Final Flashcards
Review Card: Anatomy of the Kidney

Make sure to Preserve the Venous Drainage for the Left Ovarian Vein

What is the Arterial and Venous Supply of the Kidney?
Kidneys Supplied by a Single Renal Artery that Arises from the Aorta

The Renal Veins empty into the Caudal Vena Cava
Surgical Disease of the Kidney Described Below:
Calculi/Stones within the Kidney
41% of Nephroliths are Calcium Oxalate
Can Develop Uremia and Hydronephrosis
Clinical signs- Mainly Asymptomatic
Nephrolithiasis
*Calcium Oxalate- No Medical Managment
What are the Most Common Nephroliths?
Calcium Oxalate
*41% of Nephroliths are Calcium Oxalate
What Clinical Signs are Associated with Nephroliths?
Absent/Asymptomatic- Most Common
Depression, Anorexia, Hematuria, Pain
*Nephroliths are Commonly Incidental Findings
Best way to Diagnose Nephrolithiasis
Survey Radiographs
*Most Nephroliths are Radioopaque- Plain Radiographs are normally Diagnostic
*Prior to Surgery perform a Full Check of Renal Function- Excretory Urography, GFR, and Ultrasound

What Parameters do you use to Determine the Best Managment for Nephroliths?
Type of Calculi
Anatomical Location
Clinical Effects
*Ex. Struvite Calculi can be Managed Medically, while Calcium Oxalate Calculi cannot
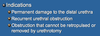
When is Surgery for Nephroliths Indicated?
Obstruction
Infection Associated with Calculi
*In Patients with Asymptomatic Nephrolithiasis, we may just Monitor Renal Function and Manage Medically

Name Two Surgical Treatment Options for Nephroliths
Nephrolithotomy
Pyelolithotomy
Surgery for Nephrolithiasis Described Below:
Ventral Midline Celiotomy
Retract Mesocolon/Mesoduodenum
Isolate Kidney and Vessels
Rumel Tourniquet or Bulldog Vascular Clamp on Isolated Vessels to Temporarily Occlude Venous Supply
Make Sagittal Incision and** **Remove the Stone
Culture Renal Pelvis, Flush Renal Pelvis and Ureter with Heparinized Saline
Catheterize Ureter to Ensure Patency and Submit Stones for Analysis

Nephrolithotomy
*Cutting into the Kidney, Opening it and removing the Stones

What Instruments can be used to Occlude the Renal Vessels during Nephrolithotomy
Rumel Tourniquet
Bulldog Vascular Clamp

How do you Close the Surgical Site following Nephrolithotomy
Sutureless Closure- Hold for 5 Minutes, Forms Fibrin Seal, Suture Capsule Only with Simple Continuous Pattern
or
Horizontal Mattress Pattern- Through Capsule and Cortex of Kidney

How Long can you Occlude the Renal Vessels for during Nephrolithotomy?
20 Minutes
*Vascular Clamp Time is 20 minutes! No longer than 20 Minutes or else you will develop Damage to the Kidney
Surgery for Nephrolithiasis Described Below:

Can be used to Remove Calculi when Proximal Ureter and Renal Pelvis are Dilated
Pyelolithotomy
*Making an Incision into the Renal Pelvis to Remove a Stone
*Have to have Swelling/Dilation for you to have Access to Renal Pelvis

What are Advantages of a Pyelolithotomy over a Nephrolithotomy?
Pyelolithotomy- Does NOT Require Occlusion of Blood Supply and does NOT Damage Nephrons
*Better to use Pyelolithotomy when Stones are Located in Renal Pelvic Area because it has Advantages over Nephrolithotomy

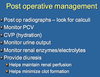
What is Post Operative Managment of a Nephrolithotomy
Post op Radiographs- Look for Calculi
Monitor Urine Output, Renal Enzymes/Electrolytes
Provide Diuresis- Helps Maintain Renal Perfusion, Helps Minimize Clot Formation
How can you Diagnose Renal Trauma?
Contrast Excretory Urography
Ultrasound

How do you Treat Minor, Moderate, and Severe Renal Trauma?
Minor Trauma (Ex. Bruising)- Conservative Treatment
Moderate Trauma (Ex. Capsular Tears, Bleeding)- Surgical Intervention by Suturing Tears, Hemostatic Agents (Gelfoam), Omentalization (Omental Patching)
Major Trauma (Shattered Cortex and Capsule)- Nephrectomy or Nephroureterectomy

What are the Indications for Performing a Nephroureterectomy
Severe Infection (Ex. Pyelonephritis)
Severe Trauma
Obstructive Calculi with Persistent Hydronephrosis
Neoplasia
Transplant
*Nephroureterectomy- Removal of the Kidney and Ureter

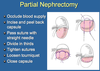
What are the Indications for a Partial Nephrectomy
Trauma/Focal Hemorrhage/ Neoplasia in a Patient with CONTRALATERAL Renal Compromise and we want to preserve as much Renal Tissue as Possible
Compromised GFR in Other Kidney

What are the Disadvantages of Performing a Partial Nephrectomy over a Nephrouretectomy?
Partial Nephrectomy- Higher Incidence of Post Operative Hemorrhage
*Risk of Hemorrhage is MUCH high than Performing a Total Nephrectomy
Progressive Dilation of the Renal Pelvis and Atrophy of the Renal Parenchyma
Hydronephrosis
Clinical Signs of which Kidney Disease:

Hydronephrosis
*Kidney will Feel like a Tumor Mass- Palpable Mass
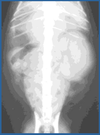
How do we Diagnose Hydronephrosis?
Abdominal Radiographs
Ultrasound
Excreatory Urogram
Treatment for Hydronephrosis
Releave Primary Cause/Obstruction < 1 week: Complete Resolution
Releave Primary Cause/Obstruction > 4 Week Duration: May Retain 25%
Severe Parenchymal Damage (> 4 Week Duration): Nephroureterectomy
*If its Caught early (< 1 Week) and you are able to Releave the Primary Obstruction, Often the Kidneys will regain full Function

Treatment for Pyelonephritis
Severe/Non Responsive Cases- Nephrouretectomy
*Typically if we can Treat Pylonephritis Medically or Surgically we will go ahead and do that. Ex. If caused by Obstructive Uropathy (Nephrolithiasis) you will remove the Stone
How is Giant Kidney Worm (Dioctophyma Renale) often Diagnosed?

Urinalysis- Eggs in Urine (If Caught Early)
Necropsy- Often Diagnosed on Necropsy
*Once the worm matures it Migrates through the Kidney thus causing Significant Damage of the Cortex and the Medulla. These worms tend to Proliferate and cause damage very Quickly

Treatment for Giant Kidney Worm (Dioctophyma Renale)
Nephrectomy- Removal of Affected Kidney
Nephrotomy- Manually Remove the Worms
*If Unilateral then remove the one Kidney. If its causing Significant Damage to the Kidney, its best to Remove the Entire Kidney (Nephrectomy)
Most Common Benign and Malignant Kidney Tumors in the Dog and Cat
Benign- Renal Adenoma (Both Dogs and Cats)
Malignant in Dogs- Renal Cell Carcinoma
Malignant in Cats- Lymphosarcoma
*Most Renal Neoplasia is Aggressive Metastatic Types of Tumors
Most Common Renal Neoplasia in the Canine
Renal Cell Carcinoma
*Mean Survival Time 6-8 Months
How to Manage Renal Cell Carcinoma in Canine
Nephroureterectomy and Chemotherapy
*Remove the Kidney and use Chemotherapeutic Protocols
Best way to Diagnose Renal Cell Carcinoma
Renal Biopsy
Most Common Renal Neoplasia in the Feline
Renal Lymphoma (Lymphosarcoma)
Treatment for Renal Lymphoma in Felines
Chemotherapy
*Renal Lymphoma- Not Surgically Treated
Renal Neoplasia Described Below:
Congenital Neoplasia
Part of the Developing Kidney
More Common in YOUNG Dogs and Cats (< 1 Year)
Mean Survival Time- 6 Months

Embryonic Nephroblastoma
*YOUNG Dogs and Cats
How do Nephroblastoma’s Develop?
Embryogenesis
Treatment Indicated for Embryonic Nephroblastoma
Nephroureterectomy and Chemotherapy
*However, these tumors are NOT very Amenable to Treatment
Clinical Signs of ______:

Renal Neosplasia
*Commonly able to Palpate a Large Mass in the Paralumbar Area
How do you Diagnose Renal Neoplasia?
Abdominal Radiographs- Can be Very Diagnostic for Renal Neoplasia
Abdominal Ultrasound- Even MORE Diagnostic for Renal Neoplasia (Confirms Kidney Mass in 85% of Patients)
*Very Rare that you have to do more advanced Diagnostics than Radiograph or Ultrasound to Diagnose Renal Neoplasia

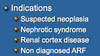
What Parameters are used to Determine if a Renal Biopsy is Indicated?
Suspected Neoplasia
Nephrotic Syndrome
Renal Cortex DIsease
Non Diagnosed Acute Renal Failure (ARF)
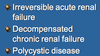
Contraindications of Performing a Renal Biopsy
Coagulopathies
Hypertension
Severe Chronic Hydronephrosis
*ALWAYS collect Coagulation Profiles on Patients prior to Renal Biopsy. If the patient is not clotting Properly the Renal Biopsy could be Disasterous

Kidney Biopsy Technique Described Below:
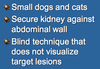
Percutaneous
*Best for Skinny/Small Dogs and Cats
Kidney Biopsy Technique Described Below:

Ultrasound Guided (_P_referred Method)
Kidney Biopsy Technique Described Below:

Keyhole
Kidney Biopsy Technique Described Below:

Wedge/Incisional Biopsy
*Surgical Method of Obtaining a Biopsy- Need to Occlude Vasculature
*Taking a Larger/Very Good Diagnostic Sample
Common Complications/Risks of Performing Renal Biopsy
Severe Hemorrhage (IMPORTANT)
Hematuria- Resolves in 2-3 days
Hydronephrosis
*Hemorrhage is a HUGE possible Complication- Make sure Patients haven’t recently been treated with blood thinners or NSAIDs

Indications for ______ in Felines:
Renal Transplant
*Mainly used in Chronic Renal Failure Cats or Patients with Acute Irreversible Renal Failure associated with a Toxin
Contraindications to Renal Transplants
Viral Positive (FELV, FIV)
Cardiac Disease
Neoplasia
Fractious
Special Considerations taken for Renal Transplants
Cost (Extremely Expensive)
Frequent Visits
Immunosuppression Therapy- LIFELONG

Prognosis for Renal Transplant in Felines
25% of Patients do NOT survive to Discharge (Don’t Leave Hospital)
Mean Survival Time- 613 Days
Breed, Sex and Clinical Signs of which Surgical Disease of the Ureter:
Breed Predisposition: Siberian Husky
Young Female Canines
Clinical Signs:
Incontinence
Fails to House Train
UTI/Urine Scalding
Ectopic Ureter
*Ectopic Ureter: Failure of One or Both Ureters to Terminate in the Normal Location

How do you Diagnose Ectopic Ureter?
Excretory Urography (Fluoroscopy)
CT
Ultrasound
Cystoscopy
*We use a Combination of Diagnostics to Confirm the Presence and Location of Ectopic Ureters

Two Different Classification of Ectopic Ureters. Which Classification is the Most Common?
Extramural: Ureter Enters into Neck, Urethra or Vagina
Intramural: Ureter Enters Normally but Exits Abnormally (MOST COMMON)

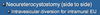
Treatment for Ectopic Ureter
Neoureterocystostomy
*Two Types: Side to Side, End to Side
Neoureterocystostomy Technique for Treatment of Ectopic Ureter Described Below:

Side To Side
*Best to Remove Remnant Ureter that may Contribute to Incontinence
Prognosis Following Treatment for Ectopic Ureter
90% Improvement when add Medications Following Neoureterocystostomy

What are the Two Types of Ureteroceles
Intravesicular (Normal)
Ectopic (Neck/Urethra)
*Ureterocele- Dilation of Distal Ureter due to Persistent Membrane over the Ureteral Oriface where it empties into the Bladder. Persistent Membrane can create Hydroureter or Obstruction

Clinical Signs of Ureterocele
UTI / Incontinence
Azotemia (If Obstruction)
*High Incidence of Urinary Tract Infections with Ureteroceles
How do you Diagnose Ureterocele?
IV Urography
*Contrast media will outine the Persistent Membrane- Cobra Head Sign

Treatment for Ureterocele
Intravesicular: Uretercelectomy
Ectopic: Neoureterocystostomy with Ureterocelectomy
What are the Causes of Ureteral Trauma
Iatrogenic (#1 Cause)
*Most Common Cause- During an Ovariohysterectomy where the Surgeon accidently Clamps Down/Ligates the Ureter

How do you Diagnose Ureteral Trauma?
Uroretroperitoneum or Uroabdomen
Radiographs
IV Urography- Localize Lesion
*Obviously if there is Urine Leakage into the Abdominal Cavity, there must be a Leaking area at the Level of the Crush Site
What are the Four Treatment Options for Ureteral Trauma?
Nephroureterectomy- Removal of Ureter and Kidney
Ureteroureterostomy- Ureteral Anastomosis
Neoureterocystostomy- Replant Ureter in Different Location in the Bladder
Urinary Diversion- Divert Urine from going across the Surgical Site to allow better chance of healing
*Urinary Diversion is usually done in Conjunction with one of the Other Surgical Procedures
Surgical Procedure used to Treat Ureteral Trauma Described Below:
Disadvantages- Extermely Difficult with High Incidence of Complications

Ureteroureterostomy (Ureteral Anastomosis)
*Disadvantages: Very Difficult with High Incidence of Complication
Surgical Procedure used to Treat Ureteral Trauma Described Below:
Catheterize Through Cystotomy
Avoids Engaging Back wall with the Suture
Suture under Magnification

Ureteroureterostomy
What Two Methods are Available for Urinary Diversion After Ureteral Surgery
Ureteral Stent
Nephrostomy Tube
Method Available for Urinary Diversion After Ureteral Surgery Described Below:

Ureteral Stent
*Urinary Diversion is Provided after every Surgical Procedure used to Correct Ureteral Trauma in order to Prevent Urine Flow through the Surgical Site
Allows Urinary Diversion to allow the Anastomosis Site to Heal following Ureteroureterostomy (Ureter Anastomosis)
Method Available for Urinary Diversion After Ureteral Surgery Described Below:

Nephrostomy Tube
*Suture Kidney to the Body Wall and then Feed the Tube Out of the Body wall to Create a Urinary Diversion without any urine going through the Anastamosis Site

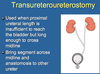
What Procedures can be used if you have Loss of Length of the Distal or Proximal Ureter
Transureteroureterostomy- Used When Proximal Ureteral Length is Insufficient to Reach the Bladder. Bring Segment across Midline and Anastomosis to Other Ureter
Renal Descensus- Mobilize Kidney and Suture Caudally to Lumbar Musculature
Nephrocystopexy- Suturing the Kidney to the Cranial Edge of the Bladder
Psoas Hitch- Fixes the Bladder in a More Cranial Position
Surgical Procedure used when Proximal Ureteral Length is Insufficient to Reach the Bladder but Long enough to Cross Midline
Transureteroureterostomy

Surgical Procedure used when there is Significant loss of Distal Ureter
Bladder Wall Flap
*Lengthening Bladder Tissue so that it can reach the Ureter

Most Common Indication for Ureteral Surgery
Ureterolithiasis
*Stones within Ureter- Primarily Calcium Oxalate
What are the Clinical Signs of Ureterolithiasis
Asymptomatic (Most Common)
UTI, Hematuria
Anorexia, Lethargy, Pain
*If the Stones are not causing a significant Obstruction Process the patients are commonly Asymptomatic
How do you Diagnose Ureterolithiasis
Plain Radiographs
*Most are Radiopaque Calcium Oxalate
Since Most Ureterolithiasis cases are ______, Medical Dissolution is NOT an Option
Calcium Oxalate
*Can only Treat Struvites via Medical Dissolution
Presurgical Considerations for _______:
Cannot Predict how Long Ureter Obstructed: 1 Week Obstruction GFR < 65% (Cannot Predict how Well Kidney will Recover)
Most Cats have Preexisting Interstitial Nephritis unrelated to Obstruction
If Azotemic with Unilateral Obstruction = Bilateral Renal Disease
High Complication Rate with Surgery
Ureterolithiasis
Treatment Options for Ureterolithiasis
Cystotomy and Retrograde Flushing and Removal via Pyelithotomy (Ideal Procedure)
Ureterotomy- Difficult with High Incidence of Leakage/Dehisence
*If you have a Stone in the Ureter it would be IDEAL to do a Cystotomy Incision, Place a Catheter into the Ureteral Orifice and try to Push the Stone into the Renal Pelvis- Flush Saline and Dislodge the Stone
Advantages and Disadvantages of Permanent Ureteral______:
Advantages:
Decreased Morbidity
Shorter Hospitilization
Less Complications
Disadvantages:
Specialized Equipment
Steep Learning Curve
Permanent Ureteral Stenting
*Due to the High Complication Rate with Ureteral Surgery, Ureteral Stenting is becoming more Common
*Rather than Remove the Actual Stone or Obstruction, you Bypass the Ureteral Obstruction with Permanent Ureteral Stent- Leads to Less Complications
Indications for Ureteral Stenting- Stone, Tumor, Stricture, Blood Clot

Method of Permanent Ureteral Stenting Described Below:

Place Guide Wire into Ureteral Orifice
Place Catheter over Guide Wire and Inject Contrast Media in order to Visualize Renal Pelvis
Remove Ureteral Catheter and feed Stent over the Guide Wire and Place the Stent into the Renal Pelvis
Endoscopic Placement
Method of Permanent Ureteral Stenting Described Below:
Perform Cystotomy Incision and Place Catheter into Renal Pelvis using Fluoroscopy
Guide Stent into Renal Pelvis

Surgical Stenting
Method of Permanent Ureteral Stenting Described Below:

Placing one End of Catheter into Kidney (Renal Pelvis)
Kidney Catheter is Placed onto Shunting Port
A Seperate Catheter is Placed into the Bladder
The Opposite End of the Bladder Catheter is Attached to the Shunting Port
SUB (Subcutaneous Ureteral Bypass)
*Feed Renal Catheter and Bladder Catheter through the Abdominal Wall and connect both of them to the Shunting Port. Secure the Port to the Abdominal Wall

Review Card: Anatomy of the Bladder
Trigone- Region Between Urethral and Ureteral Openings
Nerve Supply: Hypogastric Nerve (Sympathetic) and Pelvic Nerve (Parasymphathetic)
Blood Supply: Caudal Vesicular (Primary), Prostatic/Vaginal Artery

Types of ______ Abnormalities:
Persistant Urachus
Vesicouracheal Diverticulum
Urachal Cyst (Rare)
Urachal Sinus (Rare)
Urachal
*Urachal- Embryonic Conduit Providing Communication between Bladder and Allantoic Sac that Atrophies at Birth
Persistant Urachus- Persistance of a Tube between the Bladder and Umbilicus
Urachal Abnormality Described Below:
Persistance of a Tube between the Bladder and Umbilicus
Clinical Signs:
Urine Dribbling From Umbilicus
Omphalitis (Inflammation of Umbilicus)
Ventral Abdominal Dermatitis
UTI

Persistant Urachus
How do you Diagnose Persistant Urachus
Place Contrast In Umbilicus and Take Radiograph
*You will see Contrast Travel from Umbilicus up into the Bladder
How do you Treat Persistent Urachus
Surgical Removal of Urachal Tube
Most COMMON Urachal Abnormality
Vesicouracheal Diverticulum
Urachal Abnormality Described Below:
Most Common Urachal Abnormality in Canine Patients
External Opening at the level of the Umbilicus is Closed while the Internal Opening is Open
Patients with Recurrent Urinary Tract Infections
Vesicouracheal Diverticulum
How do you Diagnose Vesicouracheal Diverticulum
Positive Contrast Cystography

Treatment for Vesicouracheal Diverticulum
Partial Cystectomy and Diverticulectomy
*Remove that section of the Bladder Wall and suture it back together
What are the Causes of Bladder Rupture
Mainly Trauma (HBC)
Severe Cystitis
Neoplasia
Urethral Obstruction
Iatrogenic- Ex. Catheterization, Cystocentesis
True/False: In Any Case of Abdominal Trauma, consider Bladder Rupture until you can Rule it out
True
*Palpable Bladder and Normal Urination does NOT rule out Bladder Rupture

How do you Diagnose Bladder Rupture
Positive Contrast Urethrocystogram (Most Reliable)- Leakage of Contrast Material into Abdomen
Abdominocentesis (Confirm Diagnosis)- Urine in Abdominal Cavity
Plain Radiographs: Obscured Serosal Detail, Free Abdominal Fluid, Absence of Bladder
Ultrasound: Helps Determine Source of Injury and Visualize Defects in Bladder Wall

When Performing an Abdominocentesis to Confirm Bladder Rupture, What do you expect to find with Regards to Creatinine and Urea Levels
Creatinine in Peritoneal Fluid > Serum Creatinine
Urea in Peritoneal Fluid = Serum Urea
*Once Creatinine in Abdominal Fluid is Higher than Serum Creatinine you have confirmed the presence of Urine in the Abdominal Cavity

How do you Treat Bladder Rupture
Surgical Repair Immediately if Stable- Debride Tear and Necrotic Tissue and Close Bladder Wall
Omentalize or Serosal Patching- Better Seal Bladder Defect
*Make sure to Explore the Entire Abdominal Cavity
*If Patient is Unstable, then Stabilize First with Fluids and Abdominocentesis (Decompress Abdominal Cavity)
What are the Indications for Tube Cystotomy
Any Need for Urinary Diversion- Bladder or Urethral Surgery/Trauma, Neurological Bladders
*Often Times we Divert urine with a Tube Cystostomy- Do this Procedure to help Keep the Bladder Decompressed
How to Perform a ______:
Ventral Midline Incision
Purse String Suture in Bladder
Make Stab Incision in Bladder and place 6-16 fr Foley or Mushroom Tip Catheter
Create Hole in Abdominal Wall and feed Catheter through Hole
Perform Cystopexy- Hold Bladder in place
Attach Collection Bag to End of Catheter to Monitor Urine

Tube Cystostomy
Potential Complications for Performing a ______:

Tube Cystostomy
*Patient always has to have an E Collar on whenever you place these Tubes otherwise they will Grab the Tubes and pull them out
Indications for Performing a Cystopexy
Tube Cystostomy
Perineal Hernia
Urinary Incontinence associated with Pelvic Bladder
Cystopexy- Surgical attachment of the urinary bladder to the abdominal wall or to other supporting structures
In Patients with Perineal Hernias- the Bladder is one of the Structures that tends to Herniate. Cystopexy helps to prevent the Bladder from Herniating
How to Perform a ______:
Cranial Traction of Urinary Bladder
Suture Bladder Wall to Abdominal Wall
Two Lines of Suture

Cystopexy
Most Common Types of Cystic Calculi (Stones in the Bladder)
Struvite
Calcium Oxalate
*Struvite and Calcium Oxalate account for over 90% of Cystic Calculi
Clinical Signs associated with ______:
Hematuria, Straining and Discomfort
Palpation of Large Thickened Bladder
Sometimes Palpate Large Calculi
Urinary Tract Infection (76%)
Cystic Calculi
How do you Diagnose Cystic Calculi
Plain Radiographs- May see Radiopaque Stones within Bladder (Struvite, Calcium Oxalate). If Stones are Radiolucent (Cystine and Urates) then more Diagnostics are Required
Double Contrast Cystography or Ultrasound- Equally Effective for Detecting Radiolucent Stones within the Bladder (95% Effective)

What are the Non-Surgical Treatment Options for Cystic Calculi
Voiding Hydropropulsion
Transurethral Cystoscopy
Dietary Modification
Electrohydraulic Lithotripsy
Non-Surgical Treatment Option for Cystic Calculi Described Below:
Must be Very Small Calculi (Smaller than Urethral Diameter)
Place Patient under Anesthesia
Inject Saline into the Bladder- Distend Bladder
Hold Upright
Express Bladder
Re-Radiograph

Voiding Hydropropulsion
Non-Surgical Treatment Option for Cystic Calculi Described Below:
Use of Cystoscope to Remove Small Stones
Stones must be Smaller than the Diameter of the Urethra
Grab Stones and Manually Remove them out of the Bladder
Transurethral Cystoscopy
Non-Surgical Treatment Option for Cystic Calculi Described Below:
ONLY works for Struvite Stones
Cannot be Obstructed
Dietary Modification
*Alter the Diet to help Dissolve the Stones
*Diet Modification DOES NOT work on Calcium Oxalate Stones
Non-Surgical Treatment Option for Cystic Calculi Described Below:
Passage of a Cystoscope
Electrode Wire and Spark Generator to Break apart Stone
Electrohydraulic Lithotripsy
When is Surgery Indicated for Cystic Calculi
Urinary Tract Obstruction
No Medical Options
Other Retrieval Methods Failed

Most Common Surgical Procedure used to Remove Cystic Calculi
Cystotomy
Surgical Procedure for Cystic Calculi Described below:
Caudal Ventral Midline Approach
Moistened Lap Sponges
Empty Bladder (Compression/Small Needle and Syringe)
Place Stay Suture in Lateral Aspect and Apex of Bladder
Make Stab Incision at Apex of Bladder and Extend Incision with Scissors
Evert Bladder Walls to Allow Full Inspection
Remove Calculi with Instrument
Pass Urethra Catheter and Flush to Ensure Patency

Ventral Cystotomy
*Ventral Cystotomy Approach is Preferred over Doral Approach
*Submit Urine, Stones, and Mucosal Tissue for Culture

What is the Layer of Strengh when Closing a Cystotomy Incision
Submucosa
*Layer of Strength of the Bladder
Following a Cystotomy, the Bladder Requires a Water Tight Closure.
What are the Common Suture Patterns used to Close the Bladder?
One or Two Layer Inverting Pattern- Cushing Followed by Lembert
Simple Continuous in the Submucosa followed by Cushing Pattern
*Inverting Pattern will Create Fibrin Seal and assist us with Water Tight Closure- Serosa to Serosa Contact Encourages Fibrin Seal

Following Cystotomy, after closing the Bladder, make sure to perform a ______
Leak Test
*Compress Neck of Bladder and Inject Saline and look for any leakage at the incision site
What is Polypoid Cystitis

Benign Polyps that Develop within the Mucosa of the Bladder
*Rare Condition that Mimics a Neoplastic Condition
When the Polyps rupture the Patients will have Bloody Urine
How do you Diagnose Polypoid Cystitis
Biopsy
*Biopsy confirms Polypoid Cystitis
Treatment for Polypoid Cystitis
Surgery- Resect Affected Tissue
*Usually Curative after you Resect the Polyps since it is a Benign Condition
Most Common Bladder Tumor in the Dog
Transitional Cell Carcinoma (TCC)
*97% Malignant and has an affinity for the TRIGONE area

Most Common Bladder Tumor in the Cat
Transitional Cell Carcinoma
*Most Common Bladder Tumor in Cats, and the Second most Common Urinary Tract Tumor in Cats
Most Common Urinary Tract Tumor in Cats
Renal Lymphoma
How does Transitional Cell Carcioma (TCC) differ in the Dog and Cat?
Most common Older FEMALE Dogs
Most Common in Middle Aged MALE Cats
Dogs: Affinity for TRIGONE area of Bladder
Cat: Affinity for APEX of Bladder
*Felines- More Ammenable for Surgery because the TCC is in the Apex of the Bladder
Canine- Less Amenable for Surgery because the TCC is found within the Trigone Area
KNOW THESE DIFFERENCES- On Exam

Predisposing Factors for ______ in the Bladder:
Obesity
Insecticide Exposure
Herbicide Exposure
Cyclophosphamide (Anti-Cancer Drug)
Transitional Cell Carcinoma (TCC)
*Carcinogen Exposure- Insecticides and Herbicides. Patients that have been exposed to Insecticides and Herbicides have shown an Increased Incidence of the Development of TCC
Breed Predisposition for Transitional Cell Carcinoma
Older Scottish Terriers
Physical Exam Findings in Patients with ______:
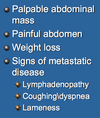
Transitional Cell Carcinoma
*Often we can Palpate a Large Mass in the Caudal Abdomen in the Area of the Bladder
*Since there is such High Metastatic Potential you are going to look for Metastatic Disease- Ex. Lymphadenopathy
How do you Diagnose Transitional Cell Carcinoma?
Cystoscopy (Very Diagnostic)- Can Visualize and Biopsy Mass
Ultrasound (Very Diagnostic)- Determines Degree of Bladder Invasiveness, Evaluate Abdomen for Metastatic Disease and LN Involvment
Bladder Tumor Antigen Test (BTAT)- High Risk of False Positives
*30% of Urine Cytology will pick up TCC

Name the Advantages and Disadvantages of the Bladder Tumor Antigen Test (BTAT) used to diagnose Transitional Cell Carcinoma
Advantage- Best used as Routine Screening Test for Older Patients
Disadvantage- High Incidence of FALSE POSITIVES
*Very Poor in Differentiating Patients with Lower Urinary Tract Disease versus Transitional Cell Carcinoma (False Positives)
Treatment for Transitional Cell Carcinoma (TCC) of the Bladder
Combination Protocol- Chemotherapy and Partial Cystectomy
*Chemotherapy and Partial Cystectomy on their Own did not Increase the Mean Survival Time of the Patient. Only in Combination do they Increase the Survival Time
Urethral Condition Described Below:
Most Common Developmental Abnormality of Male Genitalia
Incomplete Formation of Penile Urethra
Urethral Orifice can occur anywhere along Penis

Hypospadias
Treatment for Hypospadias
If Asymptomatic- Leave it alone
If Clinical Signs- Reconstruction Procedure
*Most of the Time these patients are Asymptomatic and we just leave it alone. Only Perform Surgery if the Patient is developing Urine Scolding and other Clinical Signs
Protrusion to Urethral Mucosa through Orifice
Urethral Prolapse
*Associated with some form of Straining
Clinical Signs associated with which Urethral Disorder:
Bleeding from Prepuce
Licking
Red-Purple Mass

Urethral Prolapse
Urethral Prolapse is most Common in Young Male _____ Dogs
Brachycephalic
*Most Urethral Prolapses occur in Brachycephalic Breeds that Strain while Breathing, which leads to the Prolapse
Treatment for Urethral Prolapse in Asymptomatic Patients
Reduce with Aid of Large Catheter
Place Purse String Suture- Leave for 5 Days
*Tie Purse String to help Prevent it from Prolapsing again
Two Adjunctive Treatments done in Patients with Urethral Prolapse
Surgical Correction of Airways
Castration
*Brachycephalics are more Prone to Urethral Prolapse due to Straining while Breathing. If the Airways are corrected, so that they are not straining to breathe so much then Prolpase will not recur
Treatment for Urethral Prolapse in Symptomatic Patients

Urethropexy- If Tissue is Viable
Resection and Anastomosis- Tissue is NOT Viable

What Suture Material is best for Urethral Surgery
Monofilament Absorbable (PDS)
*AVOID Braided Absorbable (Vicryl)

What Causes Urethral Obstruction in Dogs and Cats
Mucus Plugs
Crystals or Stones
Neoplasia
Strictures
*Most common cause of Urethral Obstruction in male Dogs is Calculi

Where is Urethral Obstruction Most Common in Male Dogs and Cats?
Male Dogs: Ischial Arch or Caudal to Os Penis
Male Cats: Distal 1/3 of Urethra

How do you Diagnose Urethral Obstruction
Contrast Urethrography
Plain Radiographs- Radiopaque Calculi, Large Distended Bladder

In Patients with Urethral Obstruction, you want to administer _____ right away in order to Decrease the Urea/BUN Concentrations
Fluids
*Fluids will help to Improve Metabolic Acidosis

Three Methods used to Temporarily Relieve Urethral Obstruction in a Dog or Cat due to Calculi
Catheter
Hydropropulsion
Cystocentesis
*Initially try to Relieve the Obstruction Non-Surgically
Non-Surgical Method used in CANINE Patients to Temporarily Relieve Urethral Obstruction due to Calculi:

Retrograde Hydropropulsion
*Place Catheter as far up the Urethra as possible and attempt to Inject Saline under pressure in order to distend the Urethra in an attempt to Flush the stone back into the Bladder- Much easier to do Surgery on the Bladder rather than the Urethra
Surgical Technique to Relieve Urethral Obstruction due to Calculi if Hydropropulsion was NOT Successful
Urethrotomy
*If Hydropropulsion was Successful the Calculi would be in the Bladder and we would Perform a Cystotomy
If Hydropropulsion was NOT Successful then we must perform a Urethrotomy- Cutting into the Urethra and Removing the Stone at the Location where the Obstruction has occured
Indications- Calculi that cannot be Hydropropulsed
Where would you Perform a Urethrotomy in Canine Patients

Prescrotal
*Very Superficial Area with Less Cavernous Tissue

Surgical Technique to Relieve Urethral Obstruction due to Calculi Described Below:
Place Urethral Catheter
Ventral Midline Incision between Base of Scrotum and Caudal Penis
Retract Retractor Penis Muscle
Incise Urethra and Remove Calculi
Flush Urethra
Prescrotal Urethrotomy
*Most Common Surgical Technique used in Canine Patients
Two Available Methods for Closure Following Prescrotal Urethrotomy
4\0 Monofilament Absorbable- Suture Urethra Closed
Second Intention (Preferred)- Advantage: Less Risk of Stricture, Disadvantage: Profuse Hemorrhage

Why is Perineal Urethrotomy a Less Preferred Surgical Method to Relieve Urethral Obstruction?

Increased Risk of Infection
Difficult Procedure

Surgical Formation of a Permanent Opening of the Urethra at a New Site
Urethrostomy
Preferred Locations for Urethrostomy in Dogs and Cats
Canine- Scrotal
Feline- Perineal
*Canine- Scrotal Urethrostomy is Preferred because it is More Superficial, Less Hemorrhage, and Less Urine Scold

In a Scrotal Urethrostomy, which Structures should be Draped in your Surgical Field?
Abdomen
Scrotum
Prepuce
In a Scrotal Urethrostomy, How Long should the Urethral Incision be?

2.5-4cm Long

In a Scrotal Urethrostomy, What is the Most appropriate Suturing Method?

4\0 Absorbable/Non-Absorbable Monofilament
Take Bites at Edge of Cavernous Tissue- Avoid Cavernous
*AVOID Cavernous Tissue- Only Engage Urethral Mucosa and Skin

Complications of a Scrotal Urethrostomy
Hemorrhage
Dehiscence
Urine Scald
Stricture
UTI
What is the Disadvantage of a Canine Prescrotal Urethrostomy
Higher Incidence of Urine Scald

When is a Perineal Urethrostomy in a Cat Indicated?
Frequent Obstruction
Strictures
Trauma
*Perineal Urethrostomy- Commonly done Procedure in Feline Patients. Usually performed in Cats where Medical Treatment for Recurrent Obstructions (Mucous Plugs or Crystals) isn’t Working
*After Multiple Attempts of Medically Preventing Recurrence of Urethral Obstruction, we end up doing this Salvage Procedure of removing part of the Proximal Urethra

What are the Goals of Perineal Urethrostomy in Cats?
Mobilization of Urethra
Creation of Wide Urethral Orifice

What Gland/Area of the Urethra do you dissect to when Performing a Perineal Urethrostomy in a Cat
Bulbourethral Gland/Pelvic Urethra
*Dissect to the Level of the Bulbourethral Gland- Anatomical Landmark to know you are within the Pelvic Urethra

When Performing Perineal Urethrostomy, how can you check if the Urethral Orifice is Wide Enough?
Mosquito Hemostat to Hinge
*To Ensure that you have a Wide enough Opening, take a pair of Mosquito Hemostats and place it into the Urethra and it should and it should reach all the way up to the Hinge Section of the Hemostat
Complications of a Perineal Urethrostomy in a Cat
Hemorrhage (Common)
Urinary Tract Infection (Common)
Stricture
Subcutaneous Urine Leakage: Improper Suturing
*Complication Rate- 25%

Creation of a Urethrostomy on the Ventral Body Wall Cranial to the Pubis

Antepubic Urethrostomy
Indications for which Type of Urethrostomy Procedure:
Recurrent Pelvic Urethral Obstruction
Failed Perineal Urethrostomy that cannot be Revised
Antepubic Urethrostomy

Complications associated with Antepubic Urethrostomy
Urine Scalding- Big Problem
UTI
Incontinence
Clinical Signs of Urethral ______:

Trauma
*Most of the TIme with Urethral Trauma the patient will show Straining with Hematuria
*There may be Leakage into Adjacent Subcutaneous Tissue- Urine accumulating and Causing Necrosis of that Tissue
How do you Diagnose Urethral Trauma
Positive Contrast Urethrogram

Treatment for Urethral Trauma
Incomplete or Small Laceration- Heal with Urinary Diversion and Urethral Catheter (Conservative Managment)
Complete Laceration- Anastomosis or Repair with Urinary Diversion
What are the Causes of Urethral Strictures

Patients with Urethral Strictures won’t show Clinical Signs until _____% of the Urethra is Narrowed
60%

How do you Diagnose Urethral Strictures?
Cystoscopy- See Stricture within Urethra
Urethrogram
Treatment for Urethral Strictures
Urethral Dilators
Balloon Dilation
Resection and Anastomosis (Severe Strictures)

Review Card: Dental Terminology


Very Important Anatomic Landmark shown by the Red Line

Mucogingival Line
*Junction between the Gingiva (Soft Tissue of the Oral Cavity that supports the Teeth) and the Oral Mucosa
Review Card: Dental Anatomy


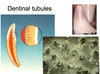
The Dentin of the Tooth is the Dense Body-Like Matrix layer beneath the Enamel and the Cementum. It is a _____ Layer sensitive to Heat or Cold because the Dentinal Tubules allow Indirect Access to the Nerves in the Pulp Chamber
Porous

Review Card: Radiographic Anatomy of Tooth
Portion of the Pulp that is BELOW the Crown = Root Canal
Portion of the Pulp that is ABOVE the Crown = Pulp Chamber

Only Visible Part of the Periodontium in a Normal Mouth
Gingiva

Potential Space Between Tooth and Gingiva
Gingival Sulcus

Collagenous Connective Tissue Structure Extending from Cementum to Periosteum of the Tooth
Periodontal Ligament

Functions of the _______:
Attaches Teeth to the Alveolus
Absorbs Shock from the Impact of Occlusal Forces and Transmits them to Alveolar Bone
Supplies Nutrients to Alveolar Bone and Cementum via Arterioles
Isolates the Tooth from the Surrounding Bone and, IMPORTANTLY, the Osteoclasts that Remodel the Surrounding Bone
Periodontal Ligament
If the ______ Ossifies, due to Trauma or Excess Vit. D, then Osteoclasts can invade the Tooth and Remodel it into Brittle Bone Rather than a Flexible Tooth full of Dentinal Tubules. This Causes the Roots to Essentially Disappear and the Crown to Break off since the Tooth Doesn’t Flex when it chews on something solid
Periodontal Ligament
*Vitamin D is Toxic to the Periodontal Ligament Fibers
True/False: This is a Mass/Tumor in the Oral Cavity

False
*This is Incisive Papilla- Overlies the Vomeronasal Organ

Perminant Bud Arises from the Deciduous Bud in Utero. Therefore if there is No _____ Tooth, there will be NO Corresponding Permanent Tooth
Deciduous Tooth

Part of the Tooth that is < 0.1 mm to 0.6 mm Thick and that is NOT Replaced if Damaged
Enamel

Part of the Tooth that Consists of Blood Vessels, Nerves and Connective Tissue

Pulp
*As the Animal Ages the Pulp Chamber becomes Progressively Smaller

Normal ______ Process:
As the Root Lengthens, the Deciduous Tooth will Erupt. Soon after the Tooth is Fully Erupted the Root will Begin to Undergo Resorption. At the Same time the Permanent Tooth Bud starts its development and Erupts as the Deciduous Tooth is Shed
Eruption

Review Card: Anatomical Numbering System
Place the Number of the Tooth on the Corresponding Side of the Letter
As a Superscript if in the Maxilla and a Subscript if in the Mandible
_If Deciduous Teeth use Small Case Lette_rs
Ex. Maxillary Canine of Right (C1)
Ex. Second and Third Premolar on Left (<span>2,3</span>P)

Incisor = I
Canine = C
Premolar = P
Molars = M

Review Card: Triadan System
First Number = Quadrant the Tooth is In
Second and Third Number = Number of the Tooth Itself
Canine Incisor is ALWAYS 04
First Molar is ALWAYS 09
KNOW THE RULE OF 4 AND 9

Examples:
Right Maxillary Middle Incisor = 102
Left Maxillary Canine = 204
Left Mandibular 4th Premolar = 308
Right Mandibular 1st Molar = 409

Dental Disorder Described Below:
Caused by Failure of the Primary Tooth’s Root to undergo Resorption
Cause Displacement of Permanent Teeth that can lead to Orthodontic Problems or Soft Tissue Trauma
Canine Teeth and Incisors Most Commonly

Retained Decidious Teeth

Two Clinical Problems that Arise from Retained Decidious Teeth
Malocclusions
Periodontal Disease
With Retained Decidious Teeth, Permanent Teeth usually Erupt Lingual to the Decidious Teeth. The Primary Exception is the Maxillary Canine which Erupts _____ to Its Deciduous Counterpart
Mesial (Rostral)

Most Common Malocclusion caused by Retained Decidious Teeth:
Mandibular Adult Canines Erupt LINGUAL to Decidious Canines
Base Narrow Canines
*Canines have come in Too Far Lingually and they are Impacting on the Soft Tissue entrapped there
Treatment for Retained Decidous Teeth
Extract Decidious Teeth that are Retained

Dental Disorder Described Below:

“Extra Teeth” most commonly seen in Premolar Area
Can Interfere with Normal Occlusions, Cause Overcrowding, Malposition, Malocclusion or Incomplete Eruption of Adjacent Teeth
Supernumerary Teeth (Polyodontia)
Dental Disorder Described Below:
Missing Teeth
Genetic Defect (Never Developed)
Premolars are Most Commonly Affected
Predisposed Breeds- Mexican Hairless and Chinese Crested Dogs

Adontonia/Hypodontia (Missing Teeth)
*Rule of Thumb- If Deciduous Tooth is Congenitally Absent, the Adult Tooth will also be missing

Normal Occlusion Described Below:

Scissor Bite

Class of Malocclusion Described Below:
Malpositioned Teeth
Jaw Length Normal
Class 1
*Some Teeth are within an Improper Position

Class of Malocclusion Described Below:
Mandibular Brachygnathisim
Upper Jaw is Longer than the Lower Jaw (Parrot Mouth)
Class 2
*Mandible is too short- Mandibular Brachygnathism

Class of Malocclusion Described Below:
Mandibular Prognathism
Mandible is Longer than the Maxilla (Underbite)
Class 3
*Ex. Bulldogs

Class 1 Malocclusion Described Below:
Teeth are Misaligned due to too many Teeth (Supernumerary Teeth) or the Jaw is too small for the Normal Number of Teeth
Crowding
*Not enough room for all the teeth to fit in the normal alignment
Most Common Class 1 Malocclusion:

Mandibular Adult Canines Erupt LINGUAL to Decidous Canines
Base Narrow Canines
Class 1 Malocclusion Described Below:
One or More Maxillary Incisors are Displaced Towards the Palate

Anterior Cross Bite
*The Maxillary Incisors should be Rostral to the Mandibular Incisors
Class 1 Malocclusion Described Below:
Maxillary Premolars are Lingual to Mandibular Premolars

Posterior Cross Bite
Class 3 Malocclusion Described Below:
Incisor Crowns Meet Instead of the Mandibular Incisors being Directly Behind the Maxillary Incisors
Considered Prognathism
Leads to Abnormal Wear on Incisors- Attrition

Level Bite
Malocclusion Described Below:

Elongation of One Half of the Hed so there is Unequal Arch Development
Midline of the Mandible and Maxilla do NOT Line Up
Wry Mouth

Treatment for Malocclusions Described Below:
Certain Teeth Extracted or have their Crown Height Reduced to Prevent Trauma to other Teeth or Soft Tissue Structures in the Mouth

Interceptive Orthodontics
Treatment for Base Narrow Canine Malocclusion:

Acrylic Material Placed Inside the Maxilla
Incline Planes

Impacted Teeth can result in _____ Formation and Should be Extracted in most Cases

Dentigerous Cyst

Dental Disease Described Below:

Damage to Ameloblasts during Enamal Development or Exposure of Enamel to Corrosive Material
Enamel Wears Down Over Time
Enamel Hypocalcification/Hypoplasia
*Overtime the Enamel is worn down and the teeth assume and Irregular Knob Shape with Dentin that stains Brown

Distemer Virus Infection or other Diseases that cause High Fever during Permanent Tooth Development can cause Generalized or Focal Defects in _____
Enamel

Treatment for Enamel Hypocalcification/Hypoplasia
Focal: Restore Defect with Composite
Cap Important Teeth to Prevent Wear

In Tibetan Terriers, ______ occurs in addition to Generalized Enamel Defects
Root Abnormalities

Dental Disease Described Below:
Drug that if Given to Pregnant Bitches and Given to Young Pups when Adult Teeth are Developting will lead to Yellow-Stained Teeth
Dentin is the Affected Layer

Tetracycline Staining
*No Treatment

Dental Disease Described Below:

Pathologic Wearing due to Contact with Opposing Tooth (Malocclusion)
Attrition

Treatment for Attrition
Orthodontic Correction
Crown Reduction
Extraction
Dental Disease Described Below:
Abnormal Contact with Crown Surface by Foreign Object (Ex. Tennis Balls, Cages)

Abrasion

Dental Disease Described Below:
Etiology- Bacteria Produce Organic Acids that, when in the Presence of Carbs, Decalcify Enamel and Dentin
Uncommon due to Scissor Bite, Pointed Crowns, and Diet
Appearance- Brownish Color, Leathery Consistency

Dental Caries (Cavities)
Treatment for Dental Caries (Cavities)
Indirect or Direct Pulp Capping
Root Canal
Extraction (Most Common)
*Normally Dental Caries are Severe by the Time they are Reconized. Therefore Most Commonly the Tooth ends up being Extracted

Dental Disease Described Below:

Infection that Can Result in Endodontic or Periodontic Lesions
Periapical Infection
*Classic Presentation- Draining Tract at the Medial Apect of the Eye

Draining Tract Associated with The Teeth is called a ______

Parulis
*If the Parulis is at the Mucogingival Line- Most Likely to be Caused by Endodontic Disease
Dental Disease Described Below:
Etiology: Focal Hyperplastic Gingiva in Periodontal Disease
Predisposed Breeds: Boxers
Can occur with Administration of Drugs- Cyclosporine, Calcium Channel Blockers

Gingival Hyperplasia
Treatment for Gingival Hyperplasia
Gingivectomy/Gingivoplasty
Post Op Care- Twice Daily Rinses with 0.2% Chlorhexidine Solution
*Treatment- Remove Excessive Tissue to Return Sulcus Depth to Normal. Try to Recreate Normal Scalloped Contour

Dental Disease Described Below:
Trauma to the Pulp
Discoloration of the Tooth- Purple/Grey
May be Reversible- But NOT Often (< 10%)
The Older the Patient the Less Likelihood the Pulp will Survive

Pulpitis
*Trauma to the Pulp has caused Bleeding. Blood Perculates out into the Dentinal Tubules leading to Purple Color of Tooth
*The Younger the Animal, the Greater the Likelyhood the Pulp will Survive
Treatment for Pulpitis
Monitor- If Tooth is Still Alive
Root Canal or Extraction- If Tooth is Dead
*Pink Tooth = Still Alive
Grey Tooth = Dead
Radiographic Findings in a Tooth with Pulpitis
Decreased Wall Size
Lucency around Apex
Apex Resorption

Tooth Fracture Classification Described Below:

Microfractures in Enamel caused by Heavy Chewing
Staining of Teeth Often Occurs in Lines
NO Loss of Structure
Enamel Infraction (Abraction)

Tooth Fracture Classification Described Below:

Tooth Fracture where the Pulp Chamber is NOT Exposed
Uncomplicated Crown Fracture
Tooth Fracture Classification Described Below:

Crown Fracture where Pulp is Exposed
Complicated Crown Fracture
Chewing on Hard Objects such as Nylabone can cause Shearing Forces of the Crown known as ______ that Extend into the Surface of the Root

Slab Fractures
*Slab of the Tooth is Fractured off- Most Common in Maxillary 4th Premolar
Treatment for Uncomplicated Crown and Enamel Fractures
Indirect Pulp Capping
Crown Restoration

Treatment for Complicated Fractures

Vital Pulpotomy
Root Canal
Extract Tooth
*If there is Minimal Periodontal Involvement, the Tooth can be Saved by Performing a Vital Pulpotomy or Root Canal and Placing the Dog on Antibiotics
*Root Canal- Take out all the Contents of the Tooth
Diagnosis and Treatment of Disease that Affect the Tooth Pulp and Apical Periodontal Tissues
Endodontics

Indications for _____:

Endotontics

Endodontic Procedure Described Below:
Maintains a Viable Tooth that will Continue to Mature
Performed after Acute Pulp Exposure due to due to Trauma
Patients < 18 Months Old (Immature Tooth)
80% Initial Success when Performed < 48 Hours after Pulp Exposure
Vital Pulpotomy
*Removal of the Corroded Portion of the Pulp

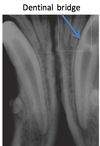
Endodontic Procedure Described Below:
Remove the Exposed and Contaminated Pulp from Crown with Dental Bur
Gently Flush the Access Site with Sterile Saline
Apply ProRoot MTA (Mineral Trioxide Aggregate) to Stimulate Dentinal Bridge Formation
Place Intermediate and Surface Restoration
Re-Radiograph at 3, 6, and 12 Months Post Op

Vital Pulpotomy

Endodontic Procedure Described Below:
Goal is to Remove ALL the Pulp Contents, Disinfect the Pulp Cavity, Create a Seal at the Apex to Trap Remaining Bacteria in the Tooth
Mature Tooth (> 24 Months)
Maintains Tooth Function but Tooth is “Dead”
Root Canal
Endodontic Procedure Described Below:
Access Pulp Cavity and Remove Dead or Infected Pulp
Clean and Shape the Canal with Endodontic Files
Flush Canal with Sodium Hypochlorite while Cleaning and Shaping
Obturate (Fill) the Canal: Seal Apex and Fill the Rest of Canal with Gutta Percha
Radiograph to Confirm Complete Obturation
Restore the Surface of the Crown at Fracture

Root Canal

Dislocation of a Tooth out of its Alveolus WITHOUT being Totally Avulsed from the Mouth
Luxation
The Total Separation of a Tooth from its Alveolus
Avulsion

For Luxated/Avlused Tooth:
Re-Implantation should occur within 30 Minutes of Avulsion. While Awaiting Aplantation the Tooth Should be Kept in a Mixture of Saliva and _____
Milk
*After 30 Minutes Success goes down Exponentially

Treatement for Tooth Luxation/Avulsion
Re-Seat in Alveolus and then Splint in Place (4 weeks)
Perform Root Canal when Splint is Removed if Tooth is Reattached
*Replace the Avlused Tooth into the Socket and then Place Acrylic Splint. A Root Canal is Performed Later when Reattachment of the Tooth is Verified
Dental Disease Described Below:
Most Common Disease of Tooth Structure in Domestic Felines
Osteoclast Resorption is the Predominant Activity
Tooth Resorption
Type of Tooth Resorption Described Below:

Type 1

Type of Tooth Resorption Described Below:

Type 2

Type of Tooth Resorption Described Below:

Type 3

Clinical Signs in Cats with ______:
Very Localized Hyperplastic/Hyperemic Gingiva
Pain- Dropping Food, “Chattering”, Anorexia, Reluctance to have Mouth Examined
Tooth Resorption
Treatment for Tooth Resorption
Type 1: Entire Tooth should be Extracted
Type 2: Extract Entire Tooth if Root Structure/Pulp Chamber are Intact. If Not Intact, Amputate Crown and Superficial Root and Leave Ankylosed Part of the Root since its being Reabsorbed anyway
Type 3: Combination of Above

Dental Disease Described Below:
Etiology: Unknown but Possibly due to Calicivirus
Chronic Non-Responsive Inflammatory Oral Disease Characterized by a Distinct Infiltrate of Plasma Cells and Lymphocytes
Clinical Signs: Ptyalism, Dysphagia, Anorexia, Severe Marginal Gingivitis

Feline Gingivostomatitis
Treatment for Feline Gingivostomatitis
Teeth Extraction- All Caudal Teeth or All Teeth (Most Effective)
Prophylaxis/Home Care

Dental Disease Described Below:
Noted in Cats < 9 Months of Age
Clinical Signs:
Abundant Plaque and Calculus that Results in Gingivitis, Bone Loss, Gingival Resorption and Pocket Formation

Juvenile-Onset Periodontitis
Treatment for Juvenile-Onset Periodontitis
Frequent Prophylaxis and Aggressive Homecare- May “Outgrow”

Extractions
Dental Disease Described Below:
Severe Inflammation of the Paradental Tissue (Kissing Lesions)
Clinical Signs:
SEVERE Halitosis (Bad Breath)
Thick, Cloudy Saliva
Oral Pain and Difficulty Eating

Canine Ulcerative Paradental Stomatitis (CUPS)
Treatment for Canine Ulcerative Paradental Stomatitis (CUPS)
Home Care: 1-2x’s Daily Brushing
Total Mouth Extractions

Study and Treatment of Diseases affecting the Supporting Structures of the Tooth

Periodontics

Dental Disease Described Below:
Most common Oral Disease
> 70-85% of Dogs and Cats
#1 Cause of Tooth Loss
More Common due to: Diet, Malocclusion
Periodontal Disease
Diseases that Exacerbate Periodontal Disease:
Neutrophil Dysfunction
Diabetes Mellitus
Autoimmune Disease
Hyperadrenocorticism
Feline Viral Disease- Especially _______
Calicivirus
*Calicivirus in Cats can cause Issues within the Oral Cavity
Three Etiologies of Periodontal Disease
Acquired Pellicle (Biofilm)- Thin Layer of Salivary Proteins that Form on Surface of Tooth and serves as Site for Bacterial Attachment
Plaque- Combinatinon of Bacteria, Food, Debris, and Oral Epithelial Cells
Calculus- Mineralized Plaque Containing Bacteria which Release Endotoxins that Cause Gingivitis

Loosely Adhered ______ Plaque causes an Inflammatory Response which Results in Destruction of the Junctional Epithelium and Epithelial Attachment exposing the Periodontium. This in turn creates a Periodontal Pocket which allows apical migration of the Bacteria and Further Loss of the Periodontal Ligament and Alveolar Bone
Subgingival Plaque
Pathophysiology of ______:

Gingival Recession
Destruction of Periodontal Ligament
Bone Loss
Mobility
Periodontal Disease
*Mobility of the Tooth caused by Destruction of Periodontal Ligament
Clinical Signs of _______:

Periodontal Disease
*Accumulation of a Lot of Debris on the Surface of the Tooth
Stage of Periodontal Disease Shown Below:
Gingival Tissue is Firm and Pink or Pigmented
Defined Stipling
Free Gingival has Knife-Like Edge
Minimal Sulcus Depth: 1-3mm in Dog, 0-1mm in Cats

Stage Zero (Normal)

Stage of Periodontal Disease Shown Below:
Erythema
Gums Bleed When Probed
Loss of Stipling
Normal Sulcus Depth
Reversible- With Proper Treatment

Stage 1 (Gingivitis)

Stage of Periodontal Disease Shown Below:
Gums Bleed when Probed
Minor Pockets
Minimal Bone Loss
Usually NO Mobility
Periodontitis can be Controlled but NOT Completely Reversed

Stage II (Early Periodontitis)
*CANNOT be Reversed, Only Controlled

Stage of Periodontal Disease Shown Below:

Stage III (Moderate Periodontitis)
*Up to about 50% Bone Loss
Stage of Periodontal Disease Shown Below:

Stage IV (Advanced Periodontitis)
* > 50% Bone Loss, Advanced Bone Mobility
# 1 Preventative Method for Periodontal Disease
Mechanical Abrasion
*Good Home Care
Treatment of Periodontal Disease
Home Care- Start Daily Tooth Brushing
Thorough Dental Cleaning
Dental Diets/Dental Hygeine Chews- Help Prevent Accumulation of Plaque and Tartar
Antibiotics- Clindamycin
True/False: Antibiotics can cure Periodontal Disease
False
*Antibiotics DO NOT cure Periodontal Disease

Dental Instrument Desribed Below:
Pointed Tip, Two Cutting Surfaces
Work Away from Sulcus
NEVER use Sharp Tip below the Gingival Margin

Scaler
*ONLY used Supragingivally- Above the Gum Line
Dental Instrument Desribed Below:
Rounded Tip and Back with Flat Face
Used for Supra-or Subgingival Calculus Removal and Root Cleaning

Curette
Dental Instrument Desribed Below:
Probe used to Measure Sulcus Depth

Periodontal Probe

Dental Instrument Desribed Below:

Considered to be the Best Scaler in Vet Met
Creates Best Motion for Cleaning
iM3 42-12

Review Card: Complete Dental Cleaning
1. Disinfect the Oral Cavity- Power Spray the Mouth with Chlorohexidine
2. Examine the Oral Cavity- Visual Inspection using Magnification. Look and Feel Under Tongue
3. Gross Calculus Removal- Hand Scaling
4. Subgingival Calculus Removal- CRITICAL STEP
5. Missed Calculus Detection- Air from 3 Way Syringe- You can see Inside Pockets this way. Residual Calculus will Appear Chalky White
6. Polish- ESSENTIAL STEP
7. Sulcus Irrigation- Flush Polish out of the Sulcus
8. Diagnostics- Periodontal Probing (Measure Sulcus Depth), Charting, Dental Radiographs

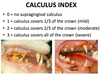
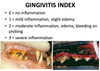
Review Card: Calculus Index and Gingitivits Index
True/False: Some Degree of Tooth Mobility is Normal and is Referred to as Physiologic Mobility and Represents the movement of a tooth within the Periodontal Ligament Space
True
*Movement in Excess of Physiologic Mobility is Referred to as Pathologic Mobility
Grade that Represents Severe Mobility of a Tooth
3

When Performing a Complete Dental Cleaning, _____ are Essential to Identify “Hidden” Lesions and Develop a Treatment Plan
Dental Radiographs

Diagnosis based on this Radiograph

Periodontal Disease

List the Pathologies seen in this Radiograph


Diagnosis based on this Radiograph

Periodontal Disease

Diagnosis based on this Radiograph

Periodontal Disease

Diagnosis based on this Radiograph

Feline Buccal Bone Expansion

The Branch of Denstistry that Deals with Tooth Extraction
Exodontics
Indications for ______:

Exodontics (Tooth Extraction)

Diagnosis based on this Pre-Extraction Radiograph

Dilaceration (Curved Root Tip)


