Immunodiagnostics Flashcards
(19 cards)
What two types of immune response can we measure?
Humoral or cellular
Most tests use humoral
What can we use to measure an antigen and antibody

How can agglutination allow us to detect an antibody
If the antibodies of interest are present they will bind to the antigen, causing them to stick together

How can agglutination allow us to detect antigen?
Instead of a latex bead coated in antigen, there are coated in antibody
And we add these to detect if a particular antigen is present - if it is, agglutination will occur

What are the two types of immuno fluorescence we can use?
Describe each one
Direct immunofluroscnence
- We can either look for presence of antigens, this is done using an antibody with a flurochrome attached.
The cells in the pic above show green since the antibodies are binding
Indirect immunofluroescence
- In indirect immunofluorescence we use an unlabelled antibody that can recognise the antigen (whereas in direct we label the antibody with a flurochrome)
Then a secondary antibody is added which has a flurochrome attached - this can be done to detect auto antibodies
We added the patients serum to a cell line to see if they’ve got antibodies against dsDNA, and if they do the antibody it will bind to the cells nucleus
The secondary antibody that’s specific for human antibodies that has got a flurochrome attached can then bind to them and identify them

What are neutralization assays used for
When we are looking for functional antibodies
Neutralisation blocks the interaction betwen the virus and its receptor on the cell.
we add a smaple to a mammalian cell culture to see if there is a virus present.
Each time a virus infects a cell it kills it, then we can stain the well to see the cells killed by the virus
If there are neutralising antibodies present we can block this interaction and prevent infect
So we can see how many neutralising antibodies are present by seeing how inhibition of cellular death there is

Describe how an enzyme immunoassay is done (ELISA) to detect an antibody
This is the most common method used to measure antibodies/antigen
There is an antigen coated well, we then add serum which contains antibody which binds to the antigen on the well
We then add a secondary antibody (e.g. an antibody which is specific for human IgG) and this has an enzyme attached to it. We can then add a substrate, and when the enzyme cleaves the substrate it causes a colour change and this can be used to detect the presence of antibodies
In the micro-titre plates, the darker colour represents a higher concentration of antibody present

Describe how elisa is done to detect an antigen
We can also do this to detect antigen
We now instead coat the well with a monoclonal antibody against the antigen of interest
We then add the patients serum, and if they’ve got the antigen present it will bind to the antibody which is coating the well.
We can then add an enzyme conjugated antigen-specific antibody which is specific for the antigen, and then we add a substrate. If there is a colour change the antigen is present in the serum, and the greater the colour change the higher the concentration of antigen.

Describe how rapid tests work
The added liquid is drawn across by capillary flow, as it moves it picks up gold coated monoclonal antibodies that bind to the antigen (e.g. we may have an antibody against the p24 antigen, and then we may have another antibody which is specific for p24, and it binds to p24 and captures the gold labelled Ab’s which are bound to the antigen).
There would then be a line of gold present in a positive test.
The control is an anti-IgG antibody, so for it to be a valid test both lines need to be seen.

Describe what a type 1 hypersensitivity reaction is
Immunological reaction characterised by IgE, these antibodies bind to IgE receptors on mast cells, and when an allergen binds to IgE bound to the mast cell this leads to a type 1 hypersensitivity reaction (e.g. asthma, riovitis, some food and drug allergies, anaphylaxis)
We an measure the level of response by measuring specific IgE antibodies against the allergen of interest (e.g IgE against peanut allergen)

Describe what a cell mediated response (type IV hypesensitivity) reaction is?
This is due to the recognition of a peptide antigen that stimulates cytokine production.There is an APC presenting an antigen on MHC I, which is then recognised by the T cell receptor, which then activates the T cell, which then makes cytokines, which then has an effect on macrophages and other T cells.
Can also be seen in various allergies such as contact dermatitis - we can measure this using patch testing.

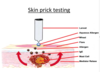
Describe how skin prick testing is done
Use an aqueous solution of the allergen (e.g. if we were looking at an allergy to pollen we would have an aqeous solution of pollen)
- We then use a lancet to prick the upper layers of the skin to introduce the allergen
- If the person is allergic there will be mast cells which are coated in IgE that are specific for that allergen, which can bind that to that allergen and cause the mast cells to degranulate, causing it to release cytokines (inclduing histamine), and this causes vasodilation and the release of fluid
- You get a wheal, which is due to the fluid moving out of the blood vessels and into the extracellular space
- And there is also a flare surrounding it which is an area of redness due to vasodilation
Describe how Type IV hypersensitivity is tested with patch tesing
Test for this with patch testing rather than using a lancet
Apply the various compounds that they may be allergic to via a patch, then we look for redness and inflammation in the skin
See if its a positive test my measuring diameter in 72 hours

Describe how interferon gamma release assays are performed

How can we tell if an infection has occurred recently
When B cells are stimulated the original isotype is IgM, and IgG is formed by class switching as the immune response develops
If IgM is negative, with IgG positive this is a distant infection
IgM positive, but IgG negative or positive it’s a recent infection
But IgM can come back in reactivation
Paired sample
Ideally we want an acute and a convalescent sample (paired sample)
We get the acute sample as early as we can
And for the convalescent sample we wait 2-3 weeks to try see a seroconversion (or an increase in antibody levels)
Seroconversion
We define as going from negative to positive for IgG or a four fold increase in titre (the inverse of the dilution of the serum)

What is affinity and avidity?
And how does avidity change over the course of the infection
Affinity
Single interaction between epitope and antigen-binding site
Avidity
Accumulated strength of multiple affinities - it’s essentially the overall antibody response (multiple different antibodies, the accumulated strength of multiple affinities)
Over the course of the infection, the avidity response increases
How are high affinity antibodies made in the germinal centre
There is a naiive B cell which has been exposed to antigen and activated, it goes into the germinal centre There are two regions of the germinal center:
The dark zone: activated B cell which can produced IgM and has IgD on the surface undergoes clonal expansion, then it undergoes somatic hyper mutation , it expresses an enzyme which mutates the bases of the antibody gene
Light zone: these then move into the light zone, and those that have an improved affinity for the antigen are able to undergo class switching, whilst those that have disadvantageous mutations and can’t recognise the antigen present from the dendritic cell undergo apoptosis

how do we measure avidity
We’re measuring whether it’s recently gone through the germinal centre reaction or not (how mature the B cell response it)
Chaotropic agent = disrupting agent
We add serum to wells coated with antigen - if there are antibodies specific for antigen it will bind to antigen
- We then either treat it with a chaotropic agent or not - this disrupts the bond
- Therefore the higher the affinity of the antibody the more that stay bound, but the weaker the affinity a lesser amount will stay bound
We have 1 antibody left out of 3, so the avidity is 0.33 - this is a low avidity response, which suggests a recent infection, and is therefore at risk of transmtting it to the baby.



