Friday [08/10/2021] Flashcards
How do Lacunar strokes typically present? [2]
Lacunar stroke is a type of stroke that results from occlusion of one of the penetrating arteries that provides blood to the brain’s deep structures. Lacunar strokes most commonly present as a pure motor hemiparesis, pure sensory stroke, sensorimotor stroke, ataxic hemiparesis or dysarthria/clumsy hand syndrome.
What is the classification system for strokes? [1]
Oxford Stroke classification
Criteria assessed by the Oxford Stroke Classification [3]
- unilateral hemiparesis and/or hemisensory loss of the face, arm & leg
- homonymous hemianopia
- higher cognitive dysfunction e.g. dysphasia
How do TACI [c.15%] typically present? Which arteries do they involve? [2]
involves middle and anterior cerebral arteries
all 3 of the above criteria are present
Which arteries do PACI [c.25%] typically effect and how do they present? [2]
involves smaller arteries of anterior circulation e.g. upper or lower division of middle cerebral artery
2 of the above criteria are present
Which arteries do lacunar infarcts typically effects [c.25%] and how they present? [4]
involves perforating arteries around the internal capsule, thalamus and basal ganglia
presents with 1 of the following:
1. unilateral weakness (and/or sensory deficit) of face and arm, arm and leg or all three.
2. pure sensory stroke.
3. ataxic hemiparesis
Which arteries do POCI [c.25%] typically effect and what is the presentation? [4]
involves vertebrobasilar arteries
presents with 1 of the following:
1. cerebellar or brainstem syndromes
2. loss of consciousness
3. isolated homonymous hemianopia
What is a lateral medullary stroke? [3]
Lateral medullary syndrome (posterior inferior cerebellar artery)
aka Wallenberg’s syndrome
ipsilateral: ataxia, nystagmus, dysphagia, facial numbness, cranial nerve palsy e.g. Horner’s
contralateral: limb sensory loss
What is Weber’s syndrome and how does it present? [2]
ipsilateral III palsy
contralateral weakness
COPD still breathless despite using SABA/SAMA and a LABA+ICS, what should you add? [1]
A LAMA like inhaled triotropium
General Mx of COPD [4]
>smoking cessation advice: including offering nicotine replacement therapy, varenicline or bupropion
annual influenza vaccination
one-off pneumococcal vaccination
pulmonary rehabilitation to all people who view themselves as functionally disabled by COPD (usually Medical Research Council [MRC] grade 3 and above)
bronchodilator therapy initially in COPD [2]
a short-acting beta2-agonist (SABA) or short-acting muscarinic antagonist (SAMA) is first-line treatment
for patients who remain breathless or have exacerbations despite using short-acting bronchodilators the next step is determined by whether the patient has ‘asthmatic features/features suggesting steroid responsiveness’
Criteria to determine if patient has asthmatic/steroid responsiveness features []4
any previous, secure diagnosis of asthma or of atopy
a higher blood eosinophil count - note that NICE recommend a full blood count for all patients as part of the work-up
substantial variation in FEV1 over time (at least 400 ml)
substantial diurnal variation in peak expiratory flow (at least 20%)
How to Tx patient if no asthmatic features/features suggesting steroid responsiveness? [2]
add a long-acting beta2-agonist (LABA) + long-acting muscarinic antagonist (LAMA)
if already taking a SAMA, discontinue and switch to a SABA
How to Tx a patient if they have asthmatic features/features suggesting steroid repsiveness? [3]
LABA + inhaled corticosteroid (ICS)
if patients remain breathless or have exacerbations offer triple therapy i.e. LAMA + LABA + ICS
if already taking a SAMA, discontinue and switch to a SABA
NICE recommend the use of combined inhalers where possible
When to include oral theophylline in Tx for COPD? []2
NICE only recommends theophylline after trials of short and long-acting bronchodilators or to people who cannot used inhaled therapy
the dose should be reduced if macrolide or fluoroquinolone antibiotics are co-prescribed
When to include prophylactic antibiotic therapy for COPD Tx [4]
azithromycin prophylaxis is recommended in select patients
patients should not smoke, have optimised standard treatments and continue to have exacerbations
other prerequisites include a CT thorax (to exclude bronchiectasis) and sputum culture (to exclude atypical infections and tuberculosis)
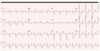
LFTs and an ECG to exclude QT prolongation should also be done as azithromycin can prolong the QT interval
What should be done before giving azithromycin prophylaxis for COPD patients? [2]
LFTs and an ECG to exclude QT prolongation should also be done as azithromycin can prolong the QT interval
When should mucolytics be considered in COPD patients? [1]
should be ‘considered’ in patients with a chronic productive cough and continued if symptoms improve
Features of Cor pulmonale and how to Tx [3]
features include peripheral oedema, raised jugular venous pressure, systolic parasternal heave, loud P2
use a loop diuretic for oedema, consider long-term oxygen therapy
ACE-inhibitors, calcium channel blockers and alpha blockers are not recommended by NICE
Factors which may improve survival in patients with stable COPD [3]
smoking cessation - the single most important intervention in patients who are still smoking
long term oxygen therapy in patients who fit criteria
lung volume reduction surgery in selected patients
WHen is electroconvulsive therapy considered? [2]
Electroconvulsive therapy is a useful treatment option for patients with severe depression refractory to medication (e.g. catatonia) those with psychotic symptoms. For catatonic schizophrenai and severe mania too.
What is the only absolute CI to ECT? [1]
The only absolute contraindications is raised intracranial pressure.
Short-term SE of ECT? [5]
headache
nausea
short term memory impairment
memory loss of events prior to ECT
cardiac arrhythmia
Long-term SE of ECT [1]
some patients report impaired memory
What is done first-line during endoscopy to stop bleeding? [1]
Band ligation
Acute Tx of variceal haemorrhage [7]
ABC: patients should ideally be resuscitated prior to endoscopy
correct clotting: FFP, vitamin K
vasoactive agents:
terlipressin is currently the only licensed vasoactive agent and is supported by NICE guidelines. It has been shown to be of benefit in initial haemostasis and preventing rebleeding
octreotide may also be used although there is some evidence that terlipressin has a greater effect on reducing mortality
prophylactic IV antibiotics have been shown to reduce mortality in patients with liver cirrhosis. Quinolones are typically used. NICE support this in their 2016 guidelines: ‘Offer prophylactic intravenous antibiotics for people with cirrhosis who have upper gastrointestinal bleeding.’
both terlipressin and antibiotics should be given before endoscopy in patients with suspected variceal haemorrhage
endoscopy: endoscopic variceal band ligation is superior to endoscopic sclerotherapy. NICE recommend band ligation
Sengstaken-Blakemore tube if uncontrolled haemorrhage
Transjugular Intrahepatic Portosystemic Shunt (TIPSS) if above measures fail
connects the hepatic vein to the portal vein
exacerbation of hepatic encephalopathy is a common complication
What should be given before endoscopy if being given? [2]
both terlipressin and antibiotics should be given before endoscopy in patients with suspected variceal haemorrhage [Abx given those with liver cirrhosis]
If endoscopic measures fail to control variceal bleed,what is done next? [2]
Sengstaken-Blakemore tube if uncontrolled haemorrhage
Transjugular Intrahepatic Portosystemic Shunt (TIPSS) if above measures fail
connects the hepatic vein to the portal vein
exacerbation of hepatic encephalopathy is a common complication
What are prophlyactic measures for variceal haemorrhages? [2]
propranolol: reduced rebleeding and mortality compared to placebo
endoscopic variceal band ligation (EVL) is superior to endoscopic sclerotherapy. It should be performed at two-weekly intervals until all varices have been eradicated. Proton pump inhibitor cover is given to prevent EVL-induced ulceration. This is supported by NICE who recommend: ‘Offer endoscopic variceal band ligation for the primary prevention of bleeding for people with cirrhosis who have medium to large oesophageal varices.’
third step for asthma Mx in 5-16 y/o
1 - SABA
2 - SABA + paediatric low-dose inhaled ICS
3 - SABA + paediatric low-dose inhaled ICS + LTRA
Prophylaxis for migraines [2]
NICE advise either topiramate or propranolol ‘according to the person’s preference, comorbidities and risk of adverse events’. Propranolol should be used in preference to topiramate in women of child bearing age as it may be teratogenic and it can reduce the effectiveness of hormonal contraceptives
Acute Tx for migraines [2]
first-line: offer combination therapy with an oral triptan and an NSAID, or an oral triptan and paracetamol
Which cancer are transplant patient at paritcular risk from? [1]
Patients who have received an organ transplant are at risk of skin cancer (particularly squamous cell carcinoma) due to long-term use of immunosuppressants
Which renal transplant drugs can cause CVD? [2]
Cardiovascular disease - tacrolimus and ciclosporin can cause hypertension and hyperglycaemia. Tacrolimus can also cause hyperlipidaemia. Patients must be monitored for accelerated cardiovascular disease.
Which renal transplant drugs can cause renal failure? [2]
Renal failure - due to nephrotoxic effects of tacrolimus and ciclosporin/graft rejection/recurrence of original disease in transplanted kidney
What must be monitored with eryhroderma? [3]
SoB:
- Inpatient treatment for erythroderma must be monitored for complications like dehydration, infection and high-output heart failure
What is erythroderma? [1]
When more than 95% of the skin is involved in a rash of any kind
Causes of erythroderma [5]
eczema
psoriasis
drugs e.g. gold
lymphomas, leukaemias
idiopathic
What is erythrodermic psoriasis and how should it be Mx? [2]
may result from progression of chronic disease to an exfoliative phase with plaques covering most of the body. Associated with mild systemic upset
more serious form is an acute deterioration. This may be triggered by a variety of factors such as withdrawal of systemic steroids. Patients need to be admitted to hospital for management
Sx of liver abscesses [2]
Raised inflammatory markers, RUQ pain and fever
How are liver abscesses Mx? [2]
Combination of antibiotics and drainage
Most common orgnaisms found in pyogenic liver abscesses [2]
The most common organisms found in pyogenic liver abscesses are Staphylococcus aureus in children and Escherichia coli in adults.
Which Abx are used in Mx of liver abscesses? [3]
drainage (typically percutaneous) and antibiotics
amoxicillin + ciprofloxacin + metronidazole
if penicillin allergic: ciprofloxacin + clindamycin
Target levels for blood glucose in pregnant women [3]
Pregnant women with GDM should be advised to maintain their CBGs below the following target levels:
fasting: 5.3mmol/L
AND
1 hour postprandial: 7.8 mmol/L or
2 hours postprandial: 6.4 mmol/L
If blood glucose targets are not met by metformin/lifestyle, what should be done? [2]
If these targets are not met with diet, exercise and metformin, then insulin should be offered as add-on therapy.
When do Sx start of alcohol withdrawal? [1]
Between 6-12 hours
when do seizures, adn when does delirium tremens begin with alcohol? [2]
Alcohol withdrawal
symptoms: 6-12 hours
seizures: 36 hours
delirium tremens: 72 hours
Frist-line Mx of delirium tremens [2]
first-line: long-acting benzodiazepines e.g. chlordiazepoxide or diazepam. Lorazepam may be preferable in patients with hepatic failure. Typically given as part of a reducing dose protocol
Sx of alcohol withdrawal [1]
tremor, sweating, tachycardia, anxiety
Which drugs can cause cataracts? [1]
Steroids
Which drugs can cause corneal opacities? [2]
amiodarone
indomethacin
Which drugs can cause optic neuritis? [3]
ethambutol
amiodarone
metronidazole
Which drugs can cause retinopathy? [2]
chloroquine, quinine
What type of herpes are genital ulcers caused by? [1]
Genital herpes is most often caused by the herpes simplex virus (HSV) type 2 (cold sores are usually due to HSV type 1)
Sx of primary attacks from Herpes [2]
Primary attacks are often severe and associated with fever whilst subsequent attacks are generally less severe and localised to one site. There is typically multiple painful ulcers.
What is syphilis caused by and what is the presentation of it? [2]
Syphilis is a sexually transmitted infection caused by the spirochaete Treponema pallidum. Infection is characterised by primary, secondary and tertiary stages. A painless ulcer (chancre) is seen in the primary stage. The incubation period= 9-90 days.
What is Chancroid caused by and how does it present? [2]
Chancroid is a tropical disease caused by Haemophilus ducreyi. It causes painful genital ulcers associated with unilateral, painful inguinal lymph node enlargement. The ulcers typically have a sharply defined, ragged, undermined border.
What is LGV caused by and how does it present? [2]
Lymphogranuloma venereum (LGV) is caused by Chlamydia trachomatis. Typically infection comprises of three stages
stage 1: small painless pustule which later forms an ulcer
stage 2: painful inguinal lymphadenopathy
stage 3: proctocolitis
How is LGV Tx? [1]
Doxycycline
Immediate frist aid for burns [4]
airway, breathing, circulation
burns caused by heat: remove the person from the source. Within 20 minutes of the injury irrigate the burn with cool (not iced) water for between 10 and 30 minutes. Cover the burn using cling film, layered, rather than wrapped around a limb
electrical burns: switch off power supply, remove the person from the source
chemical burns: brush any powder off then irrigate with water. Attempts to neutralise the chemical are not recommended
How to assess the extent of the burn [3]
Wallace’s Rule of Nines: head + neck = 9%, each arm = 9%, each anterior part of leg = 9%, each posterior part of leg = 9%, anterior chest = 9%, posterior chest = 9%, anterior abdomen = 9%, posterior abdomen = 9%
Lund and Browder chart: the most accurate method
the palmar surface is roughly equivalent to 1% of total body surface area (TBSA). Not accurate for burns > 15% TBSA
When to refer to secondary care? [3]
all deep dermal and full-thickness burns.
superficial dermal burns of more than 3% TBSA in adults, or more than 2% TBSA in children
superficial dermal burns involving the face, hands, feet, perineum, genitalia, or any flexure, or circumferential burns of the limbs, torso, or neck
any inhalation injury
any electrical or chemical burn injury
suspicion of non-accidental injury
What is the PP of severe burns? [3]
Following the burn, there is a local response with progressive tissue loss and release of inflammatory cytokines. Systemically, there are cardiovascular effects resulting from fluid loss and sequestration of fluid into the third space. There is a marked catabolic response. Immunosupression is common with large burns and bacterial translocation from the gut lumen is a recognised event. Sepsis is a common cause of death following major burns.
How to Mx more severe burns [3]
The initial aim is to stop the burning process and resuscitate the patient. Intravenous fluids will be required for children with burns greater than 10% of total body surface area. Adults with burns greater than 15% of total body surface area will also require IV fluids. The fluids are calculated using the Parkland formula which is; volume of fluid= total body surface area of the burn % x weight (Kg) x4. Half of the fluid is administered in the first 8 hours. A urinary catheter should be inserted. Analgesia should be given. Complex burns, burns involving the hand perineum and face and burns >10% in adults and >5% in children should be transferred to a burns unit.
When to conservatively manage burns? [2]
Conservative management is appropriate for superficial burns and mixed superficial burns that will heal in 2 weeks. More complex burns may require excision and skin grafting. Excision and primary closure is not generally practised as there is a high risk of infection.
What are escharotomies and when are they used? [2]
Indicated in circumferential full thickness burns to the torso or limbs.
Careful division of the encasing band of burn tissue will potentially improve ventilation (if the burn involves the torso), or relieve compartment syndrome and oedema (where a limb is involved)
Mx of scabies [4]
Treating the affected person and all household members, close contacts, and sexual contacts with a topical insecticide (e.g. permethrin 5% cream or malathion 0.5% liquid), even in the absence of symptoms.
Guidance of Tx for households with scabies [4]
avoid close physical contact with others until treatment is complete
all household and close physical contacts should be treated at the same time, even if asymptomatic
launder, iron or tumble dry clothing, bedding, towels, etc., on the first day of treatment to kill off mites.
Features of scabies
widespread pruritus
linear burrows on the side of fingers, interdigital webs and flexor aspects of the wrist
in infants, the face and scalp may also be affected
secondary features are seen due to scratching: excoriation, infection
What is obese class 1? [1]
Overweight is 25-30, obese class 1 is 30-35
Step-wise approach to managing obesity [3]
conservative: diet, exercise
medical
surgical
MoA of Orlistat and adverse effects of the drug [2]
Orlistat is a pancreatic lipase inhibitor used in the management of obesity. Adverse effects include faecal urgency/incontinence and flatulence
What is the lower dose version now available [2]
A lower dose version is now available without prescription (‘Alli’).
Which adults can be given orlistat? [4]
BMI of 28 kg/m^2 or more with associated risk factors, or
BMI of 30 kg/m^2 or more
continued weight loss e.g. 5% at 3 months
orlistat is normally used for < 1 year
When are women covered by the lactational amenorrhoea method? [LAM] [1]
She is having unprotected intercourse and will not be covered by the lactational amenorrhea method (LAM) as the baby is getting less than 85% of its feeds as breast milk (NICE CKS: Contraception - natural family planning)
If not covered by LAM, when are women art risk of prognancy from unprototected sex? [2]
If not covered by the LAM, women are at risk of pregnancy from unprotected intercourse from day 21 postpartum
When is COCOP CI? [1]
The COCP is absolutely contraindicated (UKMEC 4) for women who are breastfeeding less than 6 weeks post-partum
Are women allowed to have the COCP 7w post-partum? [2]
However, this lady is seven weeks postpartum meaning she falls into the 6 weeks - 6 months postpartum guidance, in which the COCP is categorised as UKMEC2 for breastfeeding women. This means that advantages of prescribing the COCP would generally outweigh the disadvantages and based on the FRSH advice regarding the COCP, NICE clinical knowledge summaries recommend
WHen can women start the PIP? [3]
the FSRH advise ‘postpartum women (breastfeeding and non-breastfeeding) can start the POP at any time postpartum.’
after day 21 additional contraception should be used for the first 2 days
a small amount of progestogen enters breast milk but this is not harmful to the infant
When can women start the COC? [4]
absolutely contraindicated - UKMEC 4 - if breast feeding < 6 weeks post-partum
UKMEC 2 - if breast feeding 6 weeks - 6 months postpartum*
the COC may reduce breast milk production in lactating mothers
may be started from day 21 - this will provide immediate contraception
after day 21 additional contraception should be used for the first 7 days
When can an IUD or IUD be inserted owmne a women post-partum? [1]
The intrauterine device or intrauterine system can be inserted within 48 hours of childbirth or after 4 weeks.
How effective is LAM? [2]
is 98% effective providing the woman is fully breast-feeding (no supplementary feeds), amenorrhoeic and < 6 months post-partum
Problems with Inter-pregnancy interval being shortened? [2]
An inter-pregnancy interval of less than 12 months between childbirth and conceiving again is associated with an increased risk of preterm birth, low birthweight and small for gestational age babies.
What is pre-eclampsia defined as? [2]
Pre-eclampsia is defined as new-onset BP ≥ 140/90 mmHg after 20 weeks AND ≥ 1 of proteinuria or organ dysfunction
Consequences of pre-eclampsia [4]
eclampsia
other neurological complications include altered mental status, blindness, stroke, clonus, severe headaches or persistent visual scotomata
fetal complications
intrauterine growth retardation
prematurity
liver involvement (elevated transaminases)
haemorrhage: placental abruption, intra-abdominal, intra-cerebral
cardiac failure
Features of severe pre-eclampsia [4]
hypertension: typically > 160/110 mmHg and proteinuria as above
proteinuria: dipstick ++/+++
headache
visual disturbance
papilloedema
RUQ/epigastric pain
hyperreflexia
platelet count < 100 * 106/l, abnormal liver enzymes or HELLP syndrome
High RF for pre-eclampsia [5]
hypertensive disease in a previous pregnancy
chronic kidney disease
autoimmune disease, such as systemic lupus erythematosus or antiphospholipid syndrome
type 1 or type 2 diabetes
chronic hypertension
Moderate RF for pre-eclamspia [4]
first pregnancy
age 40 years or older
pregnancy interval of more than 10 years
body mass index (BMI) of 35 kg/m² or more at first visit
family history of pre-eclampsia
multiple pregnancy
What should be given and whom to to reduce the risk of pre-eclampsia in pregnannt women? [2]
Reducing the risk of hypertensive disorders in pregnancy
women with the following should take aspirin 75-150mg daily from 12 weeks gestation until the birth
≥ 1 high risk factors
≥ 2 moderate factors
Which women will admitted and observed for risk of pre-eclampsia in pregnancy? [2]
Initial assessment
NICE recommend arranging emergency secondary care assessment for any woman in whom pre-eclampsia is suspected
women with blood pressure ≥ 160/110 mmHg are likely to be admitted and observed
First-line, and defintive Mx of pre-eclampsia in pregnancy [2]
oral labetalol is now first-line following the 2010 NICE guidelines. Nifedipine (e.g. if asthmatic) and hydralazine may also be used
delivery of the baby is the most important and definitive management step. The timing depends on the individual clinical scenario
What can be used for pre-eclampsia if women if asthmatic and can;t have oral labetolol? [1]
Nifedipine
Which type of Herpes causes oral lesions? [1]
There are two strains of the herpes simplex virus (HSV) in humans: HSV-1 and HSV-2. Whilst it was previously thought HSV-1 accounted for oral lesions (cold sores) and HSV-2 for genital herpes it is now known there is considerable overlap
Features of Herpes Simplex virus [3]
primary infection: may present with a severe gingivostomatitis
cold sores
painful genital ulceration
Mx of gingivomastitis vs cold sores vs genital herpes [3]
gingivostomatitis: oral aciclovir, chlorhexidine mouthwash
cold sores: topical aciclovir although the evidence base for this is modest
genital herpes: oral aciclovir. Some patients with frequent exacerbations may benefit from longer term aciclovir
How should women with Herpes at pregnancy be Tx? [2]
elective caesarean section at term is advised if a primary attack of herpes occurs during pregnancy at greater than 28 weeks gestation
women with recurrent herpes who are pregnant should be treated with suppressive therapy and be advised that the risk of transmission to their baby is low
What are patietns with Addison’s disease given? [2]
Patients who have Addison’s disease are usually given both glucocorticoid and mineralocorticoid replacement therapy.
Which drugs does that mean they are given [2]
hydrocortisone: usually given in 2 or 3 divided doses. Patients typically require 20-30 mg per day, with the majority given in the first half of the day
fludrocortisone
Which part of patient educatio is important with Addison disease Tx? [3]
emphasise the importance of not missing glucocorticoid doses
consider MedicAlert bracelets and steroid cards
patients should be provided with hydrocortisone for injection with needles and syringes to treat an adrenal crisis
discuss how to adjust the glucocorticoid dose during an intercurrent illness (see below)
Mx of intercurrent illness of Addison’s disease [2]
in simple terms the glucocorticoid dose should be doubled, with the fludrocortisone dose staying the same
the Addison’s Clinical Advisory Panel have produced guidelines detailing particular scenarios - please see the CKS link for more details
Associations of adhesive capsulitis [1]
diabetes mellitus: up to 20% of diabetics may have an episode of frozen shoulder
Features of adhesive capsulitis [4]
external rotation is affected more than internal rotation or abduction
both active and passive movement are affected
patients typically have a painful freezing phase, an adhesive phase and a recovery phase
bilateral in up to 20% of patients
the episode typically lasts between 6 months and 2 years
Mx of adhesive capsulitis [2]
no single intervention has been shown to improve outcome in the long-term
treatment options include NSAIDs, physiotherapy, oral corticosteroids and intra-articular corticosteroids
What is Trichomonas vaginalis? [1]
Trichomonas vaginalis is a highly motile, flagellated protozoan parasite. Trichomoniasis is a sexually transmitted infection (STI).
Features of Trichomonas vaginalis [5]
vaginal discharge: offensive, yellow/green, frothy
vulvovaginitis
strawberry cervix
pH > 4.5
in men is usually asymptomatic but may cause urethritis
Microscopy of TV [2]
microscopy of a wet mount shows motile trophozoites
Mx of TV [2]
oral metronidazole for 5-7 days, although the BNF also supports the use of a one-off dose of 2g metronidazole
Which receptors are attacked at the NMJ in myasthenia gravis? [2]
Myasthenia gravis is an autoimmune condition whereby the patient’s immune system attacks the acetylcholine receptors at the neuromuscular junction. Symptoms include weakness, especially in the evening. Treatment is focused on increasing the concentration of acetylcholine in the synaptic cleft using acetylcholinesterase inhibitors.
WEhat would GBS look like on NCS? [2]
Guillan-barre syndrome is an autoimmune condition. It has no known causes but often occurs after an episode of infection or immunization. Both conditions are associated with slowed motor conduction on nerve conduction studies.
Does MND present as LMN or UMN? [1]
Motor neuron disease is a neurological condition of unknown cause which can present with both upper and lower motor neuron signs. It rarely presents before 40 years and various patterns of disease are recognised including amyotrophic lateral sclerosis, progressive muscular atrophy and bulbar palsy.
Are there sensory signs/Sx in MND? [4]
fasciculations
the absence of sensory signs/symptoms*
the mixture of lower motor neuron and upper motor neuron signs
wasting of the small hand muscles/tibialis anterior is common
Are eyes effected in MND? [1]
doesn’t affect external ocular muscles
no cerebellar signs
abdominal reflexes are usually preserved and sphincter dysfunction if present is a late feature
What will NCS, electromyography and MRI in MND show? [3]
The diagnosis of motor neuron disease is clinical, but nerve conduction studies will show normal motor conduction and can help exclude a neuropathy. Electromyography shows a reduced number of action potentials with increased amplitude. MRI is usually performed to exclude the differential diagnosis of cervical cord compression and myelopathy
Which signs are seen in ALS? [2]
affects both upper (corticospinal tracts) and lower motor neurons
results in a combination of upper and lower motor neuron signs
Which neuron signs are seen in poliomyelitis? [1]
affects anterior horns resulting in lower motor neuron signs
Which tracts are affected in Brown-Sequard syndrome [spinal cord hemisection? [3]
- Lateral corticospinal tract
- Dorsal columns
- Lateral spinothalamic tract
How does Brown-Sequard syndrome present? [3]
- Ipsilateral spastic paresis below lesion
- Ipsilateral loss of proprioception and vibration sensation
- Contralateral loss of pain and temperature sensation
Which tracts are affected in Freidrich’s ataxia? [1]
Same as subacute combined degeneration of the spinal cord (see above)
How does Friedrich’s ataxia present? [2]
Same as subacute combined degeneration of the spinal cord (see above)
In addition cerebellar ataxia → other features e.g. intention tremor
Which tracts are affected in MS? [2]
Asymmetrical, varying spinal tracts involved
How does MS present? [2]
Combination of motor, sensory and ataxia symptoms
Name a condition that is just a snesory lesion? [3]
Disorder Tracts affected Clinical notes
Neurosyphilis (tabes dorsalis) 1. Dorsal columns 1. Loss of proprioception and vibration sensation
What is conveyed by the dorsal column? [3]
The sensation of fine touch, proprioception and vibration are all conveyed in the dorsal column
What is conveyed by the lateral spinothalamic tract? [2]
It is primarily responsible for transmitting pain and temperature as well as coarse touch.
What is conveyed by the lateral corticospinal tract? [2]
The primary responsibility of the lateral corticospinal tract is to control the voluntary movement of contralateral limbs
What is th efunction of the spinocerebellar tract? [2]
The spinocerebellar tracts carry unconscious proprioceptive information gleaned from muscle spindles, Golgi tendon organs, and joint capsules to the cerebellum
Asympatomic patient w/o any Sx of gour should be treated how? [1]
No Tx as not recommedned by NICE. Not proven to be beneficial.Lifestyle changes (less red meat, alcohol and sugar) can reduce uric acid levels without drug treatment and so can be advised.
What is associated with hyperuricaemia? [2]
Hyperuricaemia may be associated with hyperlipidaemia and hypertension. It may also be seen in conjunction with the metabolic syndrome
What causes increased synthesis of uric acid? [3]
Lesch-Nyhan disease
myeloproliferative disorders
diet rich in purines
exercise
psoriasis
cytotoxics
What causes decreased excretion of uric acid? [4]
drugs: low-dose aspirin, diuretics, pyrazinamide
pre-eclampsia
alcohol
renal failure
lead
What is idiopathic pulmonary fibrosis? [2]
Idiopathic pulmonary fibrosis (IPF, previously termed cryptogenic fibrosing alveolitis) is a chronic lung condition characterised by progressive fibrosis of the interstitium of the lungs. Whilst there are many causes of lung fibrosis (e.g. medications, connective tissue disease, asbestos) the term IPF is reserved when no underlying cause exists.
Whom is idiopathic pulmonary firbosis typically seen in? [1]
IPF is typically seen in patients aged 50-70 years and is twice as common in men.
Features of idiopathic pulmonary fibrosis [4]
progressive exertional dyspnoea
bibasal fine end-inspiratory crepitations on auscultation
dry cough
clubbing
Dx pulmonary fibrosis [4]
spirometry: classically a restrictive picture (FEV1 normal/decreased, FVC decreased, FEV1/FVC increased)
impaired gas exchange: reduced transfer factor (TLCO)
imaging: bilateral interstitial shadowing (typically small, irregular, peripheral opacities - ‘ground-glass’ - later progressing to ‘honeycombing’) may be seen on a chest x-ray but high-resolution CT scanning is the investigation of choice and required to make a diagnosis of IPF
ANA positive in 30%, rheumatoid factor positive in 10% but this does not necessarily mean that the fibrosis is secondary to a connective tissue disease. Titres are usually low
What is the investigation of choice and required to make a diagnosis for IPF? [2]
imaging: bilateral interstitial shadowing (typically small, irregular, peripheral opacities - ‘ground-glass’ - later progressing to ‘honeycombing’) may be seen on a chest x-ray but high-resolution CT scanning is the investigation of choice and required to make a diagnosis of IPF
Mx of IPF [3]
pulmonary rehabilitation
very few medications have been shown to give any benefit in IPF. There is some evidence that pirfenidone (an antifibrotic agent) may be useful in selected patients (see NICE guidelines)
many patients will require supplementary oxygen and eventually a lung transplant
Prognosis of IPF [1]
poor, average life expectancy is around 3-4 years
What is a restrictive lung picture in studies? [2]
classically a restrictive picture (FEV1 normal/decreased, FVC decreased, FEV1/FVC increased)
What will a CXR show in IPF [2]
A chest x-ray will show interstitial shadowing, and a high resolution CT will show ‘honeycomb’ lungs.
WHat is Lynch syndreom [HNPCC] characterised by? [1]
Lynch syndrome (HNPCC) is characterised by development of bowel cancer (among other cancers) with little formation of adenomatous polyps
How does familial adenomatous polyposis presetn? [2]
Typically over 100 colonic adenomas
Cancer risk of 100%
20% are new mutations
Hoes does MYH associated polyps present? [3]
Multiple colonic polyps
Later onset right sided cancers more common than in FAP
100% cancer risk by age 60
How does Puetz-Jeghers syndreom present? [3]
Multiple benign intestinal hamartomas
Episodic obstruction and intussusception
Increased risk of GI cancers (colorectal cancer 20%, gastric 5%)
Increased risk of breast, ovarian, cervical pancreatic and testicular cancers
How does Cowden disease develop? [3]
Macrocephaly
Multiple intestinal hamartomas
Multiple trichilemmomas
89% risk of cancer at any site
16% risk of colorectal cancer
How does HNPCC disease develop? [3]
Colo rectal cancer 30-70%
Endometrial cancer 30-70%
Gastric cancer 5-10%
Scanty colonic polyps may be present
Colonic tumours likely to be right sided and mucinous
What is sick euthyroid syndrome? [2]
In sick euthyroid syndrome (now referred to as non-thyroidal illness) it is often said that everything (TSH, thyroxine and T3) is low. In the majority of cases however the TSH level is within the >normal range (inappropriately normal given the low thyroxine and T3).
Mx of sick euthyroid syndrome [1]
In sick euthyroid syndrome (now referred to as non-thyroidal illness) it is often said that everything (TSH, thyroxine and T3) is low. In the majority of cases however the TSH level is within the >normal range (inappropriately normal given the low thyroxine and T3).
Changes are reversible upon recovery from the systemic illness and hence no treatment is usually needed.
A 22-year-old male falls of a ladder. He complains of neck pain and cannot feel his legs. His GCS suddenly deteriorates and a CT head confirms an extradural haematoma. What is the best imaging for his neck?
The correct answer is: CT c-spine40%
This man needs a CT scan of his c-spine. A CT scan will give the best resolution of any bony injury.
A 25-year-old teacher falls down the stairs. She complains of a headache and has vomited 3 times. She has a GCS of 15/15.
CT head within 1h72%
This lady has a head injury and vomiting > 1, therefore an urgent CT head is indicated.
An 18-year-old student is shot in the back of the head.
Urgent neurosurgical review (even before CT head performed)86%
A penetrating injury needs urgent neurosurgical review.
Which patients need a CT head immediately? [6]
GCS < 13 on initial assessment
GCS < 15 at 2 hours post-injury
suspected open or depressed skull fracture.
any sign of basal skull fracture (haemotympanum, ‘panda’ eyes, cerebrospinal fluid leakage from the ear or nose, Battle’s sign).
post-traumatic seizure.
focal neurological deficit.
more than 1 episode of vomiting
Which patietns need a CT head within 8h? [4]
CT head scan within 8 hours of the head injury - for adults with any of the following risk factors who have experienced some loss of consciousness or amnesia since the injury:
age 65 years or older
any history of bleeding or clotting disorders
dangerous mechanism of injury (a pedestrian or cyclist struck by a motor vehicle, an occupant ejected from a motor vehicle or a fall from a height of greater than 1 metre or 5 stairs)
more than 30 minutes’ retrograde amnesia of events immediately before the head injury
If a patient is on warfarin who have sustained a head injury with no other indications for a CT head scan, how should they be maanged? [1]
Perform CT head within 8h
How should thoracic back pain be maanged? [1]
Red flag if presneting with this, should be rederred to hospital immediately
Red flags for lower back pain [5]
age < 20 years or > 50 years
history of previous malignancy
night pain
history of trauma
systemically unwell e.g. weight loss, fever
Presentation of spinal stensosis [5]
Usually gradual onset
Unilateral or bilateral leg pain (with or without back pain), numbness, and weakness which is worse on walking. Resolves when sits down. Pain may be described as ‘aching’, ‘crawling’.
Relieved by sitting down, leaning forwards and crouching down
Clinical examination is often normal
Requires MRI to confirm diagnosis
Presentationr AS [3]
Typically a young man who presents with lower back pain and stiffness
Stiffness is usually worse in morning and improves with activity
Peripheral arthritis (25%, more common if female)
Presentation for PAD [3]
Pain on walking, relieved by rest
Absent or weak foot pulses and other signs of limb ischaemia
Past history may include smoking and other vascular diseases
Karyotype of Klinfelter’s syndrome [1]
Klinefelter’s syndrome is associated with karyotype 47, XXY
Features of Klinefelter’s syndrome [5]
often taller than average
lack of secondary sexual characteristics
small, firm testes
infertile
gynaecomastia - increased incidence of breast cancer
elevated gonadotrophin levels
Dx of Klinefelter’s syndrome [1]
Diagnosis is by chromosomal analysis
Inheritance and cause of Kallman’s syndrome [2]
Kallman’s syndrome is a recognised cause of delayed puberty secondary to hypogonadotrophic hypogonadism. It is usually inherited as an X-linked recessive trait. Kallman’s syndrome is thought to be caused by failure of GnRH-secreting neurons to migrate to the hypothalamus.
Features of Kallman’s syndrome
Features
‘delayed puberty’
hypogonadism, cryptorchidism
anosmia
sex hormone levels are low
LH, FSH levels are inappropriately low/normal
patients are typically of normal or above average height
Cleft lip/palate and visual/hearing defects are also seen in some patients
Exam question often of Kallman’s syndrome [1]
The clue given in many questions is lack of smell (anosmia) in a boy with delayed puberty
Inheritance of androgen insensitivity syndrome [1]
Androgen insensitivity syndrome is an X-linked recessive condition due to end-organ resistance to testosterone causing genotypically male children (46XY) to have a female phenotype. Complete androgen insensitivity syndrome is the new term for testicular feminisation syndrome
Features of androgen insensitvity syndrome [3]
‘primary amenorrhoea’
undescended testes causing groin swellings
breast development may occur as a result of conversion of testosterone to oestradiol
Dx of androgen insensitivty syndrome [1]
buccal smear or chromosomal analysis to reveal 46XY genotype
Mx of Androgen insensitivty syndrome [3]
counselling - raise child as female bilateral orchidectomy (increased risk of testicular cancer due to undescended testes) oestrogen therapy
What will Lh and testerone be in primary hypogonadism? [1]
Klinefelter’s syndrome
- high LH
- low testerone
What will LH and testerone be in hpyogonadotrophic hypogonadism? [1]
Kallman’s
- low LH
- low testerone
What will Lh and testerone be in androgen insensitivty syndrome [1]
AIS
- high LH
- normal/high testerone
Adverse effects of depolarising NM blocking drugs [3]
Malignant hyperthermia
Hyperkalaemia [normally transient]
May cause fasciculations
Why may succinylcholine [or suxamethonium cause fasciculations? [2]]
Binds to nicotinic acetylcholine receptors resulting in persistent depolarization of the motor end plate
CI for suxamethonium [2]
Suxamethonium is contraindicated for patients with penetrating eye injuries or acute narrow angle glaucoma, as suxamethonium increases intra-ocular pressure
Non-depolarizing NM blocking drugs MoA, examples, adverse effects and reversal of them
Competitive antagonist of nicotinic acetylcholine receptors
Tubcurarine, atracurium, vecuronium, pancuronium
Hypotension
Reversal by Acetylcholinesterase inhibitors (e.g. neostigmine)
In aortic dissection, pulse deficit may be seen when? [2]
In aortic dissection, a pulse deficit may be seen:
weak or absent carotid, brachial, or femoral pulse
variation in arm BP
Pan-systolic murmur seen when? [1]
MR
Slow rising pulse seen when? [1]
AS
Splinter haemorrhages seen when? [1]
infective endocarditis
RV heave seen when? [1]
RVH such as in cor pulmomale
PP of aortic dissection [1]
tear in the tunica intima of the wall of the aorta
Associations of aortic dissection [5]
hypertension: the most important risk factor
trauma
bicuspid aortic valve
collagens: Marfan’s syndrome, Ehlers-Danlos syndrome
Turner’s and Noonan’s syndrome
pregnancy
syphilis
Features of aortic dissection [5]
chest pain: typically severe, radiates through to the back and ‘tearing’ in nature
pulse deficit
weak or absent carotid, brachial, or femoral pulse
variation (>20 mmHg) in systolic blood pressure between the arms
aortic regurgitation
hypertension
other features may result from the involvement of specific arteries. For example coronary arteries → angina, spinal arteries → paraplegia, distal aorta → limb ischaemia
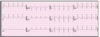
the majority of patients have no or non-specific ECG changes. In a minority of patients, ST-segment elevation may be seen in the inferior leads
Stanford classication of aortic dissection [2]
type A - ascending aorta, 2/3 of cases
type B - descending aorta, distal to left subclavian origin, 1/3 of cases
Debakey classification of aortic dissection
type I - originates in ascending aorta, propagates to at least the aortic arch and possibly beyond it distally
type II - originates in and is confined to the ascending aorta
type III - originates in descending aorta, rarely extends proximally but will extend distally
Most common trigger of anaphylaxis in children [1]
Food!
Define anaphylaxis [2]
Anaphylaxis may be defined as a severe, life-threatening, generalised or systemic hypersensitivity reaction.
Common identified triggered of anaphylaxis [3]
food (e.g. nuts) - the most common cause in children
drugs
venom (e.g. wasp sting)
How does the Resus Council IUK define anaphyaxis? [2]
The Resus Council UK define anaphylaxis as:
the sudden onset and rapid progression of symptoms
Airway and/or Breathing and/or Circulation problems
Airway problems may include:
swelling of the throat and tongue →hoarse voice and stridor
Breathing problems may include:
respiratory wheeze
dyspnoea
Circulation problems may include:
hypotension
tachycardia
What other features will around 80-90% of pts with anaphlyaxius have? [2]
generalised pruritus
widespread erythematous or urticarial rash
Recommended adrenaline dose for <6m old compared to adult? [2]
<6m then 100-150mcg
Adult then 500mcg
How often can adrenaline be repeated? [1]
Adrenaline can be repeated every 5 minutes if necessary
What is the best site for IM injection of adnrealine? [1]
The best site for IM injection is the anterolateral aspect of the middle third of the thigh.
What is refractory anaphylaxis and hwo should this be Mx? [3]
defined as respiratory and/or cardiovascular problems persist despite 2 doses of IM adrenaline
IV fluids should be given for shock
expert help should be sought for consideration of an IV adrenaline infusion
How should the patient be managed following stabilisation? [5]
non-sedating oral antihistamines, in preference to chlorphenamine, may be given following initial stabilisation especially in patients with persisting skin symptoms (urticaria and/or angioedema)
sometimes it can be difficult to establish whether a patient had a true episode of anaphylaxis. Serum tryptase levels are sometimes taken in such patients as they remain elevated for up to 12 hours following an acute episode of anaphylaxis
all patients with a new diagnosis of anaphylaxis should be referred to a specialist allergy clinic
an adrenaline injector should be givens an interim measure before the
specialist allergy assessment (unless the reaction was drug-induced)
patients should be prescribed 2 adrenaline auto-injectors
training should be provided on how to use it
What can happen in around 20% of patients with anaphlaxis? [2]
- a risk-stratified approach to discharge should be taken as biphasic reactions can occur in up to 20% of patients
How long should a patient be kept if they needed 2 doses of IM adnrealine? [1]
fast-track discharge (after 2 hours of symptom resolution):
good response to a single dose of adrenaline
complete resolution of symptoms
has been given an adrenaline auto-injector and trained how to use it
adequate supervision following discharge
minimum 6 hours after symptom resolution:
2 doses of IM adrenaline needed, or
previous biphasic reaction
minimum 12 hours after symptom resolution:
severe reaction requiring > 2 doses of IM adrenaline
patient has severe asthma
possibility of an ongoing reaction (e.g. slow-release medication)
patient presents late at night
patient in areas where access to emergency access care may be difficult
observation for at 12 hours following symptom resolution
Factors favouring pseudoseizures[5]
pelvic thrusting
family member with epilepsy
much more common in females
crying after seizure
don’t occur when alone
gradual onset
Factors favouring true epileptic seizures [2]
Ongue biting
Raised serum prolactin [why is not fully understood]