Chronic pain, brain anatomy, signalling in the NS Flashcards
Which lobe is the precentral gyrus part of?
Frontal
What lobe is the postcentral gyrus part off?
Parietal
Where is Broca’s area?
On the inferior frontal gyrus
Which hemisphere is Broca’s more commonly found in?
The left
Which gyri is the auditory complex found on?
Superior temporal gyri
What is the function of Broca’s area?
Motor aspect of speech - speech associated gestures
What does damage to Broca’s area do?
Expressive aphasia- non-fluent and slow speech
Where is wernicke’s area found?
Within the auditory association cortex
What is the function of Wernicke’s?
Sensory language areas, lexical processing
What can damage to Wernicke’s area cause?
Receptive aphasia - extremely poor comprehension
What are the most anterior and posterior parts of the corpus callosum called?
Genu (anterior)
Splenium (posterior)
What is the rostrum of the corpus callosum?
The part that projects inferiorly and posteriorly from the Genu
Where is CSF made?
Choroid plexus within the ventricular system of the brain
How much CSF is produced per day, and what happens to it when it’s been used?
500ml produced per day 140ml circulates through the subarachnoid space
Reabsorbed into the venous drainage system
What is the function of CSF?
Affords mechanical and immunological protection to the brain and spinal cord
How does CSF pass from the lateral ventricles to the third ventricle?
Interventricular foramen
How does CSF pass from the third ventricle to the fourth ventricle?
Through the aqueduct of midbrain
Which structures make up the lentiform nucleus?
Putamen
Globus palidus
What are the three borders of the lentiform nucleus?
Claustrum
Anterior limb
Posterior limb
Which motor axons pass by the Genu of the lentiform nucleus?
Corticobulbar axons
Which axons pass by the posterior boundary of the lentiform nucleus?
Corticospinal axons
What are the three main pairs of arteries given off by the circle of Willis?
Anterior cerebral arteries
Middle cerebral arteries
Posterior cerebral arteries
Roughly what areas of the brain does the anterior, middle and posterior cerebral arteries supply?
Anterior - frontal and parietal
Middle - temporal
Posterior - occipital
Which eight, fused bones make up the cranial cavity?
Frontal
Occipital
Sphenoid
Ethmoid
2 x parietal
2 x temporal
What are the red flags of lower back pain?
Previous history of malignancy
Younger than 16, older than 50 with new pain
Weight loss
Prolonged steroid use
Recent serious illness
Recent significant infection
List some mechanical causes of lower back pain below.
Trauma
Muscular and ligament pain
Pustular back pain
Facet joint syndrome = ostearthritis
Lumbar disk prolapse
Lumbar spondylosis
Describe the anatomy of an intervertebral disk.
Soft gelatinous centre called nucleus pulposus, encircled by a strong, ring-like collar of fibrocartilage called the annulus fibrosis.
What is the main function of an intervertebral disk?
Shock absorption
What happens in an intervertebral disk prolapse?
Nucleus pulposus is squeezed out of place and herniated through the annulus fibrosis
Name some reasons an IV disk would become damaged?
Trauma
Effects of ageing
Degenerative disorders of the spine
Briefly describe pathology involved once an IV disk herniation has occurred?
Posterior protrusion of the nucleus pulposus towards the intervertebral foramen and its contained spinal root. Annulus fibrosis becomes thin and poorly supported by posterior or anterior ligaments at this point
Which regions of the spine are most commonly involved in disk herniations?
Cervical and lumbar
Where are the signs and symptoms of a disk herniations seen?
Localised to the area of the body innervated by the affected spinal nerve roots- includes motor and sensory
If the nerve roots L4, L5, S1, S2 and S3 are damaged, what condition arises?
Sciatica
Describe where the pain is felt in sciatica?
Spreads down the back of the leg and over the sole of the foot
What are the most common sensory effects from spinal root compression?
Paraesthesia and numbness
What are the most common motor effects from spinal root compression?
Knee and ankle reflexes may be absent or diminished
What are the symptoms of severe spinal disease?
Pain worse at rest
Thoracic pain
Fever
General malaise
Urinary retention
What signs and symptoms of cauda equina compression occur in severe spinal disease?
Bilateral leg pain
Back pain
Urinary retention
Perinatal sensory loss
Erectile dysfunction
Reduced anal tone
What are the layers of protection for the spinal cord?
Vertebrae
Vertebral ligaments
Fat and connective tissue in epidural space
Meninges
CSF
At what point do the spinal nerves stop being covered in meninges?
Once they exit the spinal column through the intervertebral foramen
What is the epineurium?
The outer covering of spinal and cranial nerves - continuous with dura mater
Which meningeal layer contain blood vessels? (At least in the spine :/)
Pia mater and dura mater
Describe the connective tissues of the dura mater.
Thick, strong, dense and irregular
Where does the spinal cord arise and terminate in adults and babies?
-Arises in the medulla oblongata
Terminates:
- superior border of 2nd lumbar vertebrae in adults
- L3,4 in newborns
What is the superior enlargement of the spinal cord, and where does it span?
It’s a cervical enlargement, that nerves to and from the upper limb arise from
Spans from C4 to T1
What is the inferior enlargement of the spinal cord, and where does it span?
It’s a lumbar enlargement, that nerves to and from the lower limb arise from
Spans from T11 to S2
What is the conical structure at the end of the spinal cord called?
Conus medullaris (between L1, 2)
What is the filum terminale?
Extension of pia mater that extends from conus medullaris to the arachnoid and dura mater at the coccyx- anchors spinal cord to coccyx
What is contained in a dorsal root ganglion?
Cell bodies of sensory neurons
What is in the white matter of the spinal cord?
Bundles of myelinated axons of neurons
What are the anterior median fissure and posterior median sulcus of the spinal cord?
Anterior median fissure - wide groove on ventral side
Posterior median sulcus - narrow furrow on dorsal side
What is contained in the grey matter of the spinal cord?
Dendrites and cell bodies of neurons, unmyelinated axons and neuroglia
What are denticulate ligaments?
Triangular shaped membranous extensions of the pia mater than suspend the spinal cord in the middle of the rural sheath
What is found in the centre of the grey commissure?
Central canal - contains CSF
What is there grey commissure?
Crossbar between the two lateral sides of the grey matter
What are nuclei?
Clusters of neuronal cell bodies arranged in functional groups in the grey matter
What parts of the spinal cord are the intermediate grey horns found in, and what do they contain?
Thoracic and upper lumbar Contain autonomic motor nuclei - regulate activity of cardiac muscle, smooth muscle and glands
What is the difference between a nerve and a track?
Nerves are bundles of axons in PNS Tracts are bundles of axons in the CNS
What are the two spinothalamic pathways?
Neospinothalamic tract - fast pain Palaeospinothalamic tract - slow pain
Outline the common course of primary afferent of the spinothalamic pathway
Peripheral receptor, body in the dorsal root ganglion, synapses in the lamina I+II of the dorsal horn, glutamergic
Outline the common course of secondary afferent of the spinothalamic pathway
Body in the lamina I+ II of dorsal horn Cross over to the lateral funiculus Travel through medulla In midbrain give fibres to periaqueductal grey matter and to reticular formation, to hypothalamus In thalamus synapse
When are nociceptors activated?
When the pain reaches a noxious threshold
Describe pain sensitization in relation to nerve fibres?
Continued stimulation decreases the threshold at which nociceptors respond
What type of pain do the C-fibres send to the brain?
The poorly localised, diffuse ‘second’ pain (slow and burning)- polymodal; respond to mechanical, thermal and chemical stimuli
Name the three neurotransmitters used by nociceptive fibres.
Glutamate Substance P Calcitonin gene-related peptide (CGRP)
Outline the common course of tertiary afferent of the spinothalamic pathway
Body in thalamus
Signals to the cerebral cortex
Describe the course of the descending inhibitory tracts
Originate in periaqueoductal grey matter and locus ceoruleus
Synapse in medulla and move down through the inhibitory dorsal columns to the synapse of primary and secondary afferents
How does a thermal stimuli activate A-delta and C-fibres?
Hot activates the TRPV1 receptor
Cold activates the TRPM8 receptor
Results in either cooling or warming of the body behaviours - mediated through projections to the hypothalamus
How does a mechanical stimuli activate A-delta and C-fibres
High threshold
Only activated when stimuli is noxious and may cause tissue damage
How does a chemical stimuli activate C-fibres?
Can be external irritation or substances released during tissue damage
What chemicals are released when tissues are injured?
- Bradykinin
- 5-HT
- Prostaglandins
- Potassium ions
How are C-fibres activated in general?
In response to the chemicals procured by tissues during tissue damage
- CGRP and substance P are released
- mast cells are simulated
- histamine release
- vasodilation, plasma extravasion, oedema and bradykinin release
What happens to the activated threshold after the initial chemical release and vasodilation?
It is lowered to make the area more sensitive to pain
- hyperalgesia
- allondyia
Are the interneurons modulating pain inhibitory/excitatory and what neurotransmitters do they use?
Inhibitory GABA and Glycine
Describe how shifting towards A-beta fires in the gate control theory works.
C and A-delta fibres activate projection neuron firing - causing pain These can be inhibited by inhibitory interneurons A-beta firing activates the inhibitory interneuron
How do endogenous opiods and opiates work?
Stimulates PAG matter in the midbrain, which sends descending, inhibitory pathways that supresses transmission of pain signals
Names the three classes of endogenous opioids.
Endorphins Enkephaline Dynorphin
Name three types of opioid receptor.
mu kappa delta
How is back pain managed between the ages of 5 and 20?
It’s likely to be mechanical - managed with analgesia, brief rest and physiotherapy
What is the best way to manage back pain (in any age)?
Physiotherapy Being as active as possible Early management
Describe the role of the pysiotherapist in management of back pain
Builds up muscles to cope with problems Prevents and manages musculoskeletal disorders/other health problems Works in hospital or community Passive modalities to assist pain relief - electric stimulation Provides pain relief
What is nociception?
The neural mechanism by which an individual detects the presence of a potentially tissue harming stimulus
What are the stages of nociception?
Transduction Transmission Modulation Perception
Through which type of sensory vesicle is pain felt and where they are located?
Free nerve endings - skin, bone, muscle, internal organs, blood vessels - not in brain
Name the 2 levels of pain modulation
Spinal: gate control theory Supra-spinal: Conditioned pain modulation
Describe the role of the hospital specialist in management of back pain
Further evaluates, manages and treats the underlying problem causing the back pain Cause may be mechanical, metabolic, malignant or infectious
What is a ‘yellow flags’, when regarding back pain?
Psycho-social barriers to recovery
List some yellow-flags of back pain.
Belief that pain is harmful and debilitating Fear - avoidance behaviours Sickness behaviours - extended rest Social withdrawal Emotional problems - constant low mood Problems at work Financial problems Overprotective family Inappropriate expectations of treatment
What are the two different types of pain?
Neuropathic - nerve damage Nociceptive - tissue damage
Describe somatic nociceptive pain.
Well localised - dermatomal Sharp, aching and gnawing pain Constant
Describe visceral nociceptive pain.
Vague distribution, diffuse Dull, cramping and digging pain Can be periodic Causes nausea, vomiting, sweatiness, CV symptoms
What are the symptoms of neuropathic pain?
Shooting Electric shock like Burning Tingling Numbness
What kind of pain is lower back pain? (neuropathic, nociceptive)
Local nociceptor activation = nociceptive Compression and inflammation of nerve root = neuropathic
What’s the difference between somatic referred back pain and radicular pain in the leg?
Somatic referred pain - nociceptive pain affecting large areas of the posterior thigh Radicular pain - neuropathic pain radiating down lower limb to the heel in a narrow band
How can pain be measured?
NRS - numerical rating scale VAS - visual analgoue scale
Name some of co-morbidities associated with neuropathic pain.
Poor appetite Anxiety Depression Difficulty concentrating Drowsiness Lack of energy Difficulty sleeping
Describe the WHO analgesic ladder
1 - Paracetamol, NSAIDs 2- Codeine, dihydrocodeine 2-3 Tramadol 3 - Morphine, methadone, oxycodone
What are the possible side effects of NSAIDs?
GI ulceration Bleeding Renal problems Asthma Decreased bone healing
What criteria must be looked at before prescribing opioids?
Appropriate - pain model- pain patient- pain prescription
From most to least effective, list conditions opioids can be used in.
Arthritis Nueropathic pain Lower back pain Visceral pain Fibromyalgia
Name some adjuvants which can be used for neuropathic analgesics.
Anti-depressants Anti-convulsants Anti-arrhythimcs
Describe the lumbar facet syndrome.
Lower back pain to groin, hip or thigh Worse on back extension/rotation Tender over paraspinal region
How is lumbar facet syndrome diagnosed?
X-ray shows nothing local anaesthetic to medial branch of dorsal primary rami
What is resting membrane potential?
Difference in charge between inside and outside of the neuron/cell at rest
What is the typical resting membrane potential?
-60 mV to -70 mV
What is equilibrium potential?
Membrane potential where N ions entering cell = N ions leaving cell E.g. concentration gradient moves K+ out of cell but electrical potential gradient moves K+ into cell
What is action potential?
Very brief, but dramatic change in membrane potential All or nothing
What are the stages of action potential?
Depolarisation Repolarisation Hyperpolarisation
What happens during depolarisation?
Fast opening of voltage-gated Na channels
What happens during repolarisation/ hyperpolarisation?
Slow opening of voltage-gated K channels
Name 2 ways in which an action potential can be propagated
- along axon 2. out of axon via membrane
What cells myelinate neurons in CNS?
Oligodendrocytes
What cells myelinate neurons in PNS?
Schwann cells
How does action potential propagation differ in myelinated and umyelinated neuron?
Myelinated: AP jumps from node to node, faster Unmyelinated: slower, cannot jump
Name 2 disorders associated with defective myelination
Multiple sclerosis (CNS, autoimmune) and Guillan-Barre syndrome (PNS, inflammatory)
Outline the steps in synaptic transmission
- AP enters presynaptic terminal 2. Ca2+ entry through voltage-gated Ca2+ channels 3. Docking of synaptic vesicles containing neurotranmitters 4. Neurotransmitter released by exocytosis 5. Neurotransmitter binds to and activates receptors on postsynaptic membrane 6. Ions enter cells Na+ = depolarisation Cl- = hyperpolarisation
Name 5 types of neurotransmitters
Cholinergic Biogenic amines Amino acids Neuropeptides Miscellaneous
Name example of cholinergic neurotransmitter
Acetylcholine
Name example of biogenic amines neurotransmitters
Catecholamines: noradrenaline, adrenaline, dopamine 5-hydroxitryptamine
Name example of amino acids neurotransmitter
Excitatory: glutamate Inhibitory: GABA
Name example of neuropeptides neurotransmitter
Endogenous opioids
Name example of miscellaneous neurotransmitter
Gases: NO Purines: adenosine, ATP
Name 2 diseases that disrupt cholinergic transmission
Botulism (toxin prevents Ach release), Myasthenia gravis (inflammatory)
What is temporal summation?
Frequency of firing of APs at one point
What is spatial summation?
Firing at multiple sites combines e.g. 2 different dendrites
What does inhibitory postsynaptic potential?
Moves the post-synaptic membrane further away from threshold
What does excitatory post-synaptic potential do?
Brings the post-synaptic membrane closer to threshold
Name the 2 ways in which information can spread in the nervous system
Divergence (one neuron signals to many, spreading the signal) and convergence (integration of many signals to one cell)
What are the methods used to localise cerebral function?
Electro-encephalography (EEG) PET fMRI Transcranial magnetic stimulation (TMS)
What is the function and role of EEG in investigating brain?
Records the electrical activity of the brain Investigate cognitive processes in response to a stimulus
What is the function and role of PET in investigating brain?
Measures blood flow - radioactive injected Locate brain activity while performing a task
What is the function and role of fMRI in investigating brain?
Measures blood flow Locate brain activity while performing a task
What is the function and role of TMS in investigating brain?
Electromagnet to stimulate brain activity Interrupt brain activity while performing a task
List the disadvantages of pain
CNS - anxiety, depression, sleep deprivation CVS - increased BP, HR and risk of ischaemic heart disease RESP - inhibits cough, hyperventilation GIT - nausea, vomiting Genitourinary - urinary retention, uterine inhibition Muscle - restless, immobility Metabolic - Acute catabolic stress response - cortisone, glucagon..
Describe the Gate Control Theory of Pain
In absence of input local tonically active inhibitory interneuron suppresses pain pathway With strong pain, C fibres stops inhibition -> signal send to brain If Abeta fibres are also activated they reactivate the interneuron and decrease the painful stimulus
Name compartments of the supraspinal pain neuromatrix
Sensory discriminative: Thalamus, Post insula Affective-motivational: Ant insula cortex, Ant mid cingulate cortex Cognitive activation: Prefrontal cortex
Define allodynia
Pain from a stimulus not normally painful
Define Hyperalgesia
Abnormally high levels of pain from noxious stimuli Primary - Peripheral sensitisation Secondary - central sensitisation
What are the mediators that activate nociceptors?
K+ 5-HT Bradykinin H+ Histamine ATP, Adenosine
What are the mediators that sensitise nociceptors?
Prostaglandins Leukotrienes Substance P Noradrenaline Neurokinin A CGRP Nitric oxide Reactive oxygen species
Describe the mechanism of peripheral sensitization
Change nociceptors from high to low threshold Process continues after the initial stimulus has ended Mediators: ATP, H+, NGF, Sub P, histamine, cytokines, PGI2, bradykinin
What are the neurotransmitters that are part of conditioned pain modulation in the CNS?
NA 5HT Inhibitory
What are the red flags of lower back pain?
Wt loss - malignancy Fever Signs of systemic inflammatory disease Anatomical change Possible history of trauma Cauda equina syndrome Neurological signs - radiculopathy (pinched nerve)
Outline the triple response after a mild trauma
Red reaction - after scratching White wheal - around the scratch Flare - redder area of the skin
Describe the mechanism at the scratch site in triple response reaction
Tissue damage: K+ and prostaglandins released Plasma releases bradykinin, platelets: 5HT -> activation of free nerve endings CGRP and sub P release - activate mast cells (histamine release), dilation of blood vessels (flare), sub P (oedema)
Describe ischaemic pain
Results from a lack of adequate blood supply to active tissue Release of activating and sensitizing molecules resulting in breakdown of ATP
What are vertebral foramina?
All of them together form the vertebral canal
Define transverse processes of vertebrae
articulate with ribs in thoracic region, junction of pedicle and lamina
Where are the superior and inferior articulate processes?
At the junction of pedicle and lamina
What do superior and inferior vertebral notches form?
The intervertebral foramina
Name the outer and inner layer of intervertebral disc
Anulus fibrosus - outer Nucleus propulsus - inner
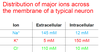
Give the distribution of major ions across the membrane of a typical neuron
Label the areas of cortical specialisation


Label


What is the structure and label its parts


Label


Describe the parts of the lentiform nucleus

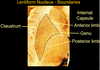
Label


Label


Label diagram


Label diagram


Label diagram


Which centre in the medulla controls the tone of blood vessels and thus total peripheral resistance in relation to pain?
The rostral ventrolateral medulla
List the signals that the rostral ventrolateral medulla integrates
- From periaqueductal grey matter
- Cerebral cortex signals
- Paraventricular nucleus in hypothalamus
- Nucleus of the solitary tract
What signals does the periaqueductal grey matter receive?
Pain signals
What signals and where from, where to does the paraventricular nucleus in hypothalamus receive?
From the rostral ventrolateral medulla and nucleus of the solitary tract
Sends signals back to both these structures and to the intermediolateral column in spinal cord
Where from does the nucleus of the solitary tract receive signals?
Baroreceptors and Paraventricular nucleus of the hypothalamus
Where does the nucleus of the solitary tract signals to?
Paraventricular nucleus in the hypothalamus, rostral ventrolateral medulla and Nucleus ambiguus
What is the role of nucleus ambiguus in the total peripheral resistence during pain response?
Receives signals from cerebral cortex, hypothalamus and nucleus of the solitary tract
Sends signals to heart
What are the final signals to the spinal column in the total peripheral resistance pathway?
The paraventricular nucleus in the hypothalamus and the rostral ventrolateral medulla signal to the Intermediolateral column in spinal cord T1-L3; than to postganglionic sympathetic nerve activity
What are the final effective signals of the total peripheral resistance pathway?
Vascular tone
Renal nerves
Other viscera


