Exam 1 Flashcards
(163 cards)
Key features of the
adaptive immune system

The adaptive immune response is __________
specific: unique antigen receptors cap of recog antigens of specific microbe
diverse: # antigens vitually limitless - lots of different antigen receptors
down side to having such a diverse repertoire of antigens
number of cells capable of recognizing any one antigen is fairly small
solution? clonal expansion
- Daughter cells bare antigen receptor identical to that expressed by the parent cell.
“Clonal Selection” hypothesis
- Lymphocyte clones specific for different antigens develop before encounter with these antigens.
- Antigen recognition triggers the expansion of lymphocytes of a specific clone.
- Thereby specifically increasing the number of cells capable of recognizing/fighting the current infection.
Once the infection is cleared, the adaptive response ….
declines (contracts), however, long lived memory cells remain
Long-lived memory cells allow for …
more rapid and enhanced response upon reencounter with antigen
At 15 months of age, a child received a measles-mumps-rubella (MMR) vaccine. At age 22, she is living with a family in Mexico that has not been vaccinated and she is exposed to measles. Despite the exposure, she does not become infected. Which of the following properties of the adaptive immune system is illustrated in this scenario?
A.Self Tolerance
B.Diversity
C.Specialization
D.Memory
E.Specificity
Memory
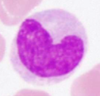
All lymphocytes are morphologically similar
true/false
true!
no difference!

how can different kinds of lymphocytes ID?
unique surface proteins
CD (cluster of differentitation) numerial disgnation
detect CD molecules using antibodies
The most common method used to detect the presence of bound antibody is a technique called
flow cytometry
CDs of
B cells
T cells
NK cells
B: 19, 20, 21
T: 2,3
- CD4: 4
- CD8: 8
NK: 16, 56
B cell function
mediate humoral immunity: prod antibodies
- recognize soluble antigens
- present antigens on surface –> activates B cell
- naive T and B cells rise to effector cells (plasma for B)
- produce soluble antibodies with the same specificity as the membrane bound Ag receptor
- antibodies combat: neutralize, phago, complement sys

Activated effector B cell (Plasma cell)
large cytop: abundant mito & RER –> prod antibody
T cell function
detect antigens derived from foreign proteins or pathogens that have entered into host cells
T cells recognize small fragments of the antigen that have been broken down and presented by antigen presenting cells
- APC captures Ags –> breakdown
- fragment presented to T cell via MHC (major histocompatability complex)
- TCR (t-cell antigen receptor): recog fragment presented –> activates T-cell
- cell mediated imunity
CD4 antigen recognization and effector function
microbial antigen presented by APC
activ macrophages, inflammation, activ T and B lymphocytes
CD8 antigen recognition, effector functions
infected cell expressing microbial antigen
killing infected cell
CD4/CD25 lymphocytes
regulatory
suppressing of immune response
CD16/CD56 lymphocytes
NK
killing of infected cell
B and T cell development
both origin from hematopoietic stem cells in bone marrow
maturation:
- b = bone marrow
- t = thymus
upon release, they are mature –> circulate b/w blod and peripheral lymph organs for antigen response
T lymphocytes
naive cell
activated/effector
memory
Ig isotype
affinity of IG produced
effection functions

b cell deficiencies
abnormalities:
- absent/reduced follicles & geminal centers in lymphoid organs
- reduced serum Ig levels
consequences:
- pyrogenic bac infections
- enteric bacterial and viral infections
t cell deficiencies
abnormalities:
- reduced T cell zones in lymophoid tiss
- reduced DTH rxns to common antigens
- defective prolif response to mitogens in vitro
consequences:
- viral/intracell microbial infections
- p. jiroveci
- atyp mycobac
- fungi
- virus associated malignancies
- EBV assoc lymphoma
innate immune deficiencies
abnormalities:
- variable
consequences:
- pyrogenic bac & viral infections
Memory cells are derived from…
purpose?
antigen stimulated lymphocytes
surv long periods of time in absence of antigens
repond rapidly to reappearnce of pathogen in higher #s compared to naive state( primary respnose)
- enhanced secondary response