Lecture 1: Pharm of Renal Infections Flashcards
What type of UTI is most likely in a nonpregnant women without anatomic abnormalities or instrumentation of the urinary tract?
Uncomplicated UTI
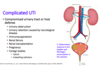
What are some of the predisposing factors which would make a UTI be considered complicated?
- Urinary obstruction
- Urinary retention caused by neuro disease
- Immunosuppression
- Renal failure or Renal Transplantation
- Pregnancy
- Foreign bodies: Calculi or Indwelling Catheters
UPEC relies on what adhesive organelle to form a biofilm?
Type 1 pili, antigen 43, curli
How is P. mirabilis able to form a biofilm for inhabiting the urinary tract?
What are the components of this biofilm?
- Produce urease
- Calcium crystals + magnesium ammonium phosphate precipitates
- Crystalline biofims
How is P. aeruginosa able to form a biofilm for inhabiting the urinary tract?
What are the components of this biofilm?
- Changes hydrophobicity of its surface
- Uses lectins, rhamnolipids
What does E. faecalis use to form a biofilm?
Fibrinogen
A young, non-pregnant female presents with dysuria, frequency, urgency, nocturia, and some suprapubic discomfort. On PE you notice some gross hematuria.
What type of UTI does this fit the criteria of?
Uncomplicated Cystitis

What are the 3 first line agents for Uncomplicated Cystitis?
- Nitrofurantoin
- Trimethoprim-Sulfamethoxazole (TMP-SMX)
- Fosfomycin
What class of agents is used as a second line treatment for Uncomplicated Cystitis?
List 4 drugs in this class.
- Oral beta lactams
- Amoxicillin, Cefpodoxime, Cefdinir, Cefadroxil
Which class is of Abx is uses as the third line for treatment of Uncomplicated Cystitis?
List 3 drugs in this class
- Fluoroquinolones
- Ciprofloxacin, Levofloxaxin, Ofloxacin
The first line agents for cystitis, Fosfomycin and Nitrofurantoin, target which gram-type of bacteria?
Gram positive and gram negative
What is the MOA of Nitrofurantoin?
- Converted into highly reactive intermediate
- Disrupts synthesis of proteins, RNA, and DNA
Nitrofurantoin antagonizes what other drug?
Contraindicated in which pts?
- Antagonizes nalidixic acid (synthetic quinolone Abx)
- Contraindicated in pts w/ G6P dehydrogenase deficiency
What is the MOA of Fosfomycin?
- Cell wall synthesis inhibitor
- Inhibits cytoplasmic enzyme enolpyruvate transferase
By which method may a bacteria become resistant to Fosfomycin?
Inadequate transport of drug into cell
Which first line agent for cystitis come in an oral form and is safe to use in pregnancy?
Fosfomycin
Nitrofurantoin and Fosfomycin should not be taken in pts when there is suspicion of?
- Early pyelonephritis
- Does NOT achieve adequate renal tissue levels
What are the two 3rd gen Cephalosporins used as a second line to treat cystitis?
Target which gram-type of bacteria?
- Cefpodoxime
- Cefdinir
*Target gram negatives
What is the 1st generation cephalosporin used as a second line tx for Cystitis?
Targets which gram-type of bacteria?
- Cefadroxil
- Targets gram positive and gram negatives
Which adverse effects exist for Fluoroquinolones and is why the FDA states that disabling and potentially irreversible effects of these drugs outweight their benefits in treating uncomplicated cystitis?
- Tendinitis and tendon rupture
- Peripheral neuropathy
- CNS effects

Which 2 drugs should not be used to emperically treat uncomplicated cystitis due to possibility of resistance?
- Ampicillin
- Amoxicillin
If resistance is identified in someone with uncomplicated cystitis, which drug/class can be used?
This drug is insufficiently active against what bacteria?
- Ertapenem (a carbapenem)
- Insufficient against P. aeruginosa

To determine what drugs to use, what are the major signs/sx’s of someone with Pyelonephritis?
- Unilateral back or flank pain
- Fever (can be high or low grade) w/ N?V
Which antibiotic class is the first line for Pyelonephritis?
List the 2 drugs that are used?
- Fluoroquinolones
- Ciprofloxacin or Levofloxacin
If severe pyelonephritis or risk factors for resistance, fluoroquinolones should be adminstered with what parenteral broad spectrum antibiotics until susceptibility data is available?
- Ceftriaxone (3rd gen.)
OR
- Aminoglycosides: Gentamicin or Tobramycin
Aminoglycosides (i.e., Tobramycin or Gentamicin) are active against which gram-type and specific bacteria?
Aerobic gram negatives + P. aeruginosa
What is the MOA of aminoglycosides?
Irreversible protein synthesis inhibitor, binds 30S ribosomal subunit
What are 3 AE’s associated w/ Aminoglycosides?
*Hint: Sheehy gave us a way to remember using the name.
- CN VIII toxicity: vertigo and hearing loss
- Renal toxicity
- Neuromusclar blockade
*“A-Mean-Guy will punch you in the ear, then the kidney, and finally knock you out”
What are the 3 second-line agents which can be used for pyelonephritis in a pt who is hypersensitive to fluoroquinolones or there is resistance?
- TMP-SMX
- Oral beta lactams –> Amoxicillin, Cefpodoxime, Cefdinir, Cefadroxil
- Aztreonam
If a pt w/ pyelonephritis cannot tolerate TMP-SMX or oral beta lactams, what do you give them?
Aztreonam
What is the structure of Aztreoname that allows it be used in penicillin hypersensitive patients?
Monobactam, monocyclic beta-lactam ring
Aztreonam has activity against which type of bacteria?
*Way to remember from CMMRS*
Aerobic gram-negatives (P. aeruginosa)
*“Tree falls on house = negative experience and will probably let air in (aerobes)
What is the MOA of Aztreonam?
- Cell wall synthesis inhibitor
- Transpeptidase inhibitor
Which 2nd line agent for Pyelonephritis comes in IV form?
Aztreonam
What are the AE’s seen in children associated with Aztreonam?
- Neutropenia (3-11%)
- Pain at injection site (12%)
What is the clinical presentation of Complicated UTI and is often due to what?
- Severe dysuria (painful urination)
- Often due to an indwelling catheter
What are the 2 first line agents for complicated cystitis?
Ciprofloxacin or Levofloxacin = Fluoroquinolones
Fluoroquinolones are used for complicated cystitis due to their coverage of which bacteria?
P. aeruginosa
*Ciprofloxacin or Levofloxacin
In complicated cystitis, the presence of gram-positive cocci on gram stains suggests what type of organism causing the UTI?
Can use what 2 antibiotics?
- Enterococcal UTI (i.e., E. faecalis or E. faecium)
- Ampicillin or Amoxicillin
Which urinary analgesic can be used for pain relief in complicated cystitis?
Common finding/AE of this drug?
- Phenazopyridine
- Colors urine orange/red
What are the 3 first line agents used in mild complicated pyelonephritis?
When is each used (i.e., bacteria and hypersensitivities)?
1) Ceftriaxone
2. Ciprofloxacin or Levofloxacin –> covers P. aeruginosa
3) Aztreoname –> alt. in setting of beta lactam allergy

The beta-lactamase inhibitors: tazobactam and avibactam are available in combinations with beta lactam drugs and can be used for severe complicated pyelonephritis, what 3 combos exist?
- Piperacillin + Tazobactam
- Ceftolozane (5th gen.) +Tazobactam
- Ceftazidime (3rd gen.) + Avibactam
The beta-lactamase inhibitors used in combo for severe complicated pyelonephritis are good inhibitors of which type of beta-lactamases?
Produced by which 2 bacteria which can cause UTI’s?
- Ambler class A β-lactamase
- E. coli and K. pneumoniae

The beta-lactamase inhibitors used in combo for severe complicated pyelonephritis are poor inhibitors of which type of beta-lactamases?
Produced by which 2 bacteria which can cause UTI’s?
- Class C β-lactamases
- Produced by Enterobacter spp. and P. aeruginosa
Which 3 Carbapenems can be used as first line therapy for severe complicated pyelonephritis?
Effective against which types of bacteria?
- Imipenem, Doripenem, and Meropenem
- Wide spectrum = good activity against gram negatives (including P. aeruginosa) + gram positives and anaerobes
Carbapenems are resistant to?
Beta-lactamases
What is the MOA of carbapenems?
Inhibit transpeptidase
What is significant about the pharmacokinetics of Doripenem, Meropenem, and Ertapenem?
NOT metabolized by dihydropeptidase
Which carbapenem is most commonly used, but is associated w/ seizures so should be avoided in pts with a history or risk of seizure?
Imipenem
Which β-lactam can be used as a first line monotherapy for treating severe complicated pyelonephritis?
Cefepime (4th gen Ceph)
Which β-lactamase inhibitor + β-lactam combo can be given at a higher dose as a first line treatment for severe complicated pyelonephritis if P. aeruginosa is suspected?
- Piperacillin + tazobactam
Which carbapenem can be given at a higher dose as a first line treatment for severe complicated pyelonephritis if P. aeruginosa is suspected?
Meropenem
Which 2 carbapenems have slightly greater activity against gram negatives and slightly less against gram positives?
Doripenem and Meropenem
What is the MOA of the β-lactams?
Cell wall synthesis inhibitors, bind/inhibit transpeptidase
Prostatitis is most often caused by what bacteria?
E. coli
What are the 3 agents which can be used to treat Prostatitis?
- TMP-SMX
- Ciprofloxacin
- Levofloxacin
What is the MOA of fluoroquinolones?
- Inhibit transcription and replication of bacterial DNA
- Through inhibition of topoisomerase II (DNA gyrase) and topoisomerase IV
Describe the 3 different mechanisms by which bacteria can develop resistance to fluoroquinolones
- Mutation to quinolone binding region on either DNA gyrase or topoisomerase IV
- Active drug efflux
- Upregulation of proteins that protect and shield both DNA gyase and topoisomerase IV
Prolonged treatment with trimethoprim part of TMP/SMX can cause what AE’s?
- Anemia
- Leukopenia
- Granulocytopenia
PSGN is caused by prior infection with what bacteria and what is it’s gram stain?
- Group A β-hemolytic streptococcus
- Gram positive
Which drug can be given IM for patient with recurrent group A β-hemolytic streptococcus infection especially if adherence to previous antibiotic uncertain?
Penicillin G
When giving β-lactams such as piperacillin and cephalosporins, what AE/contraindication must you be aware of?
β-lactam hypersensitivity –> Anaphylaxis
Repeat treatment for group A beta-hemolytic streptococcus infection should be given with an agent with greater what?
β-lactamase stability
For tx of recurrent group A β-hemolytic strep infection focused on using agents with greater β-lactamase stability describe which drugs/class can be used in order of greater β-lactamase stability?
- Penicillin G (given IM)
- 1st gen. cephalosporins –> Cephalexin or Cefadroxil
- 3rd gen. cephalosporins –> Cefpodoxime or Cefdinir
- Amoxicillin (aminopenicillin) or Clindamycin = greatest β-lactamase stability

Clindamycin, used for recurrent PSGN, is very effective against bacteria which grow under what kind of conditions?
Anaerobes
What is the MOA of clindamycin?
Protein synthesis inhibitor, binds to the 50S ribosomal subunit
What is a major AE associated w/ Clindamycin use?
C. difficile induced diarrhea and colitis


