Hemostasis Flashcards
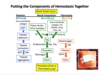
What 3 broad actions need to happen for a clot to form?
Vessel constriction
Platelet plug formation
Fibrin formation
The normal hemostatic system limits blood loss by precisely regulated interactions between components of the:
vessel wall, circulating blood platelets, and plasma proteins
___, ___, and ___ are common clinical manifestations of many diseases.
Hemorrhage, intravascular thrombosis, and embolism
Formation of a hemostatic plug (thrombus or clot) is derived from platelets and fibrin strands, in which ____ are trapped.
RBC’s/WBC’s
Define hemostasis:
Hemostasis is the arrest of bleeding following vascular injury
Hemostasis is dependent on intricate interactions between:
–Platelet adhesion and aggregation,
–Endothelial cell function,
–Blood coagulation system
–Clot lysis (fibrinolysis) system.
The components that comprise platelet aggregation/ endothelium, coagulation and fibrinolysis also termed:
primary, secondary and tertiary hemostasis, respectively
To stabilize platelet plug you need ____. In a hemophiliac, you can’t stabilize platelet plug so the patient continues to bleed.
fibrin
Blood vessels are considered to be a(n) ______ surface, to prevent a clot from forming on their surface.
anticoagulant
Platelets help maintain the ____ of the vessel lining, and they ___ any rupture in the circulatory vessels.
Platelets help maintain the integrity of the vessel lining, and they plug any rupture in the circulatory vessels.
What is a normal platelet count?
Between 150-450x10^9/L
Normal platelet lifespan is:
7-10
Coagulation factors interact in a highly ordered sequence with the ultimate object of converting _____ to insoluble ____ that stabilizes the primary hemostatic plug.
Coagulation factors interact in a highly ordered sequence with the ultimate object of converting soluble fibrinogen to insoluble fibrin that stabilizes the primary hemostatic plug.
Which coagulation factors are zymogens/active enzymes?
Vitamin K-dependent – factors II, VII, IX, X
Vitamin K-independent– factors XI, XII, and XIII
What are important protein and non-protein cofactors in secondary hemostasis?
Protein: Factor V, factor VIII, tissue factor, and von Willebrand factor (vWF)
Non-protein: Calcium (in blood) and phospholipid surfaces (from cells)
Which two coagulation factors are especially important in controlling coagulation?
Factor VII and Factor VII
These have short half-lives and are present in small amounts in the blood
In screening tests of coagulation, blood is collected and kept from clotting by a ____ sequestering agent
calcium-sequestering (e.g. citrate)
Coagulation is initiated in screening tests by adding an activating agent such as:
calcium and phospholipid
Routine coagulation tests include:
Prothrombin time (PT)
Activated Partial Thromboplastin Time (aPTT)
Thrombin Time (TT) = Thrombin clotting time (TCT)
The Thrombin Time (TT) test measures what?
The conversion of fibrinogen to fibrin.
Add thrombin to the tube to directly measure the conversion, taking no other factors into account.
How is a Thrombin Time test performed?
Thrombin is added to a citrated plasma tube of blood, and the time until a clot forms is recorded (in seconds).
NOTE: calcium and phospholipid are NOT required for TT
What causes a prolonged TT?
1. Low fibrinogen (hypofibrinogenemia)
2. Abnormal fibrinogen (dysfibrinogenemia)
- inherited
- acquired (severe liver disease)
3. Inhibitor of added thrombin
- direct inhibitor; e.g. argatroban, dabigatran
- indirect inhibitor; heparin
- Something that interferes with fibrin polymerization
- paraproteinemia (from myeloma or Waldenstroms)
- very high levels of fibrin degradation products
What drugs are direct inhibitors of added thrombin in a TT test?
Argatroban
Dabigatran
What drugs are indirect inhibitors of thrombin, causing a prolonged TT?
Heparin
(causes problems by interacting with antithrombin)
How is the Prothrombin Time test performed?
Thromboplastin and Calcium are added to citrated plasma. The time until a clot forms is recorded.

What are the essential components of the secondary hemostasis coagulation cascade?
The extrinsic pathway consists of Factor VII and tissue factor with tissue factor considered to be “extrinsic” to the bloodstream. Factor VII, when activated, forms a complex with tissue factor that converted factor X to activated factor X (factor Xa). The intrinsic system, consisting of factors XII, XI, X and IX, leads to the formation of a complex of factor IXa with its cofactor, factor VIIIa, which in the presence of phospholipid and calcium can also convert factor X to Xa. Factor Xa, as the enzyme, forms a complex with its cofactor, factor Va, and rapidly converted prothrombin to thrombin. This reaction requires a phospholipid surface and calcium. Once thrombin is formed, fibrinogen is converted to fibrin monomers that polymerize to form a fibrin clot. Thrombin activates factors V, VIII, XI and XIII in important feedback steps.

The thromboplastin reagent contains WHAT?
Tissue Factor and Phospholipid
What causes a prolonged PT?
•Anything that prolongs the TT (BUT the PT is much less sensitive than the TT to the presence of heparin, abnormal fibrinogen, and FDPs)
•Anything that lowers levels or inhibits the common pathway factors
- Factor X
- Factor V
- Factor II (prothrombin)
- Fibrinogen
•And also low levels of FVII, which can arise:
- Congenital
- Acquired
- Deficiency of Vitamin K
- Vitamin K inhibitors
- DIC
- Liver disease