Hematology/Oncology Flashcards
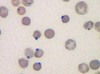
Anisocytosis
RBCs of varying sized
Poikilocytosis
RBCs of varying shapes
Bluish color on Wright-Giemsa stain of reticulocytes represents what?
Residual ribosomal RNA
vWF receptor
Gp1b
Fibrinogen receptor
Gp2b/3a
Neutrophil chemotactic factors
C5a
IL-8
LTB4
Kallikrein
Platelet-activating Factor
What cell differentiates into macrophages?
Monocytes
Macrophages are activated by what?
Gamma-interferon
What binds to macrophages to initiate septic shock? Where does it bind?
Lipid A from bacterial LPS
Binds to CD14 ON macrophages
Causes of eosinophilia
NAACP
Neoplasia
Asthma
Allergic process
Chronic adrenal insufficiency
Parasites (invasive)
What 2 substances are produced by Eosinophils?
Histaminase
Major basic protein (helminthotoxin)
Basophils contain/release what 3 substances?
Heparin
Histamine
Leukotrienes
Basophilia is uncommon, but can be a sign of what?
CML
(myeloproliferative disease)
Mast cells are involved in what type of hypersensitivity reaction?
Type 1
Mast cells bind IgE how?
Via Fc portion of IgE membrane
Mast cells release what 4 things?
Histamine
Heparin
Tryptase
Eosinophil chemotactic factors
What prevents mast cells degranulation?
Cromolyn Sodium
(used for asthma prophylaxis)
Langerhans cells are what?
Dendritic cells in the skin
Plasma cell cancer
Multiple Myeloma
Clock-face chromatin
Eccentric nucleus
Abundant RER
Well-developed Golgi Apparatus
Found in Bone Marrow
Plasma Cells
Location of Fetal Erythropoiesis
Yolk Sac (3-8 weeks)
Liver (6 wks - birth)
Spleen (10-28 weeks)
BM (18 weeks - adult)
What is the benefit of HbF?
HbF has a higher affinity for oxygen because of less avid binding of 2,3-BPG.
This allows HbF to extract oxygen from maternal hemoglobin across the placenta.
Blood type = universal recipient of RBCs
AB
Blood type = universal recipient of plasma
O