Filtration Flashcards
(30 cards)
What is filtration?
1.Filtration: the formation at the glomerular capillaries of an essentially protein-free filtrate of plasma, (~20%)

What is average GFR?
180 litres per day
- Allows regulation of ECF volume and control of blood composition (eliminating nasty substances)
What is reabsorption?
Reabsorption: Substances that the body wants are reabsorbed, those it doesn’t want stay in the tubule and are excreted.

What is secretion?

Secretion: Substances may be specifically removed from the body in this way.
Some drugs are eliminated this way
Proton excretion is important in the regulation of acid base balance
How much blood flow does the kidney receive?
Kidneys receive a blood flow of » 1200mls/min, ie 20-25% of total cardiac output
Remarkable since the kidneys weigh less than 1% of the body weight
How long would it take for the entire blood volume to pass through the kidney?
less than 5 mins
Are red blood cells and blood plasma filtered into the bowmans capsule?
None of the red cells and only a fraction of the plasma is filtered through into Bowman’s capsule.
The remainder passes via the efferent arterioles into the peritubular capillaries and then to the renal vein.
How much of renal plasma becomes glomerular filtrate?
Plasma constitutes » 55% of total BV.
55% of 1200mls/min = 660mls/min = renal plasma flow
GFR is normally 125mls/min
Therefore the filtration fraction = 125/660 x100 = 19% ie 19% of the renal plasma becomes glomerular filtrate.
What forces govern filtration?
Glomerular Filtration occurs in exactly the same way as fluid filters out of any capillary in the body.
It is dependent on the balance between the hydrostatic forces favouring filtration and the oncotic pressure forces favouring reabsorption. (Starling’s forces).
What determines the filterability of solutes across te glomerular filtration barrier?
Molecular size
Electrical charge
Shape

Describe the structure of the glomerular endothelial cell
Fenestrated - prevents filtration of blood cells but allows all components of blood plasma to pass through
Describe the function of the basal lamina of the glomerulus
Prevents the filtration of larger proteins
Descrbe the function of the slit membrane between the pedicels
Prevents filtration of medium sized proteins

Why is the glomerular capillary pressure high?
Because the afferent arteriole is short and wide and offers little resistance to flow. So the blood arriving at the glomerulus still has a high hydrostatic pressure.
In addition, the unique arrangement of the efferent arteriole which is long and narrow offers a high post-capillary resistance.
Golden rule of the circulation:
If you have a high resistance, hydrostatic pressure upstream is increased, while the pressure downstream is decreased.
Describe the difference in pressure between hydrostatic pressure and the oncotic pressure in the glomerular capillaries
At the glomerular capillaries the hydrostatic P favouring filtration always exceeds the oncotic P.

How do we calculate net filtration pressure?
Hydrostatic pressure minus the colloid osmotic pressure plus the fluid pressure creasted by fluid in the bowmans capsule

What is the number 1 factor affecting GFR?
In normal physiology, 1° factor is PGC and this is dependent on the afferent and efferent arteriolar diameter and therefore the balance of resistance between them.
What extrinsically controles the GFR?
a) Sympathetic VC nerves - afferent and efferent constriction, greater sensitivity of afferent arteriole.
b) Circulating catecholamines - constriction 1°ily afferent
c) Angiotensin II - constriction, of efferent at [low], both afferent and efferent at [high].
What is the affect of increasing the resistance of the afferent and efferent arteriole?

What does the renal vasculature adjust its resistance in relation to?
Blood pressure
This keeps BF and GFR essentially constant = autoregulation.
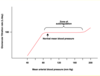
What is the effect on GFR of an increasing blood pressure and a decreasing blood pressure outwith the normal ranges?
Below 60mmHg, filtration falls and ceases altogether when MBP = 50mmHg.
If mean arterial P increases , there is an automatic increase in afferent arteriolar constriction, preventing a rise in glomerular PGC . Dilatation occurs if P falls.
What is autoregulation dependant on?
Autoregulation is independent of nerves or hormones, occurs in denervated and in isolated perfused kidneys.
What is the autoregulatory range?
In man autoregulatory range is 60-130mmHg,
What is the response in the kidneys if there is a haemorrhage?
In situations where blood volume/BP face serious compromise, eg in haemorrhage, activation of sympathetic VC nerves and AII, can override autoregulation liberating blood for more immediately important organs.
As much as 800mls of blood per minute can thus be provided to perfuse these other organs at the expense of the kidney.



