Final - Spring Flashcards
(294 cards)
neonate =
bith - 28 days
infant defined as
29 days - 1 year
general schedule for well visits
48 hrs after discharge - wt & jaundice
2 weeks
1/2/4/6/9/12 months
terminology:
preterm
late preterm
term
post-term
wt percentile: small, appropriate, large
<34
34-36
37-42
>42
<10th, 10th-90th, >90th


APGAR
A - appearance - usually lose a point for blue hands and feet
P - pulse
G- grimace
A - activity
R - respiration
done @ 1 (response for dilvery) & 5 min (response to resusc effects)

APGAR INTERPRETATION

dev milestones
domains?
set of fx skills/age-related tasks that most children do @ a certain age
- gross motor
- fine motor
- self-help/adative
- cog
- social/emo
- language
stand screedning recommended @ 9mo
___ children have dev/behav disorder
15%
early intervention
state run program that eval child for dev delays: futhur screening and potential tx
dev milestones during infancy

immunizations for neonates
most important roles of ped docs
- impt to vacc infant caregivers aga influenza and pertussis
should be reviewed @ each visit
gen starts with hep B
phys exam of neoname
exam table/open crib
- start with inspection
- heart and lung
- head –> toe: ear and hips for last (b/c more irritating)
- eye when infants eyes are spont open
older infants >6mo can be started with parent holding infant on lap/arms
temp should always be meas -_____ in children under age ____
rectal
2
normal VS for infants: temp, HR, RR, BP


periodic breathing
infants: RR may vary sig from min to min
growth meas of infant include
usually plotted on:
length
wt
head circumceference (over more prominent portion of occiput to supraorbital ridge)
**when baby is supine
plotted on WHO
- b/c breast -fed babies usually grow faster in first 6mo than formula ones and then slow down and then they both should be similar
macrocephaly usually due to
family
hydrocephalus
genetic conditions (sotos syndrome)
tumor/mass
microcephaly
genetic
intrauterine infections (TORCH, zika)
materanal smoking/drug
family
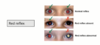
erythema toxicum
small/white papules/pustules on red base
- benign
- eosinophils
occur on day 2-3, face by 7-10

transient pustular melanosis
small pustles on HYPERPIG base:
- neutrophils
- benign
mostly in af-am infants
resolves over 1st week but hyperpig can persist for a couple of weeks

miliaria rubrum
“prinkly heat”: vesciles on red base = obstructed eccrine sweat glands
- 1st 1-2 weeks
- benign

milia
pinpoint papules on face: typ nose
- present @ birth nd fades over weeks
- keratin
- benign

how to dress infant approp?
see what you are wearing and then add 1 more layer