Female Pelvic Viscera Flashcards
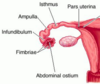
Label all:


Adnexa of uterus =
- ovary + uterine tube
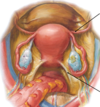
Label all:


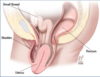
Label:

bladder
Location of uterus in relation to the bladder in females:
- uterus lays on top of urinary bladder.
- urge to urinate is entirely pressure driven.
- increased urge to urinate during pregnancy due to inreased uterine weight on the bladder.
Vestibule of vagina:
- area between labia minora.
- urethra and vaginal canal open into vestibule.
Path of vagina to abdominal cavity:
cause of pelvic inflammatory disease
- opening of vagina
- up vagina
- into cervix
- into uterus
- through and out fallopian tubes
Vagina blood supply:
- pelvic portion: vaginal artery; branch of uterine artery/internal iliac.
- perineal portion: internal pudendal artery.
Nervous innervation to pelvic vagina:
- Autonomics: uterovaginal plexus
- Pain: pelvic splanchnic nerves (parasympathetic; S2-S4 lower limb pain)
Uterovaginal plexus is a sub-plexus of:
inferior hypogastric plexus

Nervous innervation to perineal vagina:
Pudendal nerve (motor and sensory)
Vaginal fornices:
- recesses created by cervix entering vagina.
- exploited for examination and surgical access.

The anterior fornix can be used to palpate:
bladder
The lateral fornices can be used to palpate:
ovaries, oviduct, ureters
The posterior fornix can be used to palpate:
uterus, rectum, rectouterine pouch (pouch of Douglas)
Through what vaginal pouch can you enter the rectouterine pouch (pouch of Douglas), and therefore the abdominal/pelvic cavity?
posterior fornix
Label all:


Label all:

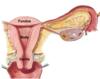
The two openings of the cervix:
- internal os = between cervix and uterus.
- external os = between cervix and vagina.
What is the normal anatomical position of the uterus:
anteverted and anteflexed.
- anteverted = angle cervix enters vagina.
- anteflexed = angle between cervix and uterus body.

Anteflexion of uterus:
- angle between cervix and uterus body.
- uterus tipped forward as it rests on the urinary bladder.

Anteversion of uterus:
- angle cervix enters vagina.
- protects/covers external os of cervix.