CM-Derm Flashcards
what are the 3 layers of the skin and? what is contained in each?
1. epidermis
- stratified squamous epithelium
- melanocytes, langerhans cells, merkels cells
2. dermis
.3-3.0 mm
-papillary layer
3. subcutaneous layer
what is the function of the skin and nails? (5)
- physical barrier- prevents toxins, organisms, trauma
- temp regulation
- protection against UV radiation
- synthesis of Vitamin D
- sensation
what are the four types of hair?
- lanugo- fine, covers fetus
- vellus- peach fuz
- intermediate- vellus and terminal hair
- terminal-scalp, beard, axilla, pubic area influenced by hormones
what are the 3 phases of hair growth?
- anagen-growth phase, 3 years
- catagen- degenerative stage, weeks
- telogen-resting phase, varies by body site
what are the four functions of hair?
- protection
- regulation of temp
- evaporation of perspiration
- sensation
what is really important thing to do when examining the patient?
UNDRESS THEM
oh la la..NOT!..be professional
what are some things you want to take note of when looking at lesion? (6)
- how many are there?!
- type
- size
- color
- palpation (consistency, mobility, temp, and moisture)
- margination
when there are multiple lesions, what are the three things you want to take note of?
- arrangement/configuration
- confluence
- distribution/location
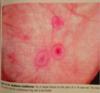
Macule lesion

explain
A macule is a flat, distinct, discolored area of skin less than 1 cm wide that does not involve any change in the thickness or texture of the skin.

papule
explain

A well-circumscribed, elevated, solid lesion, less than 1 cm. Usually dome shaped.

plaque
explaination

A well-circumscribed, elevated, superficial, solid lesion, greater than 1 cm in diameter. Usually “plateau-like” with a flat top.

bullae explaination

A raised, circumscribed lesion (> 0.5 cm) containing serous fluid above the dermis.
crust explaination

Varying colors of liquid debris (serum or pus) that has dried on the surface of the skin.
pustule explaination

A small (< 1 cm in diameter), circumscribed superficial elevation of the skin that is filled with purulent material.

wheel explaination

Transient, circumscribed, elevated papules or plaques, often with erythematous borders and pale centers. These lesions are due to dermal edema and usually resolve within twenty-four hours

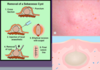
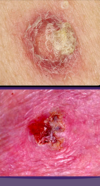
ulcer explaination

A lesion with greater than 50% surface area ulceration.

what are four examples of shapes you can use to describe the skin lesions?
- round
- oval
- annular
- serpiginous

atrophy explaination

Thinning or depression of skin due to reduction of underlying tissue.
what are four patterns you can use to describe the distribution of lesions?
- symmetrical
- exposed areas
- sites of pressure
- random
what is vitiligo
loss of pigmentation
explain what grouped lesions for disseminated would look like?

explain the locations that are common for…:
- acne vulgaris

explain the location of atopic dermatitis

explain the site for photosensitive eruptions?