Histopathology Flashcards
What are the role of neutrophils?
Acute inflammation - first responses
Describe the appearance of neutrophils.
Multi-lobed
Describe the recruitment of neutrophils.
Margination - move into margin of blood vessels, affected by blood flow Rolling - not fully adhesive Adhesion - fully adhesive Transmigration/diapedesis - either through or between endo cells and through BM
What are the role of lymphocytes and plasma cells?
Chronic inflammation
Describe the appearance of lymphocytes.
Little cytoplasm Big nucleus
What are the role of eosinophils?
Allergic reactions Parasitic infections Tumours e.g. Hodgkin’s disease (reaction to tumours
Describe the appearance of eosinophils.
Bi-lobed nucleus Red granules
What are the roles of mast cells?
Allergic reactions
Describe the appearance of mast cells.
Very large and prominent granules
What are the roles of macrophages?
- Late acute inflammation
- Chronic inflammation - granulomas etc
- Naturally phagocytic - in chronic inflammation they become secretory
Describe the appearance of macrophages.
- Small nucleus
- Lots of cytoplasm - becomes even more with increased ER and golgi bodies when secretory in chronic inflammation
What is a granuloma?
- Organised collection of activated macrophages (epithelioid macrophages)
- Secretory macrophages
- Associated with infections e.g. TB, leprosy, fungal infection
Define carcinoma.
Malignant tumours of epithelial cells
What are the features of squamous cell carcinoma?
- Intercellular bridges
- Keratin production (not in all)
- Skin, head and neck, top oesophagus, cervix, vagina, anus
What are the features of adenocarcinoma?
- Forms from glands
- Mucin production
- Lung, breast, stomach, bottom oesophagus, colon, pancreas, sweat glands
What are the features of transitional cell carcinoma?
Multi-layered Urinary tract - e.g. bladder, ureter
What type of tumour are these images? Describe why.

Squamous cell carcinoma
- Keratin at the top
- Intracellular bridges - parallel lines between cells
- Swirls of keratin
What type of tumour are these images? Describe why.

Adenocarcinoma
- Mucin stain with glands - show up blue
- Dark irregular nuclei still froming gland-like structure
What type of tumour are these images? Describe why.

Normal glandular epithelium with crypts
What are the 2 types of stains?
Histo-chemical
Immuno-histochemical
Describe histo-chemical stains and give some examples.
Chemical reaction between stain and specific component of tissue
Product of reaction has specific colour or property that can be identified
- Haematoxylin and eosin, Prussian blue iron, Congo red
What is the haematoxylin and eosin stain used for?
Most common histochemical stain to visualise cells for light microscopy
- Used in cancer diagnosis
What is the Prussian blue iron stain used for?
To detect the prescence of iron in tissue
- Haemachromatosis
What is the Congo red stain used for?
Amyloid
Describe immunofluorscence stains.
Fluorescent tag to bridge antibody to make it visible
Examined under a fluorescent microscope
Describe immunoperoxidase stains.
Detector system is an enzyme which is tagged to antibody
Bridging system to antibody to make it visible
Add substrate which makes colour change
How does carcinoma spread?
Lymphatics
How does sarcoma spread?
Blood
What shape are hepatic lobules?
Hexagonal
Where are portal triads located and what are in them?
Each corner of the hepatic lobule
Bile ducts, portal venule, hepatic arteriole
What is the direction of blood flow from the portal triad?
Towards central vein via sinusoids
What is the direction of bile flow from the portal triad?
Produced by hepatocytes towards the bile ductule via canaliculi (away from the central vein)
What is the oxygen supply and metabolic markers of zone 1 in hepatic lobules?
Richest oxygen supply
Highest levels of ALP
What is the oxygen supply and metabolic markers of zone 3 in hepatic lobules?
Lowest oxygen supply
Most metabolically active cells - suscept to hypoxic or drug damage
What are the causes of acute hepatitis?
Viruses - hepatitis viruses, other in immunosuprressed
Drugs
Alcohol
What are the causes of chronic hepatitis?
Viruses
Drugs
AI
PBC
PSC
Wilson’s
Haemachromatosis
What are the histological signs of acute hepatitis?

What are the pathological signs of chronic hepatitis?
How is bilirubin processed?
Conjugated by the liver
Excreted via bile and kidneys
- Normal to have urinary urobilinogen (bilirubin converted by gut bacteria and reabsorbed via the enterohepatic circulation to be excreted via the kidneys)
What are the main features of obstructive jaundice?
- Lack of urinary urobilinogen
- Itching - bile salts/acid deposition
- Pale stool - lack of stercobilinogen
Dark urine - conjugated bilirubin leaking out into urine
Define transudate fluid.
Protein content <30g/L
Define exudate fluid.
Protein content >30g/L
What are the causes of transudate fluid?
Cardiac failure
Renal failure
Cirrhosis
Hypoalbuminaemia
What are the causes of exudate fluid?
Malignancy
Pancreatitis
Intra-abdominal TB
Decribe the histology of alcoholic fatty liver disease (AFLD).
Fat deposition
Neutrophil Polymorphs
- IS REVERSIBLE
Describe the histology of alcoholic hepatitis.
Neutrophils infiltrating the liver
Balloon cells containing Mallory-Denk bodies (or mallory hyaline)
Accumulation of bile as hepatocytes swell with the balloon cells & block the flow of bile (reversible/irreversible)

Describe the histology of liver fibrosis.
Use collagen blue stain → collagen deposition around hepatocytes indicating scarring

Describe the histology of liver cirrhosis.
Regenerative nodules of hepatocytes
Cuff of fibrous tissue (micronodular cirrhosis)
Fibrous connective tissue that bridges between portal tracts
Distortion of vascular architecture - regeneration is disorganised so blood trying to get around the nodules leads to the portal hypertension
- IS IRREVERSIBLE

What are the features of stable chronic liver disease?
Palmar erythema
Gynaecomastia
Dupytren’s contracture
Spider naevi
What are the features of portal hypertension?
Caput medusae
Splenomegaly
Ascites
What are the features of hepatic encephalopathy?
Asterixis
What is this?

Alcoholic Fatty Liver Disease (AFLD)
WHat is this?
Alcoholic hepatitis
What is this?

Liver cirrhosis
What is this?

Liver fibrosis
What is non-alcoholic steatohepatitis (NASH)?
Similar features to AFLD but with alcohol history
- Fat deposition
- Neutrophil polymorphs
Most NASH patients have diabetes
What are the features of autoimmune hepatitis?
Inflammation
Necrosis + Fibrosis → Cirrhosis & Liver failure
What are the distinct features of Type 1 autoimmune hepatitis.
Anti-smooth muscle Abs +/- ANA
Occurs from 10 years of age → elderly
What is the prognosis of Type 1 compared to Type 2 autoimmune hepatitis?
Type 1 responds well to steriods whereas type 2 doesn’t
Type 1 has an overall better prognosis
What are the distinct features of Type 2 autoimmune hepatitis.
Anti-liver kidney microsomal-1 Abs
Tends to present in children
Association with IgA deficiency
What are the distinct features of Type 3 autoimmune hepatitis.
Anti-soluble liver antigen Abs
Describe the histology primary biliary cirrhosis (PBC).
Chronic granulomatous inflammation of the bile duct
What are the syptoms of primary biliary cirrhosis (PBC)?
Itching
Fatigue
Abdominal pain
What are the distinct features of PBC?
Anti-mitochondrial Abs
F>M
Most common in middle-age
Often have raised IgM levels
Often associated with other AI disorders e.g. scleroderma, RA
What does the blood work of PBC show?
Raised serum cholesterol
High ALP
High bilirubin
What are the histological features of primary sclerosing cholangitis (PSC)?
Beading of the bile ducts on ERCP - due to strictures
Fibrosis of the bile ducts throughout the biliary tree with associated stricture formation
Onion skinning fibrosis

What are the features of PSC?
Fibrosis symptoms
M>F
p-ANCA +ve
60% associated with UC
Bile duct dilatation on US
Increased risk of cholangiocarcinoma
What is the most common type of cancerous liver tumour?
Metastases
What is the most common type of benign liver lesions?
Haemangioma
What is the most common cause of hepatic adenomas?
COCP
What factors affect the grading of chronic hepatitis?
Dependent upon inflammation
- Portal inflammation = inflammation confined within limiting plate
- Interface hepatitis = between the portal tract and the parenchyma
- Lobular inflammation = across the whole lobe
Describe the liver fibrosis staging.
F0: no fibrosis
F1: portal fibrosis without septa
F2: portal fibrosis with few septa
F3: numerous septa without cirrhosis
F4: cirrhosis
What is Wilson’s disease?
Low ceruloplasmin
AR inheritance of a mutated copper transport gene → inability of liver to secrete the copper-ceruloplasmin complex into the plasma
What are the features/symptoms of Wilson’s disease?
Parkinsonian features
Liver disease
Kayser-Fleisher rings around cornea
Psychiatric history
What stain is used for Wilson’s disease?
Rhodanine stain
What medication is use for Wilson’s disease?
Penicillamine
What is Hereditary haemachromatosis?
Excess iron
AR inheritance causing excess iron absorption in the gut and therefore excess iron deposition - haemosiderin deposition in organs
What are the histological features of hereditary haemachromatosis?
Rusty brown appearance
What are the features/symptoms of hereditary haemachromatosis?
- Brown/bronze discolouration of the skin
- Diabetes - previously known as golden diabetes
- Slate-grey discolouration
- Steatorrhoea
What is the treatment for hereditary haemachromatosis?
Therapeutic phlebotomy
What is Gilbert’s syndrome?
AR benign condition resulting in reduced conjugation of bilirubin
- due to reduced activity of UDP Glucuronyl transferase
What are the blood work of Gilberts syndrome show?
LFTs will be normal
- Isolated rises in unconjugated bilirubin
Name some triggers for jaundice caused by Gilbert’s syndrome?
Alcohol
Dehydration
Infection
Stress
Exercise
Fasting
Menstration
What is Budd-chiari syndrome?
Hepatic vein thrombosis causing outflow tract obstruction
- Associated with polycythaemia rubra vera
What are the signs/symptoms of Budd-chiari syndrome?
Hepatomegaly
Ascites
- Sometimes symptoms of polycythaemia - often no symptoms but can be headaches, blurred vision, fatigue, weakness, itchy skin, dizziness, hight sweats

- Mesothelioma
- Associated with asbestos exposure
- Can be visceral or parietal pleura
How long is the latency period between asbestos exposure and mesothelioma?
- 20 years
- Pleural fibrosis
- Pleural plaques
What is the key feature associated with mesothelioma?
- Plueral effusions



- The patient has suffered multiple chest infections
- Suggests a likely Cystic fibrosis
What are the most likely pathogen to cause chest infections in a patient with CF?

Acute MI
What are the consequences of an MI?
Death
Arrhythmia
Rupture
Tamponade
Heart Failure
Valve Disease
Aneurysms
Dressler’s Syndrome
Embolism
Re-infacrtion

Systemic Hypertension

Right Coronary Artery - Inferior MI

A previous MI

Left Anterior Descending
Which artery is affected if ECG lead I shows ST elevation?
Circumflex artery
- Lateral
Which artery is affected if ECG leads II, III and aVF shows ST elevation?
Right cornary artery
- Inferior
Which artery is affected if ECG lead V1, V2, V3 and V4 shows ST elevation?
Left anterior descending
- Anterior

Nutmeg Liver
What are the causes of nutmeg liver?
- Right heart failure - Most common
- Obstruction of blood flow in hepatic vein
- Obstruction of blood flow in the inferior venacava
- Pathogensis:
- Increased pressure in the hepatic veins cause stasis of blood causes deoxygenation of hepatocytes
- Necrosis occurs which is surrounded by paler zone which contains damaged hepatocytes with fatty change
- Adjacent to this zone normal unaffected hepatocytes are present which are adjacent to hepatic arteriole and are better oxygenated

Chronic stable liver disease
What is Bullous pemphigoid?
An autoimmune skin disease that causes tense bullae on flexor surfaces
- Dermo-epithelial junction affected
- 10-20% mortality - risk factor for serious skin infections/sepsis
What is pathophysiology of Bullous pemphigoid?
- IgG and C3 attack the basement membrane
- Detected by immunofluorescence
- IgG anti-hemidesmosome
- Eosinophils recruited to release elastase
- Elastase damages the anchoring proteins
- Fluid fills up gap between BM and epithelium
What is Pemphigus vulgaris?
Autoimmune skin condition resulting in the formation of flaccid blisters which are prone to rupture
- Affects the epiderma-epidermal junction
What is the pathophysiology of pemphigus vulgaris?
- IgG attacks between the keratin layers (acantholysis)
- i.e. loss of intracellular connections
- Need immunofluorescence to confirm
What is Pemphigus folliaceus?
IgG-mediated autoimmune condition in which the outer layer of stratum corneum shears off
What is discoid eczema?
Coin-shaped rashes on the flexor surfaces
What is Contact dermatitis?
A localized rash or irritation of the skin caused by direct contact the inducing substance to which the skin reacts
- Itchy thickened skin
What is the pathophysiology of Contact dermatitis?
- Epidermis gets thicker
- Eczema is spongiotic because there is oedema in between the keratinocytes
- T cell mediated and eosinophils are recruited
- A differential for an eczematous reaction pattern is a drug reaction
What is the diagnosis of an 85 year old presenting with this?

Bullous pemphigoid
What is the diagnosis?

Pemphigus vulgaris
What is the diagnosis?

Pemphigus foliaceus
What is the diagnosis if this rash is found a flexor surface?

Discoid eczema
What is the diagnosis?

Contact dermatitis
What is plaque psoriasis?
A skin disease that causes silver plaques on extensor surfaces
What is the pathophysiology of plaque psoriasis?
- Rapid keratinocyte turnover leads to a thicker epidermis
- A layer of parakeratosis forms at the top
- Stratum granulosum disappears as not enough time to form it; and dilated vessels form
- Munro’s microabscesses form, made up from recruitment of neutrophils
What is Lichen planus?
T-cell mediated autoimmune condition resulting in purplish-red papules and plaques on wrists and arms
If a patient presents with this rash on extensor surfaces?

Plaque psoriasis
What are Wickham striae?
White lines found in the mouth of patients with Lichen planus
What is the pathophysiology of Lichen planus?
- T-lymphocytes have destroyed bottom keratinocytes
- Creates band-like inflammation
- Cannot see where dermis finished, and epidermis starts
What is the diagnosis of this patient who also has white lines in their mouth?

Lichen planus
What is Pyoderma gangrenosum?
Vasculitis that presents as non-healing ulcer
- Often, first manifestation of a systemic disease
- Colitis, hepatitis, leukaemia
What is the diagnosis?

Pyoderma gangrenosum
What is Seborrhoeic keratosis?
Benign, pigmented lesion that has a stuck on appearance (often gets caught on clothing)
What is the diagnosis?

Seborrhoeic keratosis
What is a Sebaceous cyst?
A swelling in the skin arising in a sebaceous gland, typically filled with yellowish sebum
- The cyst transluminates, has a central punctum and is circumscribed and hot
Describe the appearance of Basal cell carcinomas?
- Rolled, pearly-edge
- Central ulcer
- Telangiectasia
- “Rodent ulcer” as it burrows away
Why can’t BCC metastasise?
Cancer cannot break through the basement membrane
What is the most common mutation in BCC?
PTCH
Where are BCC most commonly found?
Sun-exposed areas of skin
What should be suspected if a BCC develops in a young person?
Gorlin’s syndrome
What is the diagnosis?

Basal cell carcinoma
What is Bowen’s disease?
- Squamous cell carcinoma in situ [i.e. pre-cancerous]
- Keratinocytes become more pleiomorphic and larger with mitotic figures
Describe the appearance of Squamous cell carcinoma.
Rough, scaly surface and flat reddish patches
Can SCC metastasise?
- Very very very rarely
- More commonly Peri-neural invasion - Local invasion
What do SCC’s look like under the microscope?
Pink due to lots of keratin
What is the diagnosis?

Squamous cell carcinoma
What are Café-au-lait spots?
- A common birthmark, presenting as a hyperpigmented skin patch with a sharp border and diameter of > 0.5 cm
- A form of melanocytic naevus
What is the diagnosis?

Café-au-lait spots
What is Junctional nevus?
- Melanocytes nest in the epidermis
- Flat and coloured
- Normally, melanocytes sit in the basal layer of the epidermis
- As you age, melanocytes usually drop into the dermis
What is Compound nevus
Nests in epidermis and dermis
- Raised area
- Surround by flat pigmented area
What is Intradermal naevus?
- Nests in the dermis
- Raised area
- Skin-coloured or pigmented
Describe the appearance of Melanoma?
- Irregular border
- Variable pigmentation
- Bleeding
- Itchy
- Growing
What is the most common mutation in Melanoma?
- B-raf 600
- Found in 60%
- Is a target for treatment - B-raf inhibitors
Define Asthma.
Widespread reversible narrowing of the airways that changes in severity over short periods of time.
What are the causes of asthma?
- Allergens/atopy
- Pollution
- Drugs (NSAIDs)
- Occupational (gases/fumes)
- Diet
- Physical exertion
- Intrinsic
- Underlying Genetics
What is the pathogenesis of Asthma?
- Sensitisation to allergen; followed by:
- Immediate phase = mast cell degranulation causing mediator release whihc increases vascular permeability, eosinophil and mast cell recruitment and bronchospasm
- Late phase = tissue damage, increased mucous production, muscle hypertrophy
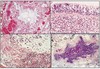
What is the histology of Asthma?
- Hyperaemia (Top left)
- Eosinophils and goblet cell hyperplasia (Top right)
- Hypertrophic constricted muscle (Bottom left)
- Mucus plugging and inflammation (Bottom Right)
Define COPD
Chronic inflammatory lung disease that causes obstructed airflow from the lungs
What are the causes of COPD?
- Smoking
- Air Pollution
- Occupational exposure
- A1AT deficiency
- Rare (IVDU, connective tissue disease)
What is the histology of COPD?
- Dilatation of airways
- Hypertrophy of mucous glands
- Goblet cell hyperplasia
What are the complications of COPD?
- Repeat infections
- Chronic hypoxia/Reduced exercise tolerance
- Pulmonary Hypertension/RHF
- Lung cancer risk
Define Bronciectasis.
Permanent abnormal dilatation of the terminal bronchi.
What are the causes of bronchectasis?
- Congenital
- CF
- Ciliary dyskinesia - i.e. Kartagener’s syndrome
- Inflammatory
- Post-infectious
- Obstruction
- 2nd to bronchiolar disease and interstitial fibrosis
- Asthma
What are the complications of Bronchiectasis?
- Recurrent infections
- Haemoptysis
- Cor pulmonale
- Amyloidosis
Define Cystic Fibrosis.
A hereditary disorder affecting the exocrine glands
It causes the production of abnormally thick mucus, leading to the blockage of the pancreatic ducts, intestines, and bronchi and often resulting in respiratory infection.
What is the pathophysiology of CF?
- CFTR gene on Chr 7
- Abnormal CFTR causess defective Cl- ion transfer so less water transfer to secretions
- Leads to thick secretions which are hard to clear
What are the signs and symptoms of CF?
- Lung
- Cough
- Purulent Secretions that is foul smelling
- Obstruction
- Respiratory failure
- Recurrent infection
- Bronchiectasis (90%)
- GI tract
- Meconium ileus
- Malabsorption
- Pancreas
- Pancreatitis
- 2nd malabsorption
- Liver
- Cirrhosis
- Male infertility
What treatments exist for CF?
- Physio
- Trikafta - elexacaftor, tezacaftor, and ivacaftor
- Antibiotics - Broad spectrum or Aminoglycosides
- Lung transplant
What are the most common causative pathogens in patients with CF?
- P. aeruginosa - most common
- S. aureus - most common in very young
- H. influenzae
- B. cepacia
What are the causes of Pulmonary oedema?
- LHF
- Alveolar injury
- Neurogenic
- High altitude
Define ARDS/RDS.
Acute damage to endothelium ± alveolar epithelium leading to an exudative inflammatory reaction
What are the causes of ARDS in adults?
- Infection
- Aspiration
- Trauma
- Inhaled irritant
- Shock
- Blood transfusion
- DIC
- Drug overdose
- Pancreatitis
What are the causes of Hyaline membrane disease of the newborns?
Insufficient surfactant - most commonly due to premature briths
What is the pathology of ARDS?
- Basic pathology = Diffuse alveolar damage
- Gross pathology:
- Fluffy white infiltrates in all lung fields
- Lungs expanded/firm
- Plum-coloured lungs, airless
- >1kg mass
- Micro-pathology:
- Capillary congestion
- Exudative phase
- Hyaline membranes
- Organising phase
What is the likely cause of death of this patient?

ARDS
What are the 4 types of bacteria pneumonia?
- Bronchopneumonia
- Lobar pneumonia
- Abscess formation
- Granulomatous inflammation
What is bronchopneumonia?
Patchy bronchial and peribronchial distribution, lower lobes, inflammation surrounding the airways themselves and is within the alveoli
What kind of pathogens cause bronchopneumonia?
- Low virulence organisms
- Staph
- H. influenzae
- Strep
- Pneumococcus
What is lobar pneumonia?
Infection of an entire lobe
- Infrequent due to Abx
What is the predominant cause of lobar pneumonia?
Pneumococci - Strep
What are the stages of lobar pneumonia?
- Congestion - Hyperaemia, Intra-alveolar fluid
- Red hepatization - Hyperaemia, Intra-alveolar neutrophils
- Grey hepatization - Intra-alveolar connective tissue
- Resolution - Restoration normal architecture
What are the complications of lobar pneumonia?
- Abscess
- Pleuritis
- Effusion
- Empyema (infected effusion)
- Fibrosis
- Sepsis
What are the causes of atypical pneumonia?
- Mycoplasma
- Viruses (CMV, influenza)
- Coxiella
- Chlamydia
- Legionella
What is COPD - emphysema?
Permanent loss of alveolar parenchyma distal to terminal bronchiole
What are the complications of COPD - emphysema?
- Bullae formation - Pneumothoraces
- Respiratory failure
- Cor pulmonale
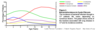
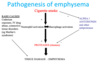
What is the pathogenesis of emphysema?
Describe Bullous emphysema.
- Irreversible enlargement of airspaces distal to terminal bronchioles
- No scarring/fibrosis
- Impaired gaseous exchange
- Dyspnoea
- Pneumothorax if vullae rupture
- Pulmonary hypertension - Cor pulmonale/RHF
Define Granuloma.
Collection of histiocytes, macrophages ± giant multinucleate cells
What are the causes of granulomatous lung disease?
- Infection
- TB must first be excluded before looking for other causes
- Fungal = histoplasma, cryptococcus, coccidioides, aspergillus, Mucor
- Other = pneumocystis, parasites
- Sarcoidosis
- Foreign body aspiration
- IVDU
- Drugs
- Occupational
Define Sarcoidosis.
Abnormal host immunological response to variety of commonly encountered antigens, probably environmental in origin, resulting in granuloma formation
What organs are commonly affected by sarcoidosis?
- Lungs
- Skin
- Lymph nodes
- Eyes
What is the pathophysiology of lung involvement in sarcoidosis?
- Discrete epithelioid and giant cell granulomas, preferential distribution in upper zones with a tendency to peri-lymphatic and peri-bronchial
- In advanced disease becomes fibrocystic
What test results indicate sarcoidosis?
- X-ray/CT = Non-caseating granuloma
- Bloods:
- Elevated serum ACE
- Hypercalcaemia (1a-hydroxylase)
What is the pathology of Idiopathic pulmonary fibrosis?
- Macro = basal and peripheral fibrosis and cyst formation
- Micro = interstitial fibrosis (varying stages)
How does the progression of disease differ in Idiopathic pulmonary fibrosis and Extrinsic allergic alveolitis?
- IPF = Progressively gets worse regardsless - 50+% die within first 3 years
- EAA = Gets beter when away from causative allergen
- Farmer’s lung - patient gets better over the weekend when they are away from work
What are the causes of Industrial lung disease/Pneumoconiosis?
- Asbestos - Asbestosis
- Silicon - Silicosis
- Coal - Coal-miner’s lung
What are the features of Asbestosis?
- Fine sub-pleural basal fibrosis with asbestos bodies in tissue
- ± pleural disease - fibrosis, pleural plaques
- Increased risk of lung cancer
What are the causes of Pulmonary hypertension?

What alternative causes of embolism than thromboembolism?
- Bone marrow
- Amniotic fluid
- Trophoblast
- Tumour
- Foreign body
- Air
- Fat
What are the consequences/symptoms of a PE?
- Small emboli:
- Pleuritic chest pain or chronic progressive SoB due to pulmonary HTN
- Repeated emboli will cause increasing occlusion of pulmonary vascular bed and pulmonary HTN
- Large emboli:
- Occlude main pulmonary tract (saddle embolus is possible) - sudden death/RHF/shock
- 30% will develop a second embolus
How does Pulmonary vasculitis present?
- Life threatening haemorrhage
- Chronic haemoptysis
- Mass lesion
- Interstitial lung disease
What are the types of benign lung tumours?
Chondroma
What are the types of malignant tumours?
- Squamous cell carcinoma (30%)
- Adenocarcinoma (30%)
- Large cell carcinoma (20%)
- Small Cell Lung Carcinoma (20%)
What are the risk factors for lung cancer?
- Smoke = strongest association with SCC and SCLC
- Other Risk Factors (25% of lung cancers are in non-smokers):
- Asbestos
- Radiation (radon exposure)
- Air pollution
- Heavy metals
- Genetics (familial lung cancers are rare)
- Susceptibility genes:
- Chemical modification of carcinogens
- Susceptibility to chromosomal damage
- Nicotine addiction
What components in cigarettes cause cancer?
- Tumour initiators - Polycyclic aromatic hydrocarbons
- Tumour promoters - Nicotine
- Complete carcinogens - Nickel, Arsenic
Which lung cancer is most common in non-smokers?
Adenocarcinoma
Describe the development of carcinoma?
- Metaplasia - Dysplasia - Carcinoma in situ - Invasive carcinoma
- Due to an accumulation of gene mutations

What occurs in the lungs that means resilient squamous epithelium still develop cancer?
- It does NOT have cilia
- Build-up of mucus as no cilia are present to sweep it away
- Within this mucus, you will get loads of carcinogens
- More carcinogens accumulate, hence the increased risk of cancer formation
What are the features of Squamous Cell Carcinoma (SCC)?
What is the pattern of progression in Adenocarcinoma?
Atypical adenomatous hyperplasia - Adenocarcinoma in-situ - Invasive adenocarinoma

What mutations occur that cause adenocarcinoma of the lung and why is this important?
- Smokers = K-ras, issues with DNA methylation and p53
- Non-smokers = EGFR mutations
- Are drug targets
What are the features of Pulmonary Adenocarcinoma?
- Peripheral/Terminal airways with multi-centric pattern
- Incidence is increasing
- More common in Females, Far East and Smokers (is the most common in non-smokers)
What will histology of adenocarcinoma show?
- Glandular differentiation
- Gland formation
- Papillae formation
- Mucin

What are the features of Large cell carcinoma?
- Poorly differentiated tumours composed of large cells
- There is no histological evidence of glandular or squamous differentiation
- Poor prognosis
What are the features Small cell lung cancer (SCLC)?
- Very close association with smoking
- Often CENTRAL and near the bronchi
- 80% will present with advanced disease
- Very chemosensitive but very poor prognosis - worst of any lung cancer
- May cause paraneoplastic syndromes (i.e. SIADH)
What is the histology of Small cell lung cancer?
- Small poorly differentiated cells
- Common mutations: p53, RB1
What is the cytology of Small cell lung cancer?
- Small cells
- Ciliated normal respiratory cell

What are the survival rates of Small cell lung cancer vs Non-small cell lung cancer?
- Small Cell Lung Cancer
- Survival 2-4 months if untreated; 10-20 months on treatment
- Chemoradiotherapy mainstay
- Survival 2-4 months if untreated; 10-20 months on treatment
- Non-Small Cell Lung Cancer:
- Early/Stage 1 tumours have 60% 5-year survival; Late/Stage 4 at 5% 5-year survival
- Less chemosensitive
- Early/Stage 1 tumours have 60% 5-year survival; Late/Stage 4 at 5% 5-year survival
What tissue is needed for cytology and histology?
- Cytology – looking at cells:
- Sputum
- Bronchial washings and brushings
- Pleural fluid
- Endoscopic fine needle aspiration of tumour/enlarged lymph nodes
- Histology – looking at tissue:
- Biopsy at bronchoscopy – central tumours
- Percutaneous CT guided biopsy – peripheral tumours
- Mediastinoscopy and lymph node biopsy – for staging
- Open biopsy at time of surgery if lesion not accessible otherwise - frozen section
- Resection specimen - confirm excision and staging
What are the features of Mesothelioma?
- Malignant tumour of the pleura
- Essentially fatal (poor prognosis)
- There is a long lag/tumours develop decades after asbestos exposure
- <1% of cancer deaths but increasing incidence with a peak predicted in around 2010-2020
- More common in males: female (3: 1)
- 50-70 years
What paraneoplastic syndromes exist?
- Endocrine:
- SIADH
- Causes hyponatremia
- Especially common with SCC
- Cushing’s syndrome
- Especially SCC
- Hypercalcaemia due Parathyroid hormone-related peptide
- Especially SCC
- Calcitonin - Hypocalcaemia
- Gonadotropins - Gynecomastia
- Carcinoid syndrome
- Secretions of serotonin
- Especially common in carcinoid tumours
- SIADH
- Non-endocrine:
- Haematologic/coagulation defects
- Skin
- Muscular
- Miscellaneous disorders
What investigations are done in breast triple testing?
- Clinical examination
-
Imaging (sonography, mammography, MRI)
- MRI tends to only be used for very small lesions
- Pathology (cytopathology and/or histopathology) – either FNA or core biopsy
What are the codings for cytology?
- C1 = inadequate
- C2 = benign
- C3 = atypia, probably benign
- C4 = atypia, probably malignant
- C5 = malignant
What is duct ectasia and how does it usually present?
Benign inflammation and dilatation of large breast ducts
- Usually presents with nipple discharge
- May cause breast pain, breast mass and nipple retraction
What is the cytology and histology of duct ectasia?
- Cytology
- Proteinaceous material and neutrophils
- Histology
- Duct distension with proteinaceous material in it
- Foamy macrophages

What is acute mastitis and how does it usually present?
Acute inflammation in the breast
- Painful/tender
- Red/erythematous breast
- Often seen in lactating women due to cracked skin and stasis of milk
- May complicate duct ectasia
- Usual organism: staphylococci
What is the cytology of acute mastitis?
Neutrophils

What is the treatment of acute mastitis?
Drainage and Antibiotics
What is fat necrosis and how does it usually present?
Benign inflammatory reaction to damaged adipose tissue
- Breast mass
- Causes = trauma, surgery, radiotherapy
What is the cytology of fat necrosis?
Fat cells surrounded by macrophages

What is fibrocystic disease of the breast and how does it usually present?
Benign group of alterations which reflect normal, albeit exaggerated, responses to hormonal influences
- Breast lump - presentation
- Very common
- No increased risk for subsequent breast carcinoma
What is the histology of fibrocystic disease of the breast?
Ducts dilated and calcified

What is fibroadenoma of the breast and how does it usually present?
Benign fibroepithelial neoplasm of breast
- Presentation
- Well circumscribed mobile breast lump
- Young women - 20-30yo
- Common
What is the histology of fibroadenoma of the breast?
Glandular and stromal cells

What is phyllodes tumour of the breast and how does it usually present?
A group of potentially aggressive fibroepithelial neoplasms of the breast
- Presentation
- Enlarging mass in women >50 years
- Some may arise within pre-existing fibroadenomas
- Uncommon
- Vast MAJORITY are BENIGN (but a small proportion can behave aggressively (malignant phyllodes))
What is the histology of phyllodes tumour of the breast?
- Overlapping cell layers, cellularity
- Level of malignancy determined on cellularity of the stroma
- High cellularity + stromal overgrowth = malignant

What is intraductal papilloma and how does it usually present?
Benign papillary tumour arising within the duct system of the breast
- Arises within the:
- Small terminal ductules = peripheral papilloma
- Can often remain clinically silent
- Large lactiferous ductules = central papilloma
- Present with bloody nipple discharge
- Small terminal ductules = peripheral papilloma
- Common - mainly in 40-60 years
What is the cytology and histology of intraductal papilloma?
- Cytology
- Clusters of cells
- Potential increased risk with multiple papillomas of carcinoma
- Histology
- Dilated ducts
- Polypoid mass in the middle
- Fibrovascular core
- Blood vessels within the stroma

What is the treatment of intraductal papilloma?
Excision of duct
What is radial scar of the breast and how does it usually present?
Benign sclerosing lesion characterised by a central zone of scarring surrounded by a radiating zone of proliferating glandular tissue
- Presentation
- Stellate masses on screening mammograms - may closely resemble carcinoma
- Range in size from microscopic to large
- Lesions >1 cm = complex sclerosing lesions
What is the histology of radial scar of the breast?
- Central stellate area
- Peripheral proliferation of ducts and acini

What is Proliferative Breast Disease?
Diverse group of microscopic intraductal proliferative lesions of the breast associated with an increased risk of subsequent development of invasive breast carcinoma but produce no symptoms
- Usual epithelial hyperplasia
- Marker of slightly increased risk of breast cancer
- Flat epithelial atypia/atypical ductal carcinoma
- FEA may represent the earliest morphological precursor to low grade ductal carcinoma in situ
- 4 x increased risk of developing cancer
- In situ lobular neoplasia
- Associated with a 7-8x increased risk of invasive breast carcinoma

Define Ductal Carcinoma in situ.
Neoplastic intraductal epithelial proliferation with risk of progression to breast cancer.
How does ductal carcinoma in situ usually present?
- Common
- 85% are detected on mammography - microcalcification
- 10% will produce clinical features - lump, Paget’s disease
- 5% diagnosed incidentally
What is the histology of ductal carcinoma in situ?
- Low → “cribriform / punched-out DCIS”
- Lumens compact/regular
- Calcification
- Overlapping cells
- High
- Central lumen necrotic material
- Large cells
- Pleiomorphic cells occlude the duct
- Few lumens

What is the treatment of ductal carcinoma in situ?
Surgical excision - chemo is very rarely given
What is the prognosis of ductal carcinoma in situ?
- Recurrence - more likely with high grade or extensive disease
Define Invasive Breast Carcinoma.
A group of malignant epithelial tumours which infiltrate within the breast and have the capacity to spread to distant sites.
What is the most common cancer in women?
Invasive breast carcinoma → 1 in 8 women
What are the risk factors for invasive breast carcinoma?
- Early menarche/Late menopause
- Age
- Obesity
- Alcohol
- OCP
- FHx (5% inheritance)
- Genetics → BRCA mutations (up to 85% increased lifetime risk)
What are the genetic pathways that lead to invasive breast cancer?
- Low Grade = arise from low grade DCIS or in situ lobular neoplasia and show 16q loss
- High Grade = arise from high grade DCIS and show complex karyotypes with many unbalanced chromosomal aberrations
What are the presenting features of invasive breast carcinoma?
Breast lump
What is the histology and cytology of invasive ductal carcinoma?
- Pleiomorphic cells with large nuclei
- E-cadherin +ve

What is the histology and cytology of invasive lobular carcinoma?
- Linear (‘Indian File’ pattern)
- Monomorphic (look similar)

What is the histology and cytology of invasive tubular carcinoma?
Elongated tubules invading the stroma

What is the histology and cytology of invasive mucinous carcinoma?
Empty spaces contain lots of mucin

Define Basal-like Carcinoma.
Carcinoma type discovered following genetic analysis of breast carcinomas
What is the histology, immunohistochemistry and any other distinct features of basal-like carcinoma?
- Histology
- Sheets of markedly atypical cells
- Prominent lymphocytic infiltrate
- Central necrosis
- Immunohistochemistry
- +ve for “basal” cytokeratins CK5/6 and CK14
- Associated with BRCA mutations
- Propensity for vascular invasion and metastasis
What is the histological grading of breast cancer?
- Grading is dependent on
- Tubule formation → 1, 2, 3
- Nuclear pleomorphism → 1, 2, 3
- Mitotic activity → 1, 2, 3
- Graded up to score from 3 to 9
- 3-5 = grade 1 = well differentiated
- 6-7 = grade 2 = moderately differentiated
- 8-9 = grade 3 = poorly differentiated
What receptor statuses are in invasive breast cancers?
- All invasive breast cancers are assessed for
- Oestrogen receptor (ER)
- Progesterone receptor (PR)
- Her2 receptor
- Phenotype:
- Low grade = ER/PR positive and Her2 negative
- High grade = ER/PR negative and Her2 positive
- Basal-like Carcinomas = ER/PR/Her2 negative - triple negative
What is the most important prognostic factor in invasive breast carcinoma?
- The status of the axillary lymph nodes
- Other factors
- Size
- Histological type
- Histological grade
Describe the NHS Breast Screening Programme.
- Women aged 47-73 years are screened every 3 years
- The screening test is a mammogram
- 5% will have an abnormal mammogram → recalled for further investigation
- Further investigation may include FNA/biopsy or further scans
Define gynaecomastia.
Enlargement of the male breast - benign
Describe gynaecomastia.
- Affects pubertal boys and men >50 years
- Idiopathic or associated with drugs - therapeutic and recreational
- Histology
- Epithelial hyperplasia of ducts with finger-like projections extending to duct lumen
- Periductal stroma often cellular and oedematous
Describe Breast Cancer.
- Rare
- Median age = 65 years
- Presentation = palpable lump
- Histologically similar to female breast cancers
What are the congenital disorders of the bowel?
- Atresia
- Duplication
- Imperforate anus - closed anus
What is Hirschsprung’s disease?
Congenital absence of ganglion cells in myenteric plexus → distal colon fails to dilate

What are the signs and symptoms of Hirschsprung’s disease?
- Constipation
- Abdominal distension
- Vomiting
- Overflow Diarrhoea
- Male - 80%
What are associated with Hirschsprung’s disease?
- Down’s syndrome (2%)
- RET proto-oncogene Cr10+ and others
What are the appropriate investigations for suspected Hirschsprung’s disease?
- Clinical impression - child/baby not going to the toilet normally
- Biopsy - hypertrophied nerve fibres but no ganglia
What are the treatment for Hirschsprung’s disease?
Resection of affected segment - frozen section used to ensure full removal
What are the mechanical causes of bowl pathology?
- Obstruction
- Adhesions
- Herniation
- Extrinsic mass
- Volvulus
- Diverticular disease
What are the most commonly affected sites of volvulus?
- Infants = Small bowel
- Sigmoid = Elderly
What is the diagnosis?

Volvulus
What is the diagnosis?

Diverticular disease
What is the diagnosis?

Diverticular disease
What is the diagnosis?

Diverticular disease
What are the complications of diverticular disease?
- Pain
- Diverticulitis
- Gross perforation
- Fistula - bowel, bladder, vagina
- Obstruction
What are the inflammatory causes of bowl pathology?
- Acute
- Infection
- Drug/toxin
- Chemo
- Radiation
- Chronic
- Crohn’s
- UC
- TB
What is Pseudomembranous colitis?
- Antibiotic associated → C. diff
- Caused by protein exotoxins of C. diff
What is the diagnosis?

Pseudomembranous colitis → think of wet cornflakes in the bowel - pseudomembrane
What is the management of pseudomembranous colitis?
- Stop causing antibiotic
- Vancomycin or Metronidazole
- Supportive measures
What is the diagnosis?

Pseudomembranous colitis → volcanic eruption of pus
What are the most common sites for ischaemic colitis?
- Watershed segments - inbetween/end of blood supply
- Splenic flexure - SMA and IMA
- Rectosigmoid - IMA and interal iliac artery
What are the causes of ischaemic colitis?
- Arterial occlusion
- Venous obstruction
- Small vessel disease - DM, cholesterol, vasculitis
- Low flow state - CCF, haemorrhage, shock
- Obstruction - hernia, intussusception, volvulus, adhesions
What is the diagnosis?

Ischaemic bowel
This slide is taken from the bowel. What is the diagnosis?

Ischaemic bowel
What are the signs and symptoms of IBD?
- Diarrhoea - can have blood in it
- Fever
- Abdominal pain
- Acute abdomen
- Anaemia
- Weight loss
- Extra-intestinal manifestations
What are the risk factors for IBD disease?
- Western population - White 2-5 times higher than non-white
- Higher incidence in Jewish population
- Peak onset in teens to twenties
- Smoking
- UC is slightly more common than Crohn’s
What are the pathological features of Crohn’s?
- Whole GI tract affected
- Skip lesions
- Cobblestone mucosa
- Transmural inflammation
- Non-caseating granulomas
- Sinus/fistula/fissure/abscess formation
- Fat wrapping
- Thick ‘rubber hose’ like wall
- Narrow lumen
What are the pathological features of UC?
- Starts at rectum and move contiguously
- Only affects rectum and large bowel
- Can get backwash damage to ileum and appendix
- Only affects rectum and large bowel
- Inflammation confined to nucosa
- Normal bowel wall thickness
- Shallow ulcers
What are the extra-intestinal manifestations of Crohn’s?
- Arthritis
- Uveitis
- Stomatitis/cheilitis
- Skin lesions
- Pyoderma gangrenosum
- Erythema multiforme
- Erythema nodosum
What is the diagnosis?

Crohn’s
What is the diagnosis?

Crohn’s
What is the diagnosis? This is taken from the bowel.

Crohn’s - Look at granuloma
What are the complications of UC?
- Severe haemorrhage
- Toxic megacolon
- Adenocarcinoma - 20-30x risk
What are the extra-intestinal manifestations of UC?
- Arthritis
- Muositis
- Uveitis/iritis
- Erythema nodusum
- Puoderma gangrenosum
- PSC
What is the diagnosis?

UC
What is the diagnosis?

UC
What are the tumours of the colon and large bowel?
- Non-neoplastic polyps
- Neoplastic epithelial lesions
- Adenoma
- Adenomacarcinoma
- Carcinoid tumour
- Mesenchymal lesions
- Stromal tumours
- Lipoma
- Sarcoma
- Lymphoma
What types of polyps are found in the colon and rectum?
- Non-neoplastic
- Hyperplastic
- Inflammatory - pseudo-polyps
- Haramtomatous
- Neoplastic
- Tubular adenoma
- Tubulovillous adenoma
- Villous adenoma
What is the diagnosis?

Hyperplastic polyp
What is the diagnosis?

Adenoma
What is the diagnosis?

(Tubular) adenoma
What is the diagnosis?

Tubular adenoma
What is the diagnosis?

Villous adenoma
What is the diagnosis?

(Villous) adenoma
What are the polyp risk factors for cancer?
- Size - >4cm = 45% have invasive malignancy
- Proportion of villous component
- Degree of dysplastic change within polyp
What familial syndrome increase your risk of adenoma and therefore adenocarcinoma of the bowel?
- Familial adenomatous polyposis (FAP)
- Gardner’s
- Turcot
- HNPCC
- Peutz Jeghers
Describe FAP.
- Autosomal dominant - average onset = 25
- Adenomatous polyps
- Average 1,000 polyps - minimu is 100
- Chromosome 5q21 (APC tumour suppressor gene)
- 100% will develop cancer within 10-15 years
What is the diagnosis?

FAP
Describe HNPCC.
- Autosomal dominant
- 3-5% of all colorectal cancers
- Multiple cancer presenting together → endometrial, prostate, breast, stomach
- Often poorly differentiated
- 1 of 4 DNA mismatch repair genes mutated
- Numerous DNA replication errors
What are the risk factors for colorectal carcinoma?
- Low fibre, high fat diet
- Lack of exercise
- Obesity
- Smoking
- Familial disease
- FHx
- IBD
What is the diagnosis?

Colorectal carcinoma - some small polyps to the right
What is the diagnosis?

Ulcerating cancer of the anus
What is the diagnosis?

Carcinoma
What are the signs and symptoms of colorectal cancer?
- Bleeding
- Change in bowel habit
- Anaemia
- Weight loss
- Pain
- Fistula
What Staging is used in colorectal carcinoma?
- Duke’s
- A = confined to wall of bowel
- B = through wall of bowel
- C = lymph node mets
- D = distant mets
- TNM is most commonly used in all carcinoma
What opportunistic diseases do HIV patients get?
- Pneumocystis jiroveci → PCP pneumonia
- CMV → especially retina and GIT
- Stains brown in immunohistochemistry
- Candida
- Tuberculosis and atypical mycobacteria
- Cryptococcus → meningitis
- Toxoplasma gondii → encephalitis and mass lesions
- JC papovavirus → progressive multifocal leukoencephalopathy
- Herpes simplex
- Cryptosporidium, Isospora belli, microsporidia → GIT
What tumours are HIV patients at risk of?
- Kaposi’s sarcoma - HHV-8
- Dermis expanded by a solid tumour
- Made of spindle-shaped cells – infiltrated by HHV-8
- HHV-8 identified in nuclei of tumour cells
- Lymphoma
- Systemic
- B-cell lymphoma
- EBV
- SSC
- Anus & cervix
- HPV
What central nervous system diseases are HIV patients at risk of?
- Progressive encephalopathy = AIDS dementia complex
- Opportunistic infections and tumours
- CNS lymphoma
What organs are affected by mycobacterial infections?
- Lung
- Lymph nodes
- Bone
- Heart
- GIT
- CNS
What are the characteristics of sarcoid diseases?
- Non-caseating granulomas = collection of macrophages with a cuff of lymphocytes around
- Diagnosed as a diagnosis of exclusion

What organs are affected by sarcoid diseases?
- Lung
- Lymph nodes
- Spleen
- Liver
- Heart
- Joints
- Basement membranes
- Skin
- Eyes
- CNS
- Salivary glands
What are the characteristics of IgG4-related diseases?
- Inflammation dominated by IgG4-AB producing plasma cells
-
Fibrosis and obliteration of veins
- Plasma cell rich inflammatory infiltrate
- Immunohistochemistry for IgG4
Name some IgG4-related diseases.
- Salivary and lacrimal glands: Mikulicz syndrome
- Thyroid: Riedel thyroiditis
- Peritoneum: Retroperitoneal fibrosis
- Liver: Biliary obstruction
- Pancreas: Autoimmune pancreatitis
- Mass lesions: Inflammatory pseudotumour
What conditions are caused by alcohol?
- Liver
- Fatty change/Steatosis
- Steatohepatitis
- Cirrhosis
- Hepatocellular carcinoma
- GI Tract
- Acute gastritis
- Oesophageal varices
- Oral cavity and oesophagus cancers
- Nervous system
- Peripheral neuropathy
- Wernicke-Korsakoff syndrome
- Cardiovascular system
- Dilated cardiomyopathy
- Hypertension
- Atheroma
- Pancreas
- Acute pancreatitis
- Chronic pancreatitis
- Cancer
- Pharynx
- Breast
- Foetal alcohol syndrome
What organs are affected in cystic fibrosis?

Describe amyloid.
- Deposition of an abnormal proteinaceous substance in non-branching fibrils - 7.5-10nm diameter
- Always contains P-component
- Beta-pleated sheet structure
- A variety of proteins can take on this conformation
- Resistant to enzymic degradation
What is the classification of amyloid?
- First classification:
-
AA – derived from serum amyloid A
- Chronic inflammatory diseases - RhA, Crohn’s Disease
-
AL – derived from light chains
- Multiple myeloma, B cell lymphoma
-
AA – derived from serum amyloid A
- Second classification:
- Transthyretin - e.g. mutation
- Beta2-macroglobulin – peritoneal dialysis
- Abeta2 protein – Alzheimer’s
- Insulin, calcitonin – endocrine tumours
What staining can be used for amyloid?
- Stains with Congo Red Dye
- Shows apple-green birefringence under polarised light

What are the clinical effects of amyloid?
- Proteinuria, renal failure
- Restrictive cardiomyopathy, arrhythmias
- Autonomic neuropathy
- Carpal tunnel syndrome
- Macroglossia
- Bleeding on injury
- Also deposited in blood vessels, endocrine organs, liver, spleen
What is the normal structure of the oesophagus?
- Z-line = the point at which epithelium transitions from being squamous to columnar
- Submucosal glands are an important feature of the oesophagus

What is the normal structure of the stomach?
Layers = Mucosa (epithelium → lamina propria → muscularis mucosa) → submucosa → muscularis propria

What is the normal structure of the duodenum?

What is the most common cause of acute oesophagitis?
GORD
What is the histological findings in acute oesophagitis?
Lots of neutrophils
What are the complcations of acute oesophagitis?
- Ulceration
- Fibrosis
- Haemorrhage
- Perforation
- Stricture
- BARRETT’S OESOPHAGUS
What is the histology of ulceration?
- Necrotic slough
- Inflammatory exudate
- Granulation tissue
In terms of the GIT what is the difference between ulceration and erosion?
- Ulcer = past muscularis mucosa into submucosa
- Erosion = before muscularis mucosa - not into submucosa
What is Barrett’s oesophagus / CLO?
Classic metaplastic process = squamous epithelium of lower oesophagus replaced by columnar epithelium
- Two main types:
- CLO - metaplasia without goblet cells = gastric metaplasia
- CLO with IM - metaplasia with goblet cells (intestinal metaplasia) → higher cancer risk

Describe squamous cell carcinoma of the oesophagus.
- Upper 2/3rd
- Associations = smoking and alcohol
What is the histology of squamous cell carcinoma of the oesophagus?
- Invades submucosa
- Cells form keratin = defining feature
- Cells have intercellular bridges
Describe adenocarcinoma of the oesophagus.
- Most common oesophageal cancer
- Bottom 1/3rd
- Associations = GORD, Barrett’s oesophagus
What is the histology of adenocarcinoma of the oesophagus?
- Glandular epithelium
- Mucin
What are the causes of acute gastritis?
- Chemical
- Aspirin/NSAIDs
- Alcohol
- Corrosives
- Infective
- H. pylori
- CMV
- Strongyloides
What are the causes of chronic gastritis?
- Autoimmune
- Bacterial
- H. pylori
- (CMV
- Strongyloides
- Chemical
- NSAIDs
- Bile reflux
- D = IBD
What investigative finding can differentiate between acute and chronic gastritis?
- Acute = Neutrophils
- Chronic = Lymphocytes
- Can have co-existing neutrophils and lymphocytes if acute on chronic
Define Mucosa Associated Lymphoid Tissue (MALT).
Chronic gastritis associated with H. pylori infection induces lymphoid tissue in the stomach.
- Increased risk of lymphoma
Define Gastric Ulcer.
Erosion where depth of the loss of tissue goes beyond the muscularis mucosa (into the submucosa).
What is the difference between chronic and acute ulcers?
- Fibrosis
- Acute = -ve
- Chronic = +ve
- If no fibrosis ulcer can heal
What investigations must be done for all gastric ulcers?
Biopsy → exclude malignancy
What are the complications of gastric ulcers?
- Bleeding → anaemia, shock (massive haemorrhage)
- Perforation → peritonitis
Define Gastric Intestinal Metaplasia.
Presence of goblet cells in the mucosa of the stomach - occurs in response to long term damage.
Define Gastric Epithelial Dysplasia.
Abnormal epithelial pattern of growth with some cytological / histological features of malignancy but no invasion through the basement membrane.
- Cancer = invasion through the BM
What are the risk factors for gastric cancer?
- Male
- Race - more common in Japan, Chile, Italy, China, Portugal and Russia - probably diet related
- Host genetic factors
- Bacterial virulence factors (i.e. Cag-A)
- Environmental factors
- Gastric cancer phenotypes
What are the types of gastric adenocarcinoma?
-
Intestinal = well-differentiated
- Mucin-containing big glands
-
Diffuse = poorly differentiated
- Composed of single cells with no attempt at gland formation
- Types = Linitis plastica, Signet ring cell carcinoma (spreads all over stomach)
What are the types of gastric cancers?
- Adenocarcinoma - 95%
- Intestinal or Diffuse
- Squamous cell carcinoma
- Lymphoma = MALToma - B-cell NHL
- Gastrointestinal stromal tumour
- Neuroendocrine tumours
What is a MALToma?
-
H. pylori as well as lymphoma
- Will see crypts that are full of neutrophils
- Good because if you treat H. pylori, the lymphoma could be reversed → CAP (Clarithromycin, Amoxicillin, PPI)
What pathogens cause duodenitis and/or duodenal ulcers?
- H. pylori
- CMV
- Cryptosporidium
- Giardia lamblia
- Whipple’s disease → Tropheryma whippelii (parasites)
How does H. pylori cause duodenitis and/or duodenal ulcers?
- Increased acid in the antral-predominant strain that spills into duodenum + less duodenal HCO3-
- Chronic inflammation leads to gastric metaplasia with H. pylori
- Chronic inflammation can also lead to duodenal ulceration
- H. pylori → many gastric ulcers
- H. pylori → 100% of duodenal ulcers
What architectural changes occur in Coeliac’s disease?
- Loos of villi
- Crypt hyperplasia
- Inflammatory changes → increased intraepithelial lymphocytes
What is Lymphocytic duodenitis?
Inflammatory changes (increased intraepithelial lymphocytes) without architectural changes
- Many people with this either have Coeliac’s or are going to develop Coeliac’s
What are the appropriate investigations for suspected Coeliac’s disease?
- Antibodies:
- Endomysial Antibodies- anti-EMAs
- Tissue Transglutaminase Antibodies - anti-TTG
- Duodenal Biopsy
- On gluten rich diet = villous atrophy
- Off gluten rich diet = normal villi
What disease causing malabsorption has a similar histology to coeliac disease?
Tropical sprue
Describe duodenal lymphoma/MALoma.
- MALTomas associated with coeliac disease
- Found in the duodenum
- Are T cell lymphomas / EATL
- Lymphomas in the stomach due to H. pylori are B cell lymphomas
Define Cerebral Oedema.
Excess accumulation of fluid in the brain parenchyma
- Shows on CT as a loss of gyri

What are the types of cerebral oedema?
- Vasogenic – disruption of the blood brain barrier
-
Cytotoxic – secondary to cellular injury e.g. hypoxia/ischaemia
- Usually due to damage at the astrocyte end-foot processes
- AQA4 is found in the brain (and is used to transport water)
What is the normal flow of CSF in the brain?
- CSF produced in choroid plexus (mainly in the lateral ventricles)
- Flows from the lateral ventricle → intraventricular foramina → 3rd ventricle
- Down the cerebral aqueduct → 4th ventricle (floor is the pons and the roof is the cerebellum)
- Into the medulla → central canal of the spinal cord (relatively little CSF goes down the spinal cord because most of it exits via a number of foramina in the 4th ventricle into the subarachnoid space)
- Circulate through the subarachnoid space and via the arachnoid granulations (superior sagittal sinus) → systemic circulation
What are the two forms of hydrocephalus?
- Non-Communicating = obstruction to the flow of CSF (usually involving the cerebral aqueduct)
-
Communicating = associated with problems in reabsorption of CSF into venous sinuses
- Can be caused by infection (e.g. meningitis)
- Inflammation of the meninges impinge and interfere with the normal flow of CSF to be reabsorbed
- Can be caused by infection (e.g. meningitis)
What is the normal ICP in a supine adults
7-15 mmHg
What is the major complication associated with raised ICP?
Herniation of brain structures
- Subfalcine → cortex forced under rigid falx cerebri
- Uncal → medial temporal lobe through tentorial notch
- Tonsillar → tonsil of cerebellum pushed through foramen magnum

Define Stroke.
Clinical syndrome characterised by rapidly developing clinical symptoms and/or signs of focal, and at times global loss of cerebral function, with symptoms lasting more than 24 hours or leading to death due to vascular pathology.
- Infarct → cerebral infarction
- Haemorrhage → SUB-ARACHNOID, primary intracerebral or intraventricular
- Excludes
- Subdural haemorrhage
- Epidural haemorrhage
- Infarction / Haemorrhage caused by infection or tumour etc
What is a TIA?
- Temporary brain clot that lasts <24hrs
- 1/3rd people with TIA get a significant infarct within 5 years → predictor of a future infarct
- Most TIAs last < 5 mins
- There is usually NO permanent injury to the brain
What is non-traumatic intra-parenchymal haemorrhage and how does it present?
Haemorrhage into the substance of the brain (parenchyma) due to rupture of a small intraparenchymal vessel
- Most common in the basal ganglia
- Hypertension plays a role in >50% of bleeds
- Presentation:
- Severe headache
- Vomiting
- Rapid loss of consciousness
- Focal neurological signs
How can arteriovenous malformations lead to strokes?
- Can occur anywhere in the CNS
- Symptomatic from 2nd and 5th decade → mean = 31 years
- High pressure = massive bleed
- Morbidity 50-80%
- Mortality at 15%
- Can be visualised on angiography

What is the presentation of arteriovenous malformations strokes and how can they be managed?
- Presentation:
- Haemorrhage
- Seizures
- Headache
- Focal neurological deficits
- Treatment:
- Surgery
- Embolisation
- Radiosurgery
What are cavernous angioma how can they cause strokes?
- Well-defined malformative lesion composed of closely-packed vessels with no parenchyma interposed between vascular spaces
- Similar to an AVM but no brain substance wrapped up amongst the vessels
- Can be found anywhere in the CNS
- Usually symptomatic over the age of 50 years
- Pathogenesis is unknown
- Strokes / bleeds can occur under lower pressure
What is the presentation of cavernous angioma strokes, what investigations should be carried out and how can they be managed?
- Presentation
- Headache
- Seizures
- Focal deficits
- Haemorrhage
- Investigation = MRI
- Target Sign – black ring around lesion (AVM has no ring) – no brain parenchyma
- Treatment:
- May not be necessary
- Surgery
What is the most common cause of sub-arachnoid haemorrhage?
Rupture of a berry aneurysm
- 1% of the general population; congenital
- Highest risk of rupture when 6-10mm
- 80% occur at the internal carotid bifurcation
- 20% occur within the vertebrobasilar circulation
- 30% of patients will have multiple berry aneurysms

What is the presentation of sub-arachnoid haemorrhage strokes and how can they be managed?
- Presentation
- Sudden-onset severe headache (Thunderclap)
- Vomiting
- Loss of consciousness
- Treatment
- Endovascular coiling
What are the differential diagnoses of infarct stroke?
- Tissue necrosis (stains)
- Rarely haemorrhagic
- Permanent damage in the affected area
- No recovery
What are the differential diagnoses of haemorrhagic stroke?
- Bleeding
- Dissection of parenchyma
- Fewer macrophages
- Limited tissue damage (periphery)
- Partial recovery
What is the largest cause of trauma death in people <45 years old?
TBI
- Accounts for 25% of all trauma deaths
- High morbidity
- 19% in a vegetative or severely disabled state
- 31% good recovery
What are the consequences of trauma related skull fractures?
-
Otorrhoea and Rhinorrhoea → i.e. loss of CSF through the ear or nose)
- Increases risk of infection - ruptured the containment of the CSF → acts as a route of infection into the cranial cavity
What are two signs associated with skull fractures?
- Battle sign → basilar skull fracture
- Bruise over mastoid process
- Takes 1 day to appear
- Racoon eyes → basal skull fracture
- Takes 1 day to appear

Define Brain Contusion.
Brain collides with the internal surface of the skull.
Define Brain Laceration.
Brain colliding with the internal surface of the skull leading to rupture of the pia mater.
Where do brain contusions and lacerations often occur?
- Due to direct contact with the skull
- Lateral surfaces of the hemispheres
- Inferior surfaces of frontal and temporal lobes
- Rebound of the brain after a direct impact can cause contrecoup damage to the opposite side of the brain
Describe Diffuse Axonal Injury.
Shearing and tensile forces cause damage to the axons.
- Occurs at the moment of injury
- Most common cause of non-haemorrhagic coma
- In some people who survive head injuries, they suffer cognitive and degenerative problems further down the line
- Potentially due to persistent inflammation
- In some people who survive head injuries, they suffer cognitive and degenerative problems further down the line
- Midline structures are particularly affected
- Corpus callosum
- Rostral brainstem
- Septum pellucidum
What is a Prion Disease?
Series of diseases with common molecular pathology.
- There is a transmissible factor
- There is no DNA or RNA involved
- Prion protein is transmitted and changes the host protein into the pathological form → can’t be metabolised and accumulates
Name some prion diseases that affect humans?
- Creutzfeldt-Jakob disease (CJD)
- Gerstmann-Straussler-Sheinker syndrome
- Kuru – endemic to Papua New Guinea
- Fatal familial insomnia
What is the histology of prion disease?

What is the pathophysiology of prion disease?
- The normal PrPSc protein can unfold and refold into a beta-pleated sheet form which is much more susceptible to aggregation
- Once a little bit of this forms, it can propagate
- This leads to a lot of insoluble protein accumulating in the parenchyma of the brain

What is new variant CJD (vCJD)?
A prion disease which is linked to BSE (Mad cow disease) that has been diagnosed at autopsy since 1990
- Patients were <45 years old
- Clinical features:
- Cerebellar ataxia
- Dementia
- Longer duration than CJD
What is the pathology of Alzheimer’s disease?
- Extracellular / Amyloid-beta plaques - right image
- Neurofibrillary tangles (Tau)
- Disrupts cytoskeleton of neurones
- Cerebral amyloid angiopathy - left image
- Deposits of proteins in the blood vessel walls → impairs vascular function
- Neuronal loss / Cerebral atrophy
- Shrinkage of brain
- Hippocampus → loss of short-term memory

Describe Amyloid Precursor Protein.
Normal physiological function of AB protein is still unknown
- Ab is formed by cleavage of APP at a transmembrane site
- APP can be processed in TWO ways
- Amyloidogenic
- Amino terminus of Ab cleaved → amyloidogenic → too much Ab → Ab thrown out of cell → accumulates → Ab forms monomers → dimers → protofibrils → fibrils (polymers)
- Non-amyloidogenic
- Ab sequence directly cleaved in two
- Amyloidogenic
- Toxicity of Ab is more likely to be intracellular
- Extra-cellular plaques probably don’t cause direct problems
What is the normal physiology vs pathophysiology of amyloid in Alzheimer’s?
Normal
- APP cleaved by a-secretase
- sAPPa released and the C83 fragment remains
- C83 is then digested by g-secretase
- Products are then removed
Pathophysiology
- APP cleaved by b-secretase
- sAPPb released and the C99 fragment remains
- C99 is digested by g-secretase releasing b-amyloid (Ab) protein
- Ab protein forms the toxic aggregates
What is the normal physiology vs pathophysiology of Tau in Alzheimer’s?
Normal
- Tau protein is a soluble protein present in axons
- Tau important for assembly and stability of microtubules
Pathophysiology
- Hyperphosphorylated tau is insoluble → self-aggregates
- Self-aggregates form neurofibrillary tangles (neurotoxic)
- The tangles result ultimately in microtubule instability and neurotoxic damage to neurones
What is the normal physiology vs pathophysiology of inflammation in Alzheimer’s?
Normal
- Microglial cells are specialist CNS macrophages
Pathophysiology
- Increased inflammatory mediators and cytotoxic proteins
- Increased phagocytosis
- Decreased levels of neuroprotective proteins
Describe the Tau protein.
- Microtubule-associated protein - used for maintaining stability of the cytoskeleton
- When it becomes hyperphosphorylated it starts causing problems
- Accumulates inside the cell and eventually it will cause cell death
- Presence and spread of tau throughout the brain is quite stereotypical and matches up quite closely with the clinical symptoms seen in the patient → Braak staging
How is Tau progression staged?
Braak staging → symptoms appear at stage 3 or 4:
- Stage I = trans-entorhinal region
- Stage II = entorhinal region (interfaces neocortex and hippocampus)
- Stage III = temporo-occipital gyrus (see the immunostaining by eye)
- Stage IV = temporal cortex
- Stage V = peri-striatal cortex (cortex around the primary visual cortex)
- Stage VI = striatal cortex (occipital lobe)
What is CTE?
Chronic Traumatic Encephalopathy = A tauopathy in people with a history of multiple repetitive TBI
- This has been seen in boxers, American footballers, rugby players and footballers
What is Parkinson’s Disease?
Parkinson’s disease = death of dopaminergic cells of substantia nigra (projects to basal ganglia) → basal ganglia are very important in the initiation of movement
- Characterised by the presence of Lewy bodies = cells with a-synuclein
- Dopaminergic cells produce neuromelanin → colours the substantia nigra → decoloration of substantia nigra
What are the signs and symptoms of Parkinson’s disease?
- Bradykinesia
- Rigidity
- Pill-rolling tremor
What is the histology of Parkinson’s disease?
- Lewy bodies are intracellular accumulations of a-synuclein
- Proteinopathy developed from abhorrent metabolism of a-synuclein → mutations in a-synuclein gene à PD
- a-synuclein immunostaining = diagnostic gold standard

What is the staging of Parkinson’s disease?
Braak PD stages:
- Based on the distribution of a-synuclein pathology throughout the brain
- Bottom-up spread - originates in the brainstem
- Goes from the medulla, up the pons and the midbrain
- Moves into the basal forebrain and the cortices

How many nigral neurones need to be lost before Parkinson’s becomes symptomatic?
60-70%
What are the access points for environmental agents affect Parkinson’s?
- Retrograde from gut to medulla via vagus nerve
- Through the nose
In what conditions can Parkinsonism be found?
- Idiopathic Parkinson’s disease
- Drug-induced Parkinsonism
- Multiple system atrophy - a-synuclein in glial cells
- Progressive supranuclear palsy - tau pathology
- Corticobasal degeneration - tau pathology
- Vascular pseudoparkinsonism
- Alzheimer’s changes
- Fronto-temporal neurodegenerative disorders
What is Multiple System Atrophy (MSA)?
-
a-synucleinopathy → however targets glial cells apposed to dopaminergic cells
- Tends to affect the cerebellum
- Patients are more likely to present with falls
- Tends to affect the cerebellum
Name some Tau Immunostaining Disease.
- Progressive Supranuclear Palsy
- Corticobasal Degeneration
- Frontotemporal dementia (Pick’s disease)
What are the histological features of Pick’s disease (Frontotemporal dementia Tau +ve)?
- Fronto-temporal atrophy
- Marked gliosis and neuronal loss
- Balloon neurons
- Tau-positive Pick bodies
Describe the structure of Tau?
- Single gene on 17q21 with 16 exons
- Alternative splicing leads to 6 isoforms
- There are either 3R or 4R forms of tau that exist in the brain - two further subsets with unknown functions
- The longest form is 4R/2N
- The smallest form is 3R/0N

Describe Tau-ve Fronto-temporal Lobar Dementia.
FTLD-U (ubiquitinated)
- Fronto-temporal dementia associated with progranulin mutations → tendency for the atrophy to be unilateral
- Problems with TDP-43 (trafficking protein) thought to be the basis for some types of FTLD (associated with MND)
- TDP-43 = TAR DNA Binding Protein 43
- Other associations:
- FUS pathology
- C9ORF72 mutations
What is the radiological classification of CNS/brain tumours?
-
Extra-axial
- Tumours of bone, cranial soft tissue, meninges, nerves and metastatic deposits
-
Intra-axial
- Derived from normal cell populations of the CNS (glia, neurons, vessels, connective tissue)
- Derived from other cell types (metastases, lymphomas, germ cell tumours)
What is the histological classification of CNS/brain tumours?
- Extra-axial
- Meningothelial cells – meningioma
- Schwann cells – schwannoma
- Intra-axial
- Astrocytes – astrocytoma
- Oligodendrocytes – oligodendroglioma
- Ependyma – ependymoma
- Neurons – neurocytoma
- Embryonal cells – medulloblastoma
What is the aetiology of CNS tumours?
- Largely unknown
- Radiation to head and neck: meningiomas, rarely gliomas
- Neurocarcinogens
- Genetic predisposition (<5% of primary brain tumours)
- Neurofibromatosis is most common form
- Autosomal dominant inheritance
- Neurofibromatosis is most common form
What are the signs and symptoms of brain tumours?
- Increased ICP
- Headache
- Vomiting
- Changed mental state
- Supratentorial
- Focal neurological deficits
- Seizures
- Personality change
- Subtentorial
- Cerebellar ataxia
- Long tract signs
- Cranial nerve palsies
What is the management of brain tumours?
-
Surgery → maximal safe resection aims to obtain and extensive excision with minimal damage to the patient
- Craniotomy → debulking (subtotal and complete resections)
- Open biopsies → inoperable but approachable tumours
- Stereotactic biopsy → open biopsy not indicated
-
Radiotherapy
- Low and high-grade gliomas
- Metastases
-
Chemotherapy - biological agents → EGFR inhibitors, PD-1 inhibitors etc
- High-grade gliomas (temozolomide)
How does grading of brain tumours stratefy them?
Outcomes
- Some tumours only have a few possible types and not all 4 → i.e. only 1 possible grade
- Grading does not tell us therapy response, disease spread or cell of origin (type)
- Grade I = benign, long-term survival
- Grade II = cause death in >5 years
- Grade III = cause death <5 years
- Grade IV = cause death <1-year
Name some Glial tumours.
- Circumscribed
- Pilocytic astrocytoma (grade I) - most common
- Pleomorphic xanthoastrocytoma (grade II)
- Subependymal giant cell astrocytoma (grade I)
- Diffuse
- Diffuse astrocytoma (grades II-IV)
- Oligodendroglioma (grades II-III)
What are the features of circumscribed gliomas?
- Grades I-II
- Occurs in children
- Rare malignant transformation
- BRAF mutation present in 50% of cases (MAPK pathway mutation)
Describe pilocytic astrocytomas?
- Grade I
- Most common child brain tumour → 20% CNS tumours <14yo
- Common in neurofibromatosis I (NF1)
- MRI → cerebellar; well circumscribed, cystic, enhancing
- Histopathology
- Piloid (hairy) cell
- Rosenthal fibres and granular bodies
- Slow growing with low mitotic activity
- BRAF mutation present in 70% of cases

What are the features of diffuse gliomas?
- Grades ≥II
- Occurs in adults
- Malignant progression
- IDH1/2 mutation present in 30% of cases - also a +ve prognostic factor
Describe diffuse astrocytomas.
- Grade II-IV
- Patients 20-40yo
- Locations
- Adults = Cerebral hemispheres
- Children = Cerebellum
- Progresses to a glioblastoma (Grade IV) → takes several years
- MRI → T1 hypointense, T2 hyperintense, non-enhancing lesion
- Low choline: creatinine ratio at MR-spectroscopy
- Cytology
- Low to moderate cellularity
- Mitotic activity negligible/absent
- Vascular proliferation and necrosis absent
- Low to moderate cellularity
- IDH1/2 mutation present in >80% of cases

Describe glioblastoma multiforme’s.
- Grade IV
- Most common primary brain cancer
- Most patients >50yo
- MRI → heterogenous, enhancing post-contrast
- Cytology
- High cellularity
- High mitotic activity
- Neoangiogenesis
- Necrosis
- Histological criteria
- Pathological blood vessels
- Blood vessel structural abnormalities
- Cellularity on inspection
- Genetics:
- 90% of cases = wildtype IDH
- 10% of cases = astrocytoma progression (have the IDH mutation)
- IDH mutant = +ve prognostic factor
Describe oligodendrogliomas.
- Grade II-III
- 5% of all primary brain tumours
- Patients 20-40yo with a long history of neurological signs
- MRI → no/patchy contrast enhancement
- Cytology
- Round cells with clear cytoplasm = “fried eggs”
- IDH1/2 mutation and co-deletion of 1p/19q present in ~100% of cases = diagnostic

Describe meningiomas.
- Rare in patients <40yo
- Any site of craniospinal axis - can have multiple sites (i.e. NF2)
- MRI → extra-axial, isodense, contrast-enhancing
- Histology
- Attaches to meninges but does not typically invade, just displaces brain matter
- If they invade = often a micro-invasion (picture)
- Globules found on histopathology
- Attaches to meninges but does not typically invade, just displaces brain matter

What is the grading of meningiomas?
-
Grade I (80%) = Benign
- Recurrence <25%
- <4 mitotic activity per 10 HPF
-
Grade II (19%) = Atypical
- Recurrence 25-50%
- 4-20 mitotic activity per 10 HPF
-
Grade III (1%) = Malignant
- Recurrence 50-90%
- >20 mitotic activity per 10 HPF
What is the most common CNS tumour in adults?
CNS Metastasis - 10x more than intrinsic tumours
- Increasing incidence due to longer survival
- Often multiple
- Very poor prognosis
What are the most frequent sites of origin of CNS metastasis?
- Any tumour can potentially give CNS metastases → can be the first presentation of the disease
- Origin can be challenging to determine
-
Most frequent tumours
- Lung
- Breast
- Melanoma
Where are CNS metastases usually found?
Grey-white junction
- As structure of cerebral blood vessels changes at this point → become smaller as they enter the white matter → neoplastic emboli tend to get stuck at this level and then start growing
Describe medulloblastoma.
- Grade IV
- Embryonal tumour = originates from neuroepithelial precursors of the cerebellum/dorsal brainstem
- Located in the Cerebellum
- Rare → but 2nd most common brain tumour in children
- Histology:
- “Small blue round cell” tumour = Wilm’s tumour
- Expression of neuronal markers – i.e. synaptophysin
- Homer-Wright rosettes

- A 45-year-old female
- History: pulmonary lobectomy
- 2 days of headache and vomiting
- Worsening headache
- CT: right frontoparietal SOL with minimal midline shift to the left
What is the diagnosis?
Metastatic carcinoma
- A 5-year-old boy
- Had headache and vomiting in the morning for 2 weeks
- Symptoms worsened and the vision became blurred
- Fundoscopic exam: papilledema
- MRI showing cystic cerebellar lesion → tumour was removed
Pilocystic astrocytoma
- A 70-year-old male
- Seizure following 2 weeks of left arm and leg weakness
- MRI showing heterogeneous enhancing right frontal lesion, started on steroids
- Partial response to steroids with improved dexterity of the left arm and leg
- A tumour was partially resected
Glioblastoma
What is the epidemiology of atheroma?
- In the western world = ½ of all deaths and more morbidity and mortality than any other disorder
- USA mortality rate from IHD is 5x than in Japan
- IHD is increasing in Japan (increasing western diet): now second leading cause of death there
Define atherosclerosis.
Characterised by atheromatous deposits in and fibrosis of the inner layer of the arterioles.
What are the risk factors for atheromatous plaques?
- Non-modifiable:
- Age
- Sex (premenopausal women protected à post-menopausal women = >risk than men)
- Genetics (FHx, familial hypercholesterolaemia, polymorphisms)
- Modifiable:
- Hyperlipidaemia (LDL bad / HDL good, diet, statins inhibit HMG-CoA reductase)
- Hypertension (increased IHD risk by 60%)
- Smoking
- Diabetes mellitus (induces hypercholesterolaemia and atherosclerosis)
- Other risk factors: inflammation, hyperhomocyteinaemia, metabolic syndrome, lipoprotein a, haemostasis (pro-coagulation), lack of exercise, stress, obesity
- Risk factors have a multiplicative effect – 2 risk factors increase the risk 4x (3 RFs = 7x increase risk)
- 20% of CVD events occur in absence of RFs and 75% events in healthy women occur in LDL below the risk level
What is the pathogenesis of atherosclorsis?
- Endothelial injury à LDL accumulation
- Monocyte adhesion to endothelium
- Monocyte migration into intima → macrophages & foam cells
- Platelet adhesion → factor release → smooth muscle cell recruitment
- Lipid accumulation à extracellular and intracellular macrophages and smooth muscle cells
What is a Fatty lesion?
- Earliest lesion - tiny streaks in the vessel wall
- Lipid filled foamy macrophages
- No flow disturbance
- In virtually all children <10y/o
- Relationship to plaques is uncertain but often found in the same sites as plaques
What is a Atherosclerotic plaque?
- Later stages
- Patchy with local flow disturbance → only involve portion of the wall - rarely circumferential
- Appear eccentric and composed of cells, lipid and matrix
- Can rupture or obstruct
- Occur in points of disturbed flow
- Bifurcations
- Curvatures
What are the pathological consequences of atherosclerotic plaques?
-
Stenosis
- Critical stenosis is when demand > supply → occurs at 70% occlusion = “stable” angina
- Acute plaque rupture can occur
-
Acute plaque change
- Rupture: exposes prothrombogenic plaque contents
- Erosion: exposes prothrombogenic subendothelial basement membrane
- Haemorrhage into plaque (increases size)
- Majority of plaques which show acute change only show mild to moderate luminal stenosis prior to acute change: therefore, there are numerous asymptomatic potential victims
What are the features of a vulnerable atherosclerotic plaque?
- Lots of foam cells and extracellular lipid
- Thin fibrous cap
- Few smooth-muscle cells
- Clusters of inflammatory cells
At what percentage of stenosis (due to atheroma) does angina occur?
Stable = 70%
Unstable = 90%
Where in the heart are most atherosclerotic plaques found?
- First parts of LAD or LCx
- Entire length of RCA
Describe angina pectoris.
Transient ischaemia not producing myocyte necrosis
- Stable = comes on with exertion, relieved by rest, no plaque disruption
- Prinzmetal (uncommon) = artery spasm
- Unstable = more frequent, longer, onset with less exertion or at rest
- Disruption of plaque
- Superimposed thrombus
- Possible embolisation or vasospasm
- Warning of impending infarction
What is the pathogenesis of a MI?
- Artery occlusion due to:
- Sudden change of plaque / Thrombus evolution
- Coagulation / Platelet aggregation
- Vasospasm
- Myocardial response
- Loss of contractility within 60 seconds → potentially reversible but irreversible after 20-30 minutes
- LAD: 50%, anterior wall left ventricle, anterior septum, apex
- RCA: 40%, posterior wall left ventricle, posterior septum, posterior right ventricle
- LCx: 20%, lateral left ventricle, not apex
How does the cardiac histology change over the months following a MI?
- <6 hours = normal by histology (CK-MB also normal)
- 6–24 hours = coagulative necrosis, loss of nuclei and striations
- 1-4 days = infiltration of neutrophils
- 5-10 days = removal of debris by macrophages
- 10-14 days = granulation, angiogenesis, collagen synthesis
- Weeks to months = strengthening, decellularising scar

What is the potential consequence of angioplasty for an acute MI?
Reperfusion injury
- Due to oxidative stress, Ca2+ overload and inflammation
- Arrhythmias common
- Biochemical abnormalities last days to weeks
- Thought to cause “stunned myocardium” → reversible cardiac failure lasting several days
What is hibernating myocardium?
- Chronic sublethal ischaemia causing lowered metabolism in myocytes is reversed with revascularisation
What are the complications of MI?
- Death (30% in 1 year but 3-4% after due to complications)
- Arrhythmia
- Rupture (papillary muscle)
- Tamponade
- Heart failure
- Valvular disease
- Aneurysm of ventricle
- Dressler’s syndrome (pericarditis; 2nd or 3rd day)
- Embolism (i.e. bowel ischaemia)
- Recurrence
Describe Chronic IHD.
- Progressive heart failure due to ischaemic myocardial damage - may not be prior infarction
- Can arise with:
- Severe obstructive coronary artery disease
- Enlarged heavy heart
- Hypertrophied and dilated LV
- Atherosclerosis
- Fibrosis (microscopic)
Describe Sudden Cardiac Death/Failure.
Unexpected death from cardiac causes in individuals without symptomatic heart disease or within 1 hour after onset of symptom → usually due to lethal arrhythmia triggered by ischaemia-induced electrical instability
- Usually on background of IHD (90%)
- Drugs such a cocaine may be the cause
- Acute myocardial ischaemia is usual trigger of arrhythmia
- Can be heritable
- Marked atherosclerosis (>75% stenosis) in one or more vessels usually >90%
- 10% non-atherosclerotic cause (long QT)
- Half have plaque rupture
- 25% have MI changes but conflicting data on role of MI
Describe Cardiac failure.
- Types:
- Left = SOB, pulmonary oedema (CXR = ABCDE)
- Right = peripheral oedema (nutmeg liver)
- Congestive heart failure
- Causes:
- IHD
- Valve disease
- Hypertension
- Myocarditis
- Cardiomyopathy
- Left sided heart failure → right sided failure
- Pathology
- Dilated heart
- Scarring
- Thinning of the walls
- Microscopy = fibrosis and replacement of the ventricular myocardium
- Complications
- Sudden death
- Arrhythmias
- Systemic emboli
- Pulmonary oedema with superimposed infection
Describe Dilated cardiomyopathy.
- Progressive loss of myocytes → dilated heart
- Causes:
- Idiopathic
- Infective: viral myocarditis
- Toxic: alcohol, chemotherapy (adriamycin, daunorubicin)
- Cobalt, iron
- Hormonal: hyper/hypothyroid, diabetes, peri-partum
- Genetic: haemochromatosis, Fabry’s, McArdle’s
- Immunological: myocarditis; inc. viral
Describe Hypertrophic cardiomyopathy (HOCM).
- Left ventricular hypertrophy → narrows outflow
- Familial in 50% (autosomal dominant, variable penetrance)
- Beta-myosin heavy chain
Describe Restrictive cardiomyopathy.
- Impaired ventricular compliance
- Idiopathic or secondary to myocardial disease (amyloid, sarcoidosis)
- Normal heart size but big atria
Describe Chronic rheumatic valvular disease.
- Sequelae of earlier rheumatic fever
- Predominantly left-sided → almost always mitral stenosis
- Mitral > Aortic > Tricuspid > Pulmonic
- Mitral alone 48%; mitral and aortic 42%
- Thickening of valve leaflet → especially along lines of closure
- Fusion of commissures
- Thickening, shortening and fusion of chordae tendineae
Describe Calcific aortic stensosis.
- Commonest cause of aortic stenosis (esp. in elderly; 70-80s)
- Calcium deposits in outflow side cusp which impair opening or orifice is compromised
- Outflow tract obstruction
What are the cause aortic regurgitation?
- Rigidity: RHD
-
Destruction: infective endocarditis
- Left-sided normally - often the more ‘damaged valve’
- Right-sided in IVDU - first valve bacterium come across
-
Disease of aortic valve ring: dilatation means that valve is insufficient to cover increased area
- Marfan’s Syndrome
- Dissecting aneurysm
- Syphilitic aortitis
- Ankylosing spondylitis
Describe aneurysms.
- True = all layers of the wall
- False = extravascular haematoma → Aortic dissections
- Causes = weak wall of large arteries
- Marfan’s
- Atherosclerosis
- Hypertension
What are the congenital gynaecological abnormalities?
- Duplication (i.e. uterus didelphys)
- Agenesis – missing part of the genital tract (e.g. a fallopian tube)
What are the infections of the gynaecology?
- Infections that cause discomfort with NO serious complications
- Candida: more common in diabetes, OCP, pregnancy
- Trichomonas vaginalis: protozoan
- Gardenerella: Gram-negative bacillus causes vaginitis
- Infections that cause SERIOUS complications
- Chlamydia: major cause of infertility
- Gonorrhoea: major cause of infertility
- Mycoplasma: causes spontaneous abortion and chorioamnionitis
- HPV: implicated in cancer
What are the causes of PID?
-
Chlamydia > gonococci, enteric bacteria
- Usually starts at the lower genital tract and spreads upwards via the mucosal surface
-
Other causes = staph/strep, coliform, clostridium perfringens
- These tend to occur secondary to abortion
- Usually starts in the uterus and spreads upwards via lymphatics and blood vessels
- Involves the deep tissue layers
What are the complications of PID?
- Peritonitis
- Intestinal obstructions due to adhesions
- Bacteraemia
- Infertility
What are the complications of salphingitis?
- Plical fusion
- Adhesions to ovary
- Tubo-ovarian abscess
- Peritonitis
- Hydrosalpinx (fallopian filled with fluid)
- Infertility
- Ectopic pregnancy
What is the epidemiology of cervical cancer?
- 2nd most common cancer affecting women worldwide
- Mean age: 45-50 years
What are the risk factors for cervical cancer?
- HPV (95%)
- Many sexual partners
- Sexually active early
- Smoking
- Immunosuppression (i.e. HIV)
What are the high / low - risk HPV types?
- High-risk = CIN / Cancer
- 16 and 18
- Others = 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68, 82)
- Low-risk = genital / oral warts
- 6 and 11
- Other types: 40, 42, 43, 44, 54, 61, 72, 73, 81)
What is the pathogenesis of HPV in relation to cervical cancer?
- Most people = Nothing = Immune system eliminates HPV → undetectable within 2 years in 90% of cases
- HPV 16 / 18 = encode proteins E6 and E7 which bind to and inactivate TSGs
- E6 → p53
- E7 → retinoblastoma
- Interferes with apoptosis and increased cellular proliferation which contributes to oncogenesis
What are the phases of HPV life cycle?
- Infection is either latent or productive:
- Latent = HPV resides in cell and only replicates when the cell divides
- Complete viral particles not produced
- Cellular changes of HPV not seen
- Productive = HPV replicates independently of cell cycle
- Cellular changes of HPV are seen
- Halo around the nucleus (koilocyte)
- Latent = HPV resides in cell and only replicates when the cell divides
What are the classifications of CIN through to carcinoma?

How does the disease pattern change between SCC and adenocarcinoma of the cervix?
- CIN (endocervical) = dysplastic changes → invasive SCC
- 80% - most common
- CGIN (glandular) = dysplastic changes → invasive adenocarcinoma
- 20%
What are the routine screening interval in the nation cervical screening?
- First invitation: 25 years
- 25-49 = 3-yearly
- 50-62 = 5-yearly
- 65+ = only screen those not screened since they were 50 or have recent abnormal tests
Describe the HPV vaccine?
- 2 vaccines available
- Bivalent (16 + 18)
- Quadrivalent (6, 11, 16, 18)
- National vaccination programme for girls aged 12 and boys aged 13 (second dose 6-24 months later)
- Does not protect you from all high-risk types
What are the diseases if the uterine corpus?
- Congenital anomalies
- Inflammation: acute or chronic
- Adenomyosis
- Dysfunctional uterine bleeding: e.g. hormonal imbalance
- Endometrial atrophy and hyperplasia
- Endometrial polyp
- Uterine tumours
- Endometrial epithelial tumours and precursors
- Tumour like lesions; e.g. endometrial polyp
- Mesenchymal tumours specific to the uterus
- Mixed epithelial and mesenchymal tumours
- Miscellaneous tumours
Describe Fibroids.
- Smooth muscle tumour of the myometrium
- Most common uterine tumour - found in 20% of >35yo
- Usually multiple
- May be
- Intramural
- Submucosal
- Subserosal
What are the malignant counterpart to fibroids?
Leiomyosarcoma
- Rare
- Usually solitary
- Post-menopausal women
- Local invasion and spread via the blood stream
- 5-year survival of 20-30%
Describe endometrial hyperplasia.
Increase in stroma and glands (usually driven by oestrogen)
- Causes = OESTROGEN
- Peri-menopausal
- Persistent anovulation (because of persistently raised oestrogen levels)
- PCOS can also cause persistently elevated levels of oestrogen giving rise to endometrial hyperplasia
- Granuloma cell tumours of the ovary
- Oestrogen therapy
- Can be associated with atypia / pre-cancerous changes
What are the risk factors for endometrial carcinoma?
- Oestrogen
- Nulliparity
- COCP
- Early menarche
- Tamoxifen
- HRT
- Late menopause
- Obesity
- DM
Describe Type 1 endometrial carcinoma.
- 85% of endometrial cancer
- Subtypes:
- Endometrioid
- Mucinous
- Secretory adenocarcinoma
- Younger patients
- Oestrogen-dependent
- Associated with atypical Endometrial hyperplasia
- Often present as low-grade tumours → superficially invasive
-
Genetic Mutations – need accumulation ≥4 different mutations
- PTEN
- PI3KCA
- K-Ras
- CTNNB1
- FGFR2
- p53
Describe Type 2 endometrial carcinoma.
- 15% of endometrial cancer
- Subtypes
- Serous
- Clear cell tumours
- Older patients
- Less oestrogen-dependent
- Arise in atrophic endometrium
- Present later → high grade, deeper invasion and higher stage
-
Genetic Mutations
-
Serous Carcinoma
- p53 (90%)
- PI3KCA (15%)
- Her 2 amplification
-
Clear Cell Carcinoma
- PTEN
- CTNNB1
- Her-2 amplification
-
Serous Carcinoma
Describe the FIGO staging of endometrial carcinoma.
- I = limited to uterus
- II = spread to cervix
- III = spread adjacent
- IV = distant spread
What are the types of gestational trophoblastic disease?
- Complete
- Partial mole
- Invasive mole
- Choriocarcinoma
Describe complete and partial moles.
- Presentation:
- Spontaneous miscarriage
- USS – snowstorm, cluster of grapes
- Very high hCG
- Complete moles may persist or recur
- Prevalence = 1 in 1000 pregnancies
- Complete = empty egg fertilised by 2 sperm (or 1 which duplicates DNA) → 46 XY or 46 XX (paternal origin only)
- Partial = normal egg fertilised by 2 sperm (or 1 which duplicates DNA) → 69 XXX or 69 XXY (1x maternal and 2x paternal origin)

Describe choriocarcinoma?
-
Incidence: 1 in 20,000-30,000 pregnancies
- Rapidly invasive, widely metastasising (lung, vagina, brain, liver, kidney)
- Responds well to chemotherapy
- 50% arise in moles
- 25% arise in previous abortion
- 22% arise in normal pregnancy
Describe endometriosis.
Presence of endometrial tissue outside the uterus - metaplasia of pelvic peritoneum → implantation of endometrial tissue
- Ectopic endometrial tissue is functional and bleeds at the time of menstruation → pain, scarring and infertility
- Associations:
- Strongly → clear cell (mesonephroid/epithelial) ovarian cancer
- Less strongly → endometroid (epithelial) ovarian cancer
- 10% of premenopausal women
What are the types of ovarian cysts?
- Non-neoplastic functional Cysts
- Follicular and luteal cysts
- Endometriotic cyst
- Polycystic Ovarian Syndrome (PCOS)
- 3-6% of women of reproductive age
- Patients have persistent anovulation
- Other features include obesity and hirsutism/virilism
What are the risk factors for ovarian tumours?
- Oestrogen - not COCP
- Nulliparity
- Early menarche
- Late menopause
- HRT
- Genetic predisposition (1%) = Lynch II
- FHx of ovarian or breast cancer
- Endometriosis
- Inflammation (PID)
What are the protective factors for ovarian tumours
- Pregnancy
- COCP
Briefly describe the distribution in the types of ovarian tumours?
Epithelial
- Type 1
- Low-grade serous
- Mucinous
- Endometroid
- Clear cell
- Transitional
- Mixed types
- Type 2
- High-grade serous
- 65% of all ovarian tumours
- 95% of all malignant tumours
Germ cell tumours
- Bimodal peaks - 15-21 and 65-69
Sex cord tumours
- Most common in post-menopausal women - some subtypes in 25-30-year olds
What are the causes of heredity ovarian cancer?
- Familial breast-ovarian cancer syndrome = BRCA1 association
- Site-specific ovarian cancer = BRCA1 association
- Lynch type II
Describe the classification of epithelial tumours.
- Type 1 ovarian carcinoma = low-grade
- Low-grade serous
- Endometroid
- Mucinous
- Clear cell
- Arise from benign ovarian tumours and endometriosis
- Present as large, stage 1 tumours
- Mutations = K-Ras, BRAF, PI3KCA, Her2, PTEN, beta-catenin
- Type 2 ovarian carcinoma = high grade and aggressive
- High-grade serous carcinomas
- NO precursor lesions
- Mutations = p53 (75% of cases), K-Ras, BRAF, BRCA
- BRCA = better response to chemo plus can use PARP inhibitors
Describe secondary ovarian tumours?
- Krukenberg Tumour = bilateral metastases composed of mucin-producing signet ring cells
- Most often from gastric or breast cancer
- Metastatic Colorectal Carcinoma
- Ovaries are prone to metastatic spread of colorectal cancer
Describe endometroid ovarian tumours.
- Epithelial - 10-24% of ovarian tumours
- Associated with
- Endometriosis (10-20% associated with endometriosis)
- Endometrioid carcinoma co-existence in uterus
- Better prognosis than mucinous and serous
Describe serous ovarian tumours?
- Epithelial – most common (usually cystic, 30-50% are bilateral)
- Benign tumours – lined by bland epithelium
- Borderline tumours – more complex, atypical epithelial lining with papillae (NO invasion through basement membrane)
- Malignant tumours – invasive with poor prognosis (15% 5-year survival)
Describe Mucinous tumours.
- Epithelial – 10-20% of ovarian tumours
- Secrete mucin (epithelium resemble gastrointestinal or endocervical epithelium)
- 4-10% of colorectal cancer metastases to ovary – 14-32% identified in ovary first
Describe clear cell ovarian carcinoma.
- Epithelial
- Strong association with endometriosis
- Called ‘clear cell’ because their cytoplasm is clear due to the presence of a lot of glycogen
- Glycogen dissolves when the sample is processed for microscopy leaving an empty space)
Describe sex cord stromal tumours?
-
Fibromas (arising from fibroblasts):
- Benign
- No endocrine production
-
Granulosa cell (arising from granulosa cells):
- Variable behaviour
- May produce oestrogen
-
Thecoma (arising from thecal cells):
- Benign
- May secrete oestrogen (rarely secretes androgens)
-
Sertoli-Leydig Cell (arising from Sertoli-Leydig cells)
- Variable behaviour
- May be androgenic
What are the types of germ cell tumours?
- Dysgerminoma (no differentiation)
- Embryonic Group
- Teratoma (embryonic tissues)
- Choriocarcinoma (trophoblastic cells from placenta)
- Endodermal sinus tumour (extraemryonic tissue from amniotic sac)
- Embryonal carcinoma
What are the subtypes of teratomas?
-
Mature Teratoma - most common type of germ cell tumour
- Benign - solid or cystic
- Tissues all mature to adult-type tissues (teeth and hair are very common)
-
Immature Teratoma
- Indicates presence of embryonic elements (most commonly neural tissue)
- Malignant - grows rapidly, penetrates the capsule and forms adhesions
- Spreads within the peritoneal cavity
- Metastasises to the lymph nodes, lungs, liver and other organs
-
Mature Cystic Teratoma with Malignant Transformation
- Rare
- Any type of the mature tissue within the teratoma can become malignant → can give rise to carcinoid, thyroid cancer, BCC, melanoma etc
- Most frequently SCC
Describe vulva pathology.
-
Lichen sclerosus = thinning epithelium with a layer of hyalinisation underneath
- Sometimes associated with epithelial dysplasia and development of malignancy
- Papillary Hidradenoma = benign tumour
-
Malignant Tumours
- Squamous cell carcinoma (85%)
- HPV or lichen sclerosus
- VIN (vulval intraepithelial neoplasia)
- Invasive adenocarcinoma or adenocarcinoma in situ (Paget’s disease)
- Malignant melanoma
- BCC
- Squamous cell carcinoma (85%)
Describe vaginal pathology.
- Congenital anomalies (e.g. absence or atresia)
- Carcinoma (squamous cell carcinoma)
- Adenocarcinoma
- Children of women with threatened abortion treated with diethyl stilbosterol = risk of clear cell carcinoma
- Rhabdomyosarcoma
What are the categories of causes of infertility?
- Congenital
- Hormonal
- Inflammatory
- Neoplastic
- Genetic
- Immunological
What are the causes of acute pancreatitis?
I GET SMASHED:
- Idiopathic (15%)
- Gallstones (50%)
- Ethanol (33%)
- Trauma
- Steroids
- Mumps
- Autoimmune
- Scorpion
- Hyper-calcaemia/-lipidaemia
- Pancreatitis causes hypocalcaemia → if hypercalcaemia is the cause, calcium drops to a normal level
- ERCP
- Drugs - thiazides
What is the pathogenesis of acute / chronic pancreatitis?
- Duct Obstruction
- Gallstone distal to where the common bile duct and pancreatic ducts join → reflux of bile up the pancreatic duct → damage to acini and release of proenzymes which become activated → inflammation / damage
- Alcohol leads to spasm/oedema of the sphincter of Oddi → formation of protein-rich pancreatic fluid → obstructs pancreatic ducts
- Direct Acinar Injury = all other causes
What are the patterns of injury in acute pancreatitis?
- Periductal = necrosis of acinar cells near the ducts (usually secondary to obstruction)
- Perilobular = necrosis at the edges of the lobules (usually due to poor blood supply)
- Panlobular = worsening of periductal or perilobular inflammation

What are the complications of acute pancreatitis?
- Pancreatic
- Pseudocyst formation = collection of fluid without epithelial lining
- Abscess - pseudocysts can become infected leading to abscess formation
- Systemic
- Shock
- Hypoglycaemia
- Hypocalcaemia
What is the prognosis of acute pancreatitis?
- Dependent on severity
- Haemorrhagic pancreatitis = 50% mortality
What are the features of chronic pancreatitis?
- Relapsing or persistent
- Relatively uncommon - 50% associated with acute pancreatitis
- Mortality of 3% per year
What are the causes of chronic pancreatitis?
I GET SMASHED + Chronic disease
- Idiopathic
- Gallstones
- Ethanol (80%)
- Trauma
- Steroids
- Mumps
- Autoimmune
- Scorpion
- Hyper-calcaemia/-lipidaemia
- ERCP
- Drugs - thiazides
- Chronic disease
- Haemochromatosis
- Cystic fibrosis
What are the patterns of injury in chronic pancreatitis?
- Chronic inflammation with parenchymal fibrosis and loss of parenchyma (ascini become atrophic)
-
Duct strictures with calcified stones with secondary dilatations
- Pancreatic calcifications are diagnostic of chronic pancreatitis
What are the complications of chronic pancreatitis?
- Early = Malabsorption
- Late = Diabetes mellitus (endocrine parts survive much longer than exocrine components)
- Pseudocysts - also complication of acute
- Carcinoma of the pancreas
What is the histology of pancreatic pseudocysts?
- Lined by fibrous tissue (no epithelial lining)
- Contains fluid (rich in pancreatic enzymes or necrotic material)
- Connects with pancreatic ducts

What are the outcomes of pancreatic pseudocysts?
- Resolve
- Perforate
- Compress adjacent structures
- Infected
Describe IgG4-related pancreatitis?
- Characterised by large numbers of IgG4 positive plasma cells
- May involve the pancreas, bile ducts and almost any other part of the body
- Histology = duct is surrounded by loads of IgG4 expressing plasma cells
- Patients respond very well to steroids

What are the types of pancreatic tumours?
-
Carcinomas
- Ductal (85% of all neoplasms)
- Increasingly common with age; M>F (2: 1)
- 5-year survival = 5% = 5% of all cancer deaths
- Pre-malignant bridges; 95% k-ras mutation
- Acinar
- Acinar-ductal metaplasia
- Associated with increased serum lipase
- Ductal (85% of all neoplasms)
-
Cystic Neoplasms
- Serous cystadenoma
- Mucinous cystic neoplasm (usually benign)
- Pancreatic Neuroendocrine Tumours (Islet cell tumours)
What are the risk factors for pancreatic cancers?
- Smoking
- BMI
- Dietary factors
- Chronic pancreatitis
- Diabetes mellitus
What are the pathways to ductal carcinoma?
- 2 types of dysplastic ductal lesions
- Pancreatic Intraductal Neoplasia (PanIN)
- Intraductal Mucinous Papillary neoplasm - doesn’t invade through the BM
- K-Ras mutations are present in 95% of cases
What is the pathology of ductal carcinoma?
- Macroscopic
- Gritty and grey
- Invades adjacent structures
- Tumours in the head present earlier
- Microscopic
- Adenocarcinomas
- Secrete mucin (stain for mucin)
- Form glands
- Set in desmoplastic stroma (i.e. tumour induces fibrous tissue growth around it)
- Adenocarcinomas
What are the most common sites of ductal carcinoma and neuroendocrine tumours of the pancreas?
Ductal Carcinoma = Head > Body > Tail
Neuroendocrine = Tail > Body > Head
What are the complications of ductal carcinoma?
- Metastases
- Chronic pancreatitis
- Venous thrombosis
- Circulating pancreatic cancer cells releasing mucous which activates the clotting cascade
Describe cystic pancreatic tumours?
- Serous cystadenoma + Mucinous cystic neoplasm
- Contain serous or mucin secreting epithelium (like ovarian tumours)
- Usually benign
Describe pancreatic endocrine tumours.
- Usually non-secretory
- Stained by neuroendocrine markers (chromogranin stain)
- Behaviour is difficult to predict
What are the types of pancreatic endocrine neoplasms?
- Insulinomas = most common type of functional tumour
- Derived from beta cells
- Whipple’s triad
- Glucose <50mg/dL
- S/S hypo
- Relief on glucose administration
- MEN1
- Pituitary adenoma
- Parathyroid hyperplasia
- Pancreatic tumours
What are the risk factors for gallstones?
- Crohn’s disease
- Diabetes mellitus
- High triglyceride + low fibre diet
- Female
- Ethnicity (e.g. Native Americans)
- >40
- Medication:
- Somatostatin analogue (octreotide)
- Glucagon-like peptide-1 analogues
- Ceftriaxone
- COCP / HRT
- Non-alcoholic fatty liver disease
- Obesity
- Weight loss – particularly if fast
- Hereditary factors (e.g. disorders of bile metabolism)
What are the types of gallstones?
- Cholesterol
- >50% cholesterol
- May be single
- Mostly radiolucent - NOT seen on a plain abdominal X-ray → must USS
- Pigment (contain calcium salts of unconjugated bilirubin)
- Often multiple
- Mostly radio-opaque (because they contain calcium)
What are the complications of gallstones?
MOST PEOPLE do not have any problems
- Bile duct obstruction
- Acute and chronic cholecystitis
- Pancreatitis
- Gallbladder cancer
What is the histology of acute and chronic cholecystitis?
- Acute cholecystitis
- Acute inflammation = neutrophils, oedema
- 90% are associated with gallstones
- Chronic cholecystitis
- 90% contain gallstones
- Fibrosis, small, neoangiogenesis
- Diverticula (Rokitansky-Aschoff sinuses)
- Contracts against obstruction → diverticula
Describe gallstone cancer.
- Adenocarcinoma → technically a type of cholangiocarcinoma
- 90% associated with gallstones
- Uncommon


