L11 - K Okkenhaug - Hypersensitivity Flashcards
(30 cards)
what is hypersensitivity?
over reactions of the immune system - to non harmful stuff
what are the types of hypersensitivity?

describe Type 1 hypersensitivity
- rapid allergic reactions
- host has pre-existing IgE antibody (gerneated through Th2 response)
- MAst cells - via FcRI cross linking degranulate histamine
- IgE is probably prebound to its receptor
what properies to allergen have in common?
why do they stimulate a strong IgE response
- often proteases.
- They are generally low MW
- highly soluble, so they diffuse readily into mucus.
- They are also generally stable and can survive as a desiccated particle
how do we determine sensitivity to allergens?
skin-prick test. A ‘wheal and flare’ reaction appears at the site of infection within a few minutes. The wheal is swelling (edema) and the subsequent redness (flare or erythema) is from increased blood flow.
is type I sensitivity common/
very - upto 30% of some populations
type I:
These atopic (atopy is a predisposed state) individuals have serum IgE raised 1—- times the normal level.
These atopic (atopy is a predisposed state) individuals have serum IgE raised 10-100 times the normal level.
describe systemic anaphylaxis
allergen directly into blood - systemic anaphylaxis
increased permeability of blood vessels results in extreme drop in blood pressure and anaphylactic shock, which can be fatal.
treatment ofr type I hypersensitivity
identification and avoidance of the antigen; as well as antihistamine and corticosteroids, which suppress leukocyte function.
In some cases, desensitisation may be achieved by gradual exposure to increased dose of antigen, to convert Th2 to Th1 and/or iTreg responses.
outline asthma
chronic inflammation of the airways characterised by increased TH2 lymphocytes, eosinophils, neutrophils and basophils, which amplify inflammation and airway remodeling
which genetic loci affect asthma?
HLA class II,
TCR and genes which affect the TH1/TH2 balance.
Other genes affect the IgE receptor and cytokines including IL-4.
In addition, are effects of non-immune genes such as those influencing smooth muscle cell behavior, bronchial physiology and tissue repair. Mice lacking the T-Bet transcription factor, which drives T cells to differentiate into TH1 cells, and suppresses the TH2 pathway, have increased levels of IL-4, IL-5 and IL-13 cytokines and have a disease similar to human asthma.
how do you test for asthma
breathing exhalation rate tested after exposure to known allergen
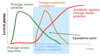
describe the late repsonse for asthma
As in the skin test, a late response follows after about 6 hours, due to leukotrienes and other inflammatory mediators. This phase is most damaging and leads to recruitment of eosinophils and TH2
lymphocytes
why do type 1 allergies occur so fast
pre existing IgE
describe type 2 hypersensitivity
IgM or IgG antibody binding to cells or tissue antigens
blood transfusion is an example of what type of hypersensitivity?
2
describe how blood matching works?

how does the ABO blood group system work?
- Molecules consist of a core H antigen
- The O (null) allele is unmodified H antigen
- Sugars may be attached to this core:
- The A allele adds a terminal N-acetylgalactosamine The B allele adds a terminal galactose
- AB indicates both modifications
describe the rhesus reaction (blood)
- blood incompatability
- mother is Rhesus negative and the child is Rhesus positive the mother can produce antibodies to the Rhesus antigen
- some Rh+ cells leak into the maternal circulation at birth
- IgG can cross the placenta and compromise the subsequent Rh+ baby.
treatment for rhesus reaction?
giving anti-Rh antibody (RhoGam) to the mother before she reacts to her child’s red blood cells. The antibody crosslinking to FcgRIIB receptor prevents activation of naïve B cells (see lectures on antibody and tolerance).
describe type 3 hypersensitivity
antigen: soluble
quantity: high - IgG response
(low quantities = IgE responses)
- Immune complexes form and are deposited in tissues.
- These trigger mast cells via the low affinity FcRIII receptor.
- Complement is activated and polymorphs are attracted to the site of deposition, causing local tissue damage and inflammation.
examples of type 3 responses
arthritis and glomerulonephritis
Other examples of T3 hypersensitisation include pigeon fancier’s lung or farmer’s lung, where the antigen is _____.
Other examples include pigeon fancier’s lung or farmer’s lung, where the antigen is inhaled.
what is serum sickness
used to result when high doses of horse serum were used to treat pneumonia.
This classic form of type III hypersensitivity is rarely seen now although injection of serum is still used as anti-snake venom.