Eye Complaints Flashcards
Objectives
cornea
- Clear part of the eye
- Avascular

Meibomian Glands
- Secrete oil
- Keeps tears from evaporating quickly

Circulation of Aqueous Humor
ciliary body–> posterior chamber–> through pupil–> anterior chamber–> canal of schlemm–> circulation
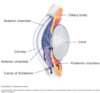
Internal Eye Anatomy

General Considerations for eye complaints
- The eye stops growing by age three
- The eye moves thru 100° of motion
- The cornea is avascular
- The lens continues to add volume throughout life, doubling its volume by age 70
- The ciliary body produces fluid for the anterior chamber and its muscles accommodate the lens. This fluid must be continually exchanged.
- The retina converts light energy into electrical energy
PANCE Eye Disorders
- Conjunctival Disorders
- Corneal Disorders
- Lacrimal Disorders
- Lid Disorders
- Neuro-Ophthalmologic Disorders
- Orbital Disorders
- Retinal Disorders
- Traumatic Disorders
- Vascular Disorders
- Vision Abnormalities
Conjunctivitis
- Diffuse dilatation of conjunctival vessels with redness extending to the periphery
- Watery, mucoid, mucopurulent watery discharge can be noted
- Etiology can be bacterial, viral, allergic, or environmental irritation
- Possibly highly contagious

Cataracts
- Opacity of lens
- Degenerative eye disease
- Gradual onset
- Yellowing of lens
- “Mistiness” of vision
- Like looking through a dirty window
- Occurs w/aging or UV light
- Most common cause of blindness

Corneal Abrasion
- Corneal abrasions are commonly seen when foreign material comes in contact with the anterior eye. Prolonged wearing of contact lenses can also lead to corneal abrasions.
- Careful visualization of the eye along with fluorescence stain and the use of a Wood’s Lamp will elicited most superficial abrasions.

Corneal Ulcer
- A single open sore of the cornea
- Caused by bacterial, viral, or fungal infections, physical or chemical trauma, prolonged wear of contact lenses, corneal drying (Bell’s Palsy)

Corneal Ulceration
- Example of herpes infection after staining of the eye

Keratitis
- Inflammation of the cornea
- Caused by bacterial, viral, fungal, or parasitic infections, minor trauma or injury, excessive contact lens wear

Pterygium
- A triangular, pinkish, tissue growing from the canthus toward the pupil
- Will cross over the corneal margin
- Unknown etiology (Surfer’s eye)
- Once large enough, the patient’s vision will be effected
- Treated with surgical excision
** A Pinguecula does not cross the corneal margin
Dacryocystitis
- An infection of the lacrimal sac, secondary to obstruction of the nasolacrimial duct at the junction of the lacrimal sac
- Causes pain, redness, excessive tearing, and swelling over the inner aspect of the lower eyelid

Blepharitis
- Inflammation of the eyelids; usually seen at the area where the eyelashes grow
- Crusting is typically noted with redness and swelling
- Commonly caused by clogged Meibomian gland pores
- Treated with anti-inflammatory and antibiotic medications, warm compresses

Hordeolum (Sty)
- A painful local infection of the glands of Zeis (external hordeolum) or meibomian gland (internal hordeolum); usually of Staph origin
- Usually localizes to the lid margin and therefore can be treated by removing a single eyelash
- Warm compresses, antibiotics, possible I&D are treatments

Chalazion
- Redness and swelling of the eyelid away from the eyelash margin
- Usually not painful
- Usually caused by a clogged oil gland
- Usually does not make the entire eyelid swell
- Treated with warm compresses, sometimes antibiotics/cortisone; possible I&D

Ectropion
- Chronic condition where the eyelid turns out; usually the lower lid; seen in older patients
- With the condition, the eyelid dries out and becomes irritated
- Treated with artificial tears and lubricating ointments; surgery maybe required
- Secondary causes: age/muscle weakness, facial paralysis (Bell’s palsy, tumors), previous scaring or surgery, eyelid growths, genetic disorders (Down Syndrome)

Entropion
- Chronic condition where the eyelid turns inward so that the eyelashes contact the conjunctiva
- Usually seen in older patients; lower eyelid only
- Treated with artificial tears and lubricating ointments; surgery maybe required
- Similar causes to ectropion but may also be due to a trachoma infection or congenital conditions

Nystagmus
- Repetitive, uncontrolled movements of the eye (rhythmic beating)
- Types
- Congenital
- Spontaneous
- Acquired persistent spontaneous
- Gaze-evoked nystagmus
- Rebound nystagmus
- Positional nystagmus
Congenital Nystagmus
- usually has a high frequency, usually horizontal; a lifelong history without other symptoms makes the diagnosis
- More frequent than acquired
- Accompanies other disorders
- micro-ophthalmic anomalies
- Down syndrome
- Is usually mild and non-progressive
- Affected persons not normally aware of spontaneous eye movements
- Vision impairment depends on severity of movements
Spontaneous Nystagmus
- results from a peripheral vestibular lesion in the labyrinth or vestibular nerve (CN 8), usually horizontal and torsional
Acquired persistent spontaneous Nystagmus
- results from a lesion in the brain stem or cerebellum, usually vertical, horizontal or torsional
Gaze-evoked nystagmus
- usually results from drugs, i.e., phenobarbital, phenytoin, alcohol and diazepam; is always in the direction of the gaze and may present with and without fixation
Rebound nystagmus
- a type of gaze evoked nystagmus that either reverses or reverses direction as the eccentric gaze position is held; result of cerebellar atrophy or lesions of the cerebellum
Positional nystagmus
- turning the head causing the nystagmus) usually results from otolith debris in the semicircular canals, i.e., vertical torsional for the vertical canals and horizontal torsional for the horizontal canal
Physiologic Nystagmus
- Direction of nystagmus is defined by the direction of its quick phase
- a right-beating nystagmus is characterized by a rightward-moving quick phase
- Oscillations may be vertical, horizontal or torsional or any combination
- 2-3 beats of nystagmus is considered normal
- Nystagmus is often named as a gross description of the movement
- Downbeat, upbeat, or lateral nystagmus
Dz(s) that can cause Pathological Nystagmus
- Benign Paroxysmal Positional Vertigo
- Cerebral vascular accident
- Meniere’s disease
- Multiple sclerosis
- Brain tumors
- Wernicke-Korsakoff Syndrome (encephalopathy)
- Lateral medullary syndrome
- Aniridia (absence of the iris)
- Optic nerve hypoplasia
- Albinism (absence of skin pigmentation)
- Horner’s syndrome
Toxic or Metabolic Causes of Nystagmus
- Alcoholic intoxication
- Lithium
- Barbiturates
- Phenytoin (Dilantin)
- Salicylates
- Benzodiazepines
- LSD or PCP
- Ketamine
- Certain anticonvulsants or sedatives
- Methamphetamine
- Thiamine deficiency
CNS Disorders associated with Nystagmus
- Cerebellum disorders such as:
- CVA
- Thalamic hemorrhage
- Tumor
- Trauma
- Multiple sclerosis
- Cerebellar ataxia
- Purely vertical nystagmus (usually central origin)
Optic Neuritis
- Inflammation of the optic nerve where eye pain and temporary vision loss is noted (usually in one eye)
- Patient can also suffer loss of color vision, visual fields, see flashing lights
- Changes can become permanent
- Can be due to multiple sclerosis or unknown causes
- Treatment with steroids
Papilledema
- A condition where pressure in or around the brain causes swelling of the optic nerve and the nerve is pushed into the center of the eye
- May be caused by brain tumor, abscess/infection, head injury, bleeding in the brain, intracranial hypertension, inflammation of the brain or tissue coverings, uncontrolled hypertension
- May present with vision changes, headache, nausea, vomiting, but not eye pain

Orbital Cellulitis

- A major infection of the anterior tissues of the face and orbits
- Staph or Strep bacterium are the usual principal etiologic agents
- Commonly noted to be a spread of an acute sinusitis
- Presents with periorbital redness and swelling, the eye is painful to touch (11% of patients suffer loss of vision)
- Suspicion of diagnosis is confirmed by CT
- Ophthalmologic Emergency—Patient admission is recommended, ophthalmologic consultation, and treatment with IV antibiotics

Macular Degeneration
- One of four major causes of vision loss in the U.S.
- 2.44 million cases 2010, affecting 2.5% of whites 50yrs and older vs. 0.9% of other races
- Rates sharply rise after age 80 with whites 13.8% and 11% overall rate
- Effects the central vision, usually begins with dry/nonexudative degeneration which can progress to wet/exudative/neovascular degeneration
- May present with drusen bodies (yellow deposits under the retina made up of lipids)
- Vitamin supplements and intraocular injections with vascular endothelial growth factor inhibitors are used to slow the progression of the disease
- Neither treatment prevents the degeneration

Retinal Detachment
- Sudden loss of vision, ↓ or cloudy vision; PAINLESS, preceded by flashing lights and floaters
- “Curtain” over visual field
- Floating folds observed
- Separation of retina from its blood supply
- ↑ risk in patients with ↑ age, myopia & post-op ocular surgery
- Can occur with blunt trauma to the eye/head
- Immediate referral for laser or cryotherapy

Retinopathy
- Disease of the retinal layer of the eye; usually thought of either being due to uncontrolled hypertension or diabetes
- Either condition can lead to visual changes and possible loss of vision
- Both conditions cause changes to the circulation of the retina and can be visualized by fundoscopic examination
- Cotton wool spots, copper/silver wire changes, flame hemorrhages, neovascular changes, etc.
Orbital Blowout Fracture
- Facial blunt trauma can cause fractures in the floor or wall of the ocular orbit which can permit the ocular globe of “fall” into the defect.
- Patients present with a history of facial trauma, bruising, swelling, redness, and pain around the face. Diplopia, facial numbness, and epistaxis are also frequently noted.
- A hallmark of the condition is asymmetric extraocular movement or entrapment of the eye with a “frozen” gaze.
Globe Rupture
- Rupture of the eyeball occurs with either blunt but more commonly penetrating trauma. Any full-thickness injury to the cornea or sclera is considered an open globe.
- Globe rupture is an ophthalmologic emergency and is associated with a high frequency of visual loss.
Hyphema
- A collection of blood in the anterior chamber of the eye (between the iris and cornea—not to be confused with a subconjunctival hemorrhage)
- Hyphema is usually secondary to trauma and is therefore painful
- Ophthalmology consult is most often required

Retinal Vascular Occlusion
- Two main types
- retinal artery occlusion
- retinal vein occlusion
- Retinal arterial occlusion is the more critical/time sensitive to diagnose, an Ocular Emergency
- Patients typically in their 60’s, males > females
- May obviously cause severe visual loss if circulation is not restored (<6hrs)
- Usually caused by either embolus or thrombus (CAD, AF, sickle cell, valvular heart disease, diabetes, oral contraceptives)
- Diagnosed by fluorescein angiography or optical coherence tomography
- Treated by: hyperventilation with 95% O2, 5% CO2, ocular massage, Diamox (acetazolamide 500mg IV stat), sublingual nitroglycerine, Methylprednisolone 1g IV stat, paracentesis of eye
- Of note tPA treatment has not showed improvement of visual acuity
Retinal Vein Occlusion Hallmarks
- Flame type redness
- So called “blood and thunder”

Amaurosis Fugax
- Transient loss of vision in one or both eyes( therefore visual exam is usually normal at the time of presentation)
- Etiology: Internal carotid artery occlusion or stenosis
- Thromboembolism, vasospasm, cerebrovascular disease, elevated plasma viscosity conditions (leukemia, multiple myeloma)
- A “rule-out” diagnostic evaluation is required, i.e. careful physical exam, labs, head CT, vascular U/S, EKG
Glaucoma
- Increased interocular pressure of the eye (measured > 22 mmHg) which in turn ultimately damages the optic nerve
- Due to the aqueous humor failing to drain properly from the anterior chamber of the eye
- Two Types
- Open angle glaucoma
- Closed angle glaucoma
Open angle glaucoma
- most common type, slow onset, typically painless in the early stages, typical fundoscopic changes on exam
Closed angle glaucoma
- a shift in the lens of the eye with a sudden build up of inner ocular pressure AN OCULAR EMERGENCY
- Typically painful
- Sudden onset
- Presenting headache, nausea, vomiting, halos or rings around lights
Glaucoma Tx
- Historic treatment of slow onset-open angle glaucoma is medication to slow aqueous humor production, newer meds now effect the release system (trabecular system) at the “angle”
- Lasers treatment has been used to put a new hole in the iris to increase drainage
- Stents are now being placed in the eye to facilitate drainage
- Lasers are being used on the trabecular meshwork and associated structures
** “Angle” refers to the reference points between the iris and cornea; where the interocular fluid drains into the venous system
Typical fundoscopic changes in glaucoma
- increased disc to cup ratio
- > 6:10 ratio is suspicious for glaucoma

Scleritis
- Severe, destructive, inflammation involving the sclera and episclera of the eye
- Most commonly seen in women aged 30-50; most often noted in patients with connective tissue disease (RA, lupus, polyarteritis nodosa); may be seen with infection; 50% have unknown etiology
- Presents with a deep boring pain of the eye with decreased visual acuity; 14% of patients loose significant visual acuity within 1yr
- Treated initially with a 10 day course of steroids; systemic immunosuppressive medication may be needed; consultation with ophthalmology and rheumatology after initial treatment failure
Amblyopia
- Commonly called “lazy eye”; is the most common cause of visual impairment in children
- Caused by
- strabismus—improper alignment of the eyes (muscle function)
- refractive error of one eye—irregular eye shape
- cataract—congenital clouding of the lens
Amblyopia Tx
- Treatment depends on the cause
- Often putting a patch on the normal eye will improve the patient’s vision because the problem eye is forced to become “stronger”
- Treatment usually only effective till age 12
- Surgery may be necessary
Strabismus
- Involves a lack of coordination between extraocular muscles
- prevents bringing the gaze of each eye to the same point in space
- prevents proper binocular vision → adversely affects depth perception
- 2 main causes:
- Disorder of the brain coordinating the eyes
- Disorder of one or more muscles
- Deviated or crossed eye
- Constant or intermittent
- Also known as:
- tropia- Always deviated (concomitant/constant)
- phoria- Sometimes deviated (in-concomitant/intermittent)
- ~30% of strabismus patients have a family member with strabismus
- Risk factors: premature birth, cerebral palsy, history of seizures, vision loss

Strabismus: types of ocular misalignment
- Esotropia—inward eye deviation
- Exotropia—outward eye deviation
- Hypertropia—upward eye deviation
- Hypotropia—downward eye deviation
- Esophoria—inward eye deviation (when other eye is covered)
- Exophoria—outward eye deviation (when other eye is covered)


