Electrophysiology Flashcards
What are the types of action potential present in the heart? Are these fixed?
Working myocardium: with a plateau , and stable resting membrane potential. Occurs in atrial and ventricular myocytes. Pacemaker tissue: no stable membrane potential. In AV, SA nodes. **as you move between the two the action potential types blend/transition to the other. Purkinje fibers and bundle of His are a blend ***
Differences between cardiac muscle and skeletal muscle action potentials
- cardiomyocyte AP is much longer and lasts the length of the contraction so it can’t go into tetanus - cardiomyocyte (working, not pacemaker ) resting membrane potential more negative (closer to equilibrium potential for potassium)
If AV node, SA node, bundle of His and purkinje fibers all have intrinsic pacemaker activity, why is only the SA node the pacemaker?
Because the SA node has the fastest repolarization because it has the most “funny current” channels. So it’s impulse will reach the other areas before they have a chance to fire.
EC coupling in cardiomyocytes
1)action potential reaches dyad/triad2) voltage gated Ca channels open3) Ca binds to Ryr2 and causes Ca release from calsequestrin in SR (Ca channel and Ryr2 NOT physically coupled)4) Ca –> troponin–>tropomyosin–>myosin binding–>contraction4) Ca is resequestered by SERCA or extruded by Na/Ca exchanger
What are the three states of voltage gated sodium channels, calcium channels and transient outward potassium channels and which order must they proceed in? What variable does each transition depend on?
Open–> Inactivated –> Closed Open–> Inactivated depends on time Inactivated—-> Closed depends on membrane potential
Phases of a working cardiomyocyte action potential
0- fast depolarization. 1- repolarization with Na channels inactivated and k channels open 2- plateau with inward Ca balancing outward potassium 3- repolarization, pretty rapid 4- resting membrane potential
Mechanical effects of B1-adrenergic stimulation
-positive inotropy (force of contraction increases)-positive lusitropy (rate of relaxation increases)
Channels and currents involved in phase 0 of a working cardiomyocyte action potential
- voltage gated sodium channels open, rapidly depolarize the cell then inactivate - inward sodium current attempts to reach the Nernst equilibrium potential for sodium.
Channels and currents involved in phase 1 of a working cardiomyocyte action potential
- sodium channels are inactive - potassium channels carrying the transient outward current Ito are open
Molecular mechanisms of positive inotropic and positive lusitropic effects
All mediated by PKA phosphorylation of key proteins.Inotropy-more Ca enters cell with each action potential-SERCA increases velocity-therefore more Ca released by Ryr2Lusitropy-troponin C has less affinity for Ca…lets go sooner-increased SERCA velocity
Channels and currents involved in phase 2 of a working cardiomyocyte action potential
- slow inward ( Isi) AKA Ica, carry calcium into the cell and this balances the outward potassium current ( Ito) at the beginning, and then rapid ( Ikr) and slow (Iks) potassium outward currents (these are called delayed rectifiers)
Channels and currents involved in phase 3 of a working cardiomyocyte action potential
- Calcium channels are inactive - outward potassium current is carried by delayed rectifiers
Channels and currents involved in phase 4 of a working cardiomyocyte action potential
-inward rectifier potassium current directs an outward current of potassium
Channels and currents involved in phase 0 of a pacemaker action potential
-depolarization mediated by slow inward calcium current ( Isi AKA Ica) - No sodium channels
Phases of the action potential in a pacemaker cell
0- depolarization mediated by slow inward calcium current 3-repolarization, funny current starts 4- diastolic depolarization. Analogous to resting membrane potential in cardiomyocytes
Channels and currents involved in phase 3 of a pacemaker action potential
- repolarization due to rapid ( Ikr) and slow ( Isi) delayed potassium rectifiers -The funny current ( both Na and K along their gradients) begins and intensifies and the membrane potential gets more negative
Channels and currents involved in phase 1 of a pacemaker action potential
- the funny current lets sodium in and potassium out - this slowly depolarizes the membrane until threshold is reached
Mechanism behind absolute and relative refractory period in cardiomyocytes
Absolute: sodium channels are inactive and will not convert to a closed state until a certain, negative membrane potential is reached. Relative: a proportion of the channels have become closed, and are now free to open again
Factors influencing conduction velocity
1) Size of cells: smaller cells resist flow 2) Number of gap junctions: more is faster 3) Rise of action potential:
Cardiac cells ranked from fastest to slowest conduction
Purkinje cells > Bundle of His > ventricle/atria > SA and AV nodes
The relative number of beats per minute of pacemaker cells in the heart
SA > AV > bundle of His/ Purkinje fibers
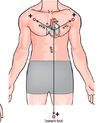
Components of the atrial conducting system
-SA node ( posterior RA wall) - Bachman’s bundle (RA–>LA) - Intranodal branches (SA node–>AV node)
Components of the ventricular conduction system
- AV node ( inferior, medial part of RA) - bundle of His ( from AV node into interventricular septum) - right and left bundle branches (RBB, LBB) ( run down septum parallel) - purkinje fibers ( come off right and left branches the whole way down)
Location and function of the cardiac skeleton
Between atria and ventricles, fibrous tissue that does not conduct an action potential. Its function is to make the action potential go through the AV node and through the bundle of His to get into the ventricles.