HIV Flashcards
(70 cards)
What does ‘natural history of HIV infection’ mean?
hallmark of disease progression
The course of the disease process in the absence of tx
- CD4+ T cell depletion
- cellular immunity impairment
- susceptibility to opportunistic infections
HIV enter and time to spread across body
Retrovirus of lentivirus family
virus particles enter via genital mucosa/directly into bloodstream -> to lymph nodes in CD4+ T cells -> body spread in 3-5 days
HIV viral replication cycle
- binding = CD4+ T cells, CD4 molecules, co-receptors (CCR5/CXCR4). CD4 also on monocytes/macrophages, DCs, eosinophils, microglial cells
- fusion
- reverse transcription
- integration
- protein synthesis, processing and assembly
- budding
three issues with HIV
Destruction of infected CD4+ T cells
- early in infection -> regeneration and re-establishes -> immune function preserved for many years
- chronic immune activation, immune dysregulation, ongoing direct viral killing of CD4 cells -> CD4 cells gradual decline -> fall below threshold -> opportunistic infections occur
Rapid HIV mutation
- new generation every 1.5 days
- no proof-reading mechanism so mutation very quick
- -> genetical diverse virus pool, some evade detection by the immun system
Reservoirs of latent infection
- HIV replication requires CD4+ cell activation
- some CD4+ cells infection with HIV are resting, and persist as latently infected cells if they are not killed
- even with viral replication is suppressed by antiretroviral drugs, this infection reservoir persists for many years -> why HIV infection cannot be eradicated with current tx
3 clincial stages of HIV infection: primary/acute infection
- primary/acute infection
- asymptomatic chronic infection
- symptomatic disease, including AIDS
Primary infection
- 1-4 wks after virus inquisition until production of sufficient HIV antibodies to be detected by an HIV antibody test
- sx’s 40-90% individuals, lasts 7-10 days = fever, malaise, arthralgia, loss of appetite, rash, myalgia, pharyngitis, oral ulcers, weight loss >2.5 kgs aka anorexia
- neuro sx (high viral loads in CSF) = headache, menignism (photphobia, neck stiffness/nuchal rigidity, seizures, kernigs and brudzinksi’s sign), CN palsies, transient hemiplegia/dysarthria
- DDx = often missed (ddx infectious mononucleosis/EBV/VMW, influenza, malaria, acute hep B/C, 2o syphilis, rubella, drug reaction e.g. to ART in PEP for HIV), always consider when presentation is unexplained fever,
- Dx = clincial suspicion, p24 antigen or viral load
- viral load = 100 million RNA copies per ml of blood, massive CD4+ depletion in gut-associated lymphoid tissue, CD4+ count in seurm may fall, high viral load in blood and genital fluids increases the risk of onwards transmission
*
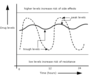
- asymptomatic chronic disease
Lasts 5-10 years
HIV viral load falls and then plateaus
stable HIV viral load ‘set point’ = rises as ‘AIDS’ develops
CD4 count usually recovered but not usually to baseline levels
- STILL functional deficiencies in CD4+ T cell responses
CD4 count gradually falls overt ime

Symptomatic disease progression
First manifestions
- frequent minor infections e.g. viral infections, recurrent vaginal/oral candidiasis (agular cheilitis sign around mouth in candida)
- derm (dry skin, seborrhoeic dermatitis, psoriasis)
- haem (anaemia, thrombocytopaenia)
- systemic (fatigue, weight loss, night sweats, diarrheoa)
unusual infections
- oral hairy leukoplakia
- multidermatomal shingles
AIDS-defining syndromes, infections and malignancies (represents severe immunosuppresion)
- rare above CD4 >200
- CMV retinits unusual until CD4<50
- candidiasis of oes, bronchi, trachea, or lungs
- herpes simplex of oes, bronchi, trachea, or lungs
- cryptococcosis
- cytomegalovirus disease
- HIV encephalopathy
- Kaposi’s sarcoma (HHV8, KSHV)
- Lymphoma: Burhkitt’s, immunoblastic, primary cerebral
- Mycobacterium avium complex, TB, or other species
- PCP
- Progressive multifocal leukoencephalopathy (JC virus)
- toxoplasmosis, cerbral

Opportunistic and not opportunistic infections

malignancies associated with viral infections

the role of HIV in non-AIDS-defining clinical disease
renal
- post-infectious glomerulonephritis
- HIV-associated neuropathy (HIVAN) = more common in black ethnic groups, men and injecting drug users
cardiovascular
- increased rates of atherosclerosis
- HIV-associated dilated cardiomyopathy
- pericarditis and pericardial effusions
- pulmonary hypertension
hepatic
- fast progression of cirrhosis in those with Hep B and C infection
- higher rate sof NASH
bone
- ostopaenia, osteoporosis
- high rates of vit D deficiency and osteomalacia
- osteonecrosis
neuro
- peripheral neuropathy
- bell’s palsy
- mononeuritis multiplex
- vauolar myelopathy
- cognitive impairment
LTNPs
long term non-progressors 5% of HIV patients = maintain low viral laods and good CD4 counts over many years (over 20 years in some cases)
Disease progression = host and viral factors
Disease progression is faster in those who have a symptomatic primary infection, particularly in those who have a severe and prolonged seroconversion illness.
Host factors
- CCR5 (good), HLA I alleles (B27, B57)
- CD8+ HIV-specific TY cells destory HIV-infected CD4+ cells by MHC I-restricted cytolysis/indirectly via cytokines and chemokines. Host cellular transcription factors.
Viral fitness
- HIV mutations that = evolve to evade the immune response, develop under pressure of AR’s (and confer drug resistance)
life expectancy
variable
atients in Europe and North America who start antiretroviral therapy and whose CD4 counts rise to above 350 at 1 year after treatment initiation have an estimated life expectancy approaching that of the general populatiom
Recent improvements in survival with HIV probably reflect transition to less toxic antiretroviral drugs, improved adherence, prophylactic measures, and management of comorbidity
HIV-2
1 = from chimpanzee
2 = sooty mangabey monkeys in West Africa (spread to Portugal and their former colonies)
- less transmissible, less pathogenic
- viral loads lower
- disease progression is slower
routine monitoring of people living with HIV
All HIV+ adults
Pre-ART initiation
Immediately post-ART initiation
Established ART
Not current wanting ART
HIV hx

sexual hx in HIV
- unprotected sex in last 72 hours (vaginal/anal) -> to offer post-exposure prophylaxis to partners
- hx from all sexual partners since the last negative HIV test, or lifetime aprtners if never tested before -> contacted and offered testing
- advice on safer sex, contraception and pre-conception (try to conceive with least risk to their partner)
- women not on ART/without an undetectable viral load -> self-insemination
- men not on ART/without an undetectable viral load -> fertility clinics to arrange sperm washing
HIV physical exam
general = skin, oropharynx, lymph nodes, heart, lungs, abdominal (hepatosplenomegaly), MSK, neuro, anogenital, cognitie function testing
measure weight, height, BMI, waist circumference, BP
In CD4 <50/ul = dilated fundoscopy or retinal photography to look for CMV retinitis
HIV Ix’s
- HIV-1/2 status = serology, HIV avidity assays
- CD4 cell count and CD4% =
- HIV viral load = measure RNA in plasma (time since last test, known time of exposure, sx of seroconversion illness, test for 1o HIV infection, CD4 count). Steady state after around 4 months
- resistance and HLA-B*57:01 testing = HLA one for Abacavir therapy as +ve can mean abacavir hypersensitivity reaction
- biochemistry and haematology = metabolic problems (insulin resistance, lipid dysregulation, renal/liver/bone/disease) -> renal/liver/bone profile, HbA1c, dipstick urinalysis + urine protein/creatinine ratio if dipstick +ve for protein, FBC
- other infections and immunity = hep B and C serology, immunity to hep A/measles/varicella, full STI screen including syphilis serology, IGRA
- women = cervical cytology 25-65 (and not done in last 12 months), rubella immunity in women of child-bearing age
- over 40s = QRISK2, FRAX tool (over 50s)
routine monitoring for HIV+ not on ART

pre-ART routine monitoring

immediately post-ART routine monitoring

established ART routine monitoring
hx:
- adherence to ART
- medications
- contraception and plans for conception
- symptoms

what things should you consider on top of routine monitoring