Dr. Mhawi 3 Digestive System 3 Liver, Gall Bladder, Pancreas Flashcards
What is the dual blood supply of the liver?
8.6.1
HEPATC PORTAL VEIN
–Carries 75% of blood supply to liver
–Carries blood from small intestine, pancreas and spleen
Essentially depleted of oxygen
§Contains nutrients
§Noxious materials
§ blood cells and breakdown products of blood cells
–From spleen
§Endocrine secretions of pancreas
Hepatic artery
–Carries oxygenated blood to liver
–Makes up remaining 25% of supply
§Blood from hepatic portal vein and hepatic artery is _____as it perfuses hepatocytes of parenchyma
mixed
–Therefore, hepatocytes are never exposed to fully oxygenated blood

What makes up the portal triad?
8.6.1
– branches of hepatic portal vein
– branches of hepatic artery
–draining branches of bile ducts system
Explain the image

Liver, vessels injected with Prussian blue in gelatin. Green lines delineate the boundary of a liver lobule.
What are the 4 structures of the liver?
§Hepatocytes
–PLATES OF CELLS
§Connective tissue (stroma)
–Blood vessels, nerves, lymphatics, travel within CT stroma
§Sinusoidal capillaries (sinusoids)
–Between plates of cells
§Perisinusoidal spaces
(of Disse) (not visible in this low magnification slide)
What are the 3 ways to describe liver lobules

8.6.1
§Classic liver lobule (blue)
§Liver acinus (red)
§Portal lobule (green)
8.6.1
Explain the image

Comparison of the classic liver lobule, portal lobule, and liver acinus. The area indicated in blue shows the territory of each of the three units relating to liver organization and function. The classic lobule has the terminal hepatic venule (central vein) at the center of the lobule and the portal canals containing portal triads at the peripheral angles of the lobule. The portal lobule has a portal canal at the center of the lobule and terminal hepatic venules (central veins) at the peripheral angles of the lobule. The liver acinus has distributing vessels at the equator and terminal hepatic venules (central veins) at each pole.
What are the characteristic of the classic lobule?

8.6.1
§Consists of stacks of anastomosing plates of liver cells (hepatocytes)
–1 cells thick
–Plates of cells radiate from the center toward the periphery of the lobule
§Plates of cells are separated by branching system of sinusoids
–Perfuse cells with mixed portal & arterial blood
§The center of classic lobule is occupied by a large venule: TERMINAL HEPATIC VENULE
– (also called CENTRAL VEIN)
Explain the image
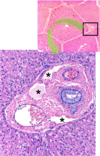
Lower panel is a higher magnification of the portal area where the branches of the hepatic artery, hepatic portal vein, and the bile duct are visible. Space of Mall is indicated by the asterisks.
- 6.1
- 6.1

What are the characteristics of the portal lobule?

8.6.1
§Emphasizes the exocrine function of liver
–Major exocrine function is BILE SECRETION
§Morphologic axis of portal lobule is the i_nterlobular bile duct_ of portal triad
§Outer margins are lines drawn between the 3 central veins closest to the portal triad
§This shows the triangular block of tissue with portions of 3 classical lobules that secrete the bile which drains into its axial bile duct.
What are the characteristics of the liver acinus?

§Described as diamond-shaped or oval- shaped
§Short axis defined by terminal branches of portal triad that lie along border between 2 classic lobules
§Long axis is line between the 2 central veins closest to the short axis
§Provides the best correlation between blood perfusion (heart diseases), metabolic activity, and liver pathology
Describe the 3 zones the liver acinus?
§Zone 1 is closest to the short axis
§Zone 3 is farthest from the short axis and closest to the terminal hepatic venule (central vein)
§Zone 2 lies between zones 1 and 3 but has no sharp boundaries

What are the chacateristics of zone 1?
–first to receive nutrients and toxins
–Last to die if circulation is impaired
–First to regenerate
–First to show degenerative changes following bile duct occlusion (bile stasis)
What are the characteristics of zone 3?
–First to show ischemic necrosis (centrilobular necrosis) during reduced perfusion
–First to show fat accumulation
–Last to respond to toxins and bile stasis
Explain the image

Photomicrograph of centrilobular necrosis in human liver. This photomicrograph shows a routine H&E liver biopsy specimen from an individual with congestive heart failure. Pathologic changes (referred to as ischemic necrosis) are most severe in hepatocytes in zone 3. This zone surrounds the terminal hepatic venule (central vein). This type of necrosis is referred to as centrilobular necrosis. Note the presence of multiple round vacuoles, which indicates extensive lipid accumulation. No noticeable changes are seen in the periphery of the lobule, that is zone 1 and much of zone 2
What are the blood vessels of the parenchyma?

§PORTAL VEIN :
–Lumen larger than that of associated artery
–Provides venous blood to the sinusoids
§HEPATIC ARTERY:
–Thick muscular wall (typical of arteries)
–Provides arterial blood to sinusoids
Question Labeling in Gartner, 6th ed. (2014). Plate 15-3, Fig. 2, page 370.
What are the characteristics of the central vein?

§CENTRAL VEIN:
–Thin wall
–Central position
–Receives blood from hepatic sinusoids
–More properly called TERMINAL HEPATIC VENULE
§Because it is the terminal venule of the hepatic portal vein system
What are the characteristics of sinusoids and explain the image.

8.6.1
§SINUSOIDS:
–Wide blood vessels separating plates of hepatocytes
–Lined with thin endothelial cells
§With wide open fenestrae
–i.e., no diaphragm
§Discontinuous
–Large gaps seen between the cells
–Endothelial cells supported by discontinuous basal lamina
Liver section showing sinusoid capillaries with their endothelial cells close to the hepatocytes. The barely visible thin slit between the hepatocytes and the endothelium is the space of Disse. Kupffer cells can be seen inside the sinusoid. PT stain. High magnification. The structure of the liver sinusoid and its associated cells is illustrated in the upper right panel. Note Kupffer cells and stellate (Ito) cells.