General neurology stuff COPIED Flashcards
Cycloplegia
paralysis of accommodation
dysarthria
slurred speech caused by articulation problems due to a motor deficit.
Dysphonia
loss of volume caused by laryngeal disorders.
Odynophagia
Pain on swallowing
Possible causes; infection, oesophageal cancer, larnynx or pharynx cancer.
Dysphagia
Difficulty swallowing
possible causes; pharyngitis, oesophageal disease
xerostomia
dry mouth
possible causes; anticholinergic drugs, Sjogren’s syndrome
Where’s the extradural space?
between the skull and the dura. Especially at the frontoparietal area. Other areas dura can be tightly bound to the skull.
cause: often tearing of middle meningeal artery.
Where’s the subdural space, and who’s vulnerable?
The elderly; tearing of the veins across the subdural space causing gradual seepage of blood
What is the main inhibitory neurotransmitter?
GABA (Gamma-Aminobutyric acid)
Papilloedema
Optic disc swelling; increased intracranial pressure.
Usually bilateral and can occur over a period of hours to weeks. Unilateral presentation is extremely rare.
May be asymptomatic or with a headache.
Ataxia
A term for a group of disorders that affect co-ordination, balance and speech.

A gumma is a soft, non-cancerous growth resulting from the tertiary stage of syphilis.
Gummas are most commonly found in the liver (gumma hepatis), but can also be found in brain, heart, skin, bone, testis, and other tissues.
paraparesis
partial paralysis of both legs.
(in contrast to paraplegia)

Polyneuropathy ; affects peripheral nerves
same areas on both sides of the body; featuring weakness, numbness, and burning pain.
It usually begins in the hands and feet and may progress to the arms and legs; May be caused by diabetes and Guillain–Barré syndrome.
Iris contraction/ pupil smaller
miosis
(pilocarpine causes this)

Extend the knee whilst the hip is in 90 degree flexion.
- positive if pain on extension. Sign is absent in local causes of neck stiffness.
NB> absence of this sign does not exclude meningitis.
Romberg’s sign
Can’t stand steadily with eyes closed.
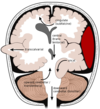
motor speech area located on left hemisphere (dominant side)
Broca’s area
- comprehension okay, repetitive of words difficulty.
Area on dominant side involved with understanding language.
Symptoms of Wernicke’s aphasia are.. (30
Wernicke’s area
symptoms; profound word-finding difficulty,
impaired repetition of words
profound loss of comprehension