Chapter 6 Flashcards
hematopoiesis occurs via a stepwise maturation of CD34+ hematopoietic stem cells converting into either myeloid stem cells or lymphoid stem cells
Myeloid stem cells can transform into erythroblasts, myeloblasts (neutrophils, basophils,eosinophils), monoblasts (monocytes), and megakaryoblasts
Lymphoid stem cells can become either B or T lymphoblasts
Cells mature and are released from the BM into the blood
A normal WBC is 5-10 K/uL
low WBC= leukopenia, high WBC= leukocytosis
What are the main causes of neutropenia?
- Drug toxicity (eg. chemo with alkylating agents)-damage to stem cells
- Severe infection (e.g. gram-negative sepssi)- increased movement of neutrophils into tissues results in decreased criculating neutrophils
As a tx, GM-CSF or G-CSF may be used to boost granulocyte production, therbu decreasing risk of infection
What are the main causes of lymphopenia?
- Immunodeficiency
- High cortisol state (e.g. exogenous steorids or cushing syndrome)
- Autoimmune
- Whole body radiation- lymphopenia is the first cell sign to go with radiation
What are some causes of neutrophilic leukocytosis?
- Bacterial infection or tissue necrosis- induces release of marignated pool and BM neutophils, including immature forms (immature cells are marked by decreased Fc receptors (CD16)
Basophilia is classically seen in ______
CML
Causes of lymphocytic leukocytosis?
- Viral infections- T lymphocytes undergo hyperplasia in response to virally infected cells
- Bordetella pertussis infection- products lymphocytosis- promoting factor, which blocks circulating lymphocytes from leaving the blood to enter the lymph node
What causes infectious mononucleosis?
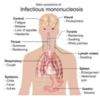
EBV infection that results in a lymphocytic leukocytosis comprised of reactive CD8+ T cells (CMV can also cause)
During this, EBV is spread via saliva and primarily infects the oropharynx, resulting in pharyngitis, the liver, resulting in hepatitis with hepatomegaly and elevated LEs, and B cells
Again, in Infectious mono the main immune response is via CD8 T cells, resulting in:
- Generalized LAD due to T-cell hyperplasia in the lymph node paracortex
- Splenomegaly due to T-cell hyperplasia in the PALS
- High WBC count with atypical lymphocytes (reactive CD8 cells) in the blood

How is Infectious mono diagnosed?
Monospot test for screening- detects IgM Abs that cross-react with horse or sheep red blood cells (heterophile Abs). Usually positive 1 week after infection
A negatve monospot test suggests CMV as a possilbe cause of IM
Definitie diangosis made via serologic testing for the EBV viral capsid antigen
What are the complications of infectious mono?
Increased risk of splenic rupture- avoid contact sports
Rash is exposed to ampicillin
Dormancy of vius in B cells elads to increased risk for both recurrence and B-cell lymphoma, especially if immunodeficiency develops
What is acute leukemia?
A neoplastic proliferaiton of blasts; defines as the accumulation of 20+% of blasts in the BM
Incresaed blasts crowd out normal hematopoiesis, resulting in an acute presentation with fatigue, anemia, thrombocytopenia (bleeding), or neutropenia (infection)
The blasts then enter the blood stream, resulting in a high WBC count.

Acute leukemia is divided into:
acute lymphoblastic leukemia (ALL) and acute myelogenous leukemia (AML)
What is ALL?
Neoplastic accumulation of lymphoblasts (20+%) in the BM
lymphoblasts are marked by positive nuclear staining for TdT, a DNA polymerase (TdT is absent in myeloid blasts and mature lymphocytes)
Who gets ALL?
Mostly children, associated with down syndrome (usually arises AFTER 5 yo)
What are the subtypes of ALL?
B-ALL and T-ALL
B-ALL
-Most common subtype, usually marked by lymphoblasts (Tdt+) that express CD10, CD19, and CD20
Excellent response to chemo, requires prophylaxis to scrotum and CSF
What is the prognosis of B-ALL based on primarily?
Cytogenetic abnormalities
t(12:21) has a good response; common in children
t(9:22) has a poor prognosis (PHiladelphia); common in adults
T-ALL
Marked by lymphoblasts (TdT+) that express markers ranging from CD2 to CD8 (e.g. CD3,CD4, CD7). Dont express CD10
Usually presents in teenagers as a medistinal (thymic) mass (called acute lymphoblastic lymphoma becuase the malignant cells form a mass)
What is acute myeloid leukemia?
Neoplastic accumulation of immature myeloid cells in the BM- Myeloblasts are usually positive for MPO
Crystal aggregates of MPO may be seen as Auer rods

Who gets AML?
Most common in older adults; 50-60+ yo
Subclassification of AML is based on cytogenetic abnormalities, linegae of immature myeloid cells, and surface markers. What are the man subtypes?
- Acute promyelocytic leukemia (APL)
- Acute monocytic leukemia
- Acute megakaryocytic leukemia
Describe Acute promyelocytic leukemia (APL)
– Marked by a t(15:17) which involves translocation of the retinoic acid receptor (RAR) on chrom 17 to chrom 15; RAR disruption blocks maturation and promyelocytes accumulate
- Increased risk of DIC
- Tx with all-trans-retinoic- acid (vitA derivative), which binds the altered receptor and causes the blasts to mature (and eventually die)
Describe acute monocytic leukemia
Proliferaiton of monoblasts; usually lack MPO
Blasts prolifeate in the gums (below)






















