Ch. 17 pt 2 Flashcards
how does salmonella present clinically
acute - anorexia, abd pain, bloating, N/V, bloody diarrhea w/ short asymp phase –> bacteremia & fever w/ flu-like symp
abd pain may mimic appendicitis
erythematous maculopapular rash (Rose spots)
systemic- extraintestinal complication = septic arthritis, abscess, osteomyelitis, encephalopathy, meningitis, seizures, endocarditis, myocarditis, pneumonia & cholecystitis
what is the pathogenesis of ischemic bowel dz
what variables determine the severity of the dz
two phases:
- initial hypoxic injury
- reperfusion injury
severity:
- severity of vascular compromise
- time frame
- vessels affected (more proximal, more significant)
What is the morphology of shigella
L colon (but ileum may be involved)
abundance of M cell in dome epithelium overlying Peyers Patches
mucosa = hemorrhagic, ulcerated & pseudomembrane
histology of early cases similar to self-limited colitides (like Campylobacter colitis)
tropism for M cells, aphthous ulcers similar to Crohns dz

What is the pathogenesis of colon CA
- APC/B-catenin/Wnt path –> classic adenoCA sequence (80% sporadic mutations)
- Microsatellite instability (MSI) path –> defect in DNA mismatch repair
both paths = accumulation of multiple mutations but differ in genes involved & mechanism by which mutations accumulation
epigentic events - MC = methylation induced gene silencing –> enhance progression along either path

which etiologies of colon CA cause sesile serated adenomas & mucinous adenocarinoma
DNA mismatch repair defect
- MYH-associated polyposis = AR
- Hereditary non-polyposis colorectal cancer - R-side = AD
- Sporadic CA (10-15%)- R side
&&&
hypermethylation = Sporadic CA (5-10%) - R side
How does salmonella cause infection
very few vaible strains cause infxn
= absence of gastric acid, in ind w/ atrophic gastritis or those on acid-suppressive therapy
penetrates SI mucus layer –> transverses the intestinal epithelium thru M cell on Peyer’s patches –> causes Peyers patches in terminal ileum to enlarge & elevations –> hyperplasia –> points of intussusception Mesenteric LN =enlarged
what are characteristics of Schistosoma
*know!!!*
from snail –> ingested
adult worms residing w/i mesenteric veins
sxs by trapped eggs w/i the mucosa and submucosa
granulomatous immune rxn –> bleeding and obstruction
–> SCC bladder
–> cirrhosis (2nd MCC)
what are freq abnormalities in the SI an LI
what are the causes
malabs & diarrhea: disrupt normal h2o and nutrient transport
infectous & inflam disorders: intestinal bacteria 10x # of eukaryotes in the body
Colon = MC site of GI neoplasia in the Western pop
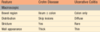
Campylobacter spp.:
geography
transmision
epidemiology
GI site
reservoir
symptoms
complications
high income countries
poultry, milk, contaminated water, other foods - food poisoning
sporadic__, children, travelers
colon
farm animals
water/bloody diarrhea- (travelers diarrhea)
reactive arthritis (pt w/ HLA-B27), guillain-barre syndrome, erythema nodosom
when do you begin regular surveillance colonoscopies
age 50
younger is african american or FHx
polyp removal reduce the incidence of colorectal adenocarcinoma
What are diagnostic tests used infectious enterocolitis
selective serologic testing (giardia Ag)
fecal leukocytes (evidence of invasion)
fecal lactoferrin
stool culture
assays for toxins (C. diff toxin)
stool for ova & parasites
Lactose def = lactose cant be broken down to glu and galac, so it stays in lumen and exerts osmotic forces to attract fluid & cause diarrhea
what are the 2 types of lactose def
- congenital: mutation in gene encoding lactase; _auto re_c; explosive diarrhea w/ watery, frothy stool & abd distention w/ milk ingestion
- aquired: downreg of lactsoe gene expression; native american, african american, chinese; may present after enteric viral/bacteral infxn
(Bx is unremarkable for biochem defect)
Which dz’s have defect of only transepithelial transport
carcionoid syndrome
Abetalipoproteinemia

what are the steps of MMR carinogenesis (10-15 % sporadic & HNPCC)

what are characteristics of intestinal hookworm
penetrate skin –> develop lungs –> migrate to trachea & swallowed
suck blood & reproduce in the duodenum –> multiple superficial erosions, focal hemorrhage, and inflammatory infiltrates
Chronic infxn leads to iron deficiency anemia
neoplasia in IBD are related to..
duration of dz - > 8-10 yo
extent of dz - pancollitis > chance than if only L side dz
neutrophilic response: active inflam
(acquired conditions predispose to CA; chronic inflam, DALM = dysplasia associated lesions or mass (aka precursor lesions) & immune def)
What are characterisitics of V. cholerae
comma-shaped, gram (-)
India & Bangladesh, areas of natural disaster
cause cholera
transmitted in shellfish, contaminated H2O (fecal-oral)
Severe cases: ‘rice water diarrhea’ with fishy odor ==> dehydration
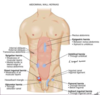
label this


what is the epidemiology of Colon Cancer
highest incidence = North america - bc dietary factors = low fiber, high fat/refined carbs
USA- 2nd MC cause of cancer death
peak incidence = 60-70 yo (rarely under 50 UNLESS HNPCC!)
use of ASA & NSAID –> prevention (inhibit COX-2)
What are characterisitics of obstructions due to adhesions
MC obstrution in USA
most often = acquired (surgery, trauma, intra-abd infxn, endometriosis)
healing –> fibrous bridge that creates loops where material can get lodges btn the bowel & adhesion

When/How do the SI and LI form embryonically
=4th & 5th wk
quickly outgrow the space –> entire midgut herniate into the umbilical cord - form loop
rotate –> pulled back for midline closure

Wht are characterisitics of adenovirus
common cause peds diarrhea & immunocompromised diarrhea
droplet/close contact transmission
SI bx show epithelial degeneration but more often non specific villous atrophy & compensatroy crypt hyperplasia
nonspecific sxs - resolve after 10 days
what are other causes of chronic colitis
what are characteristics of each
diversion colitis: blind colon segment bc of SRG resulting in ostomy; develop numerous mucosal lymphoid follicles; cure = re-anastamonsis
microscopic colitis: both types = watery diarrhea w/o wt loss; collagenous-in mid-age F; lymphocytic- in celiac dz & auto immune dz
graft-vs-host dz: after allogenic hematopoietic stem cell transplantation; crypts severely destroyed; watery diarrhea may become bloody in severe cases
what is the distinction between UC and Crohns primarily based on?
what are these characterisics for crohns dz
distribution & morphology
- MC: terminal ilieum, ileocecal valve, cecum (40% limited to SI & 30% SI & LI); multiple, sharply delineated areas (skip lesions)
- intestinal wall = thickened/rubbery bc transpural edema, inflam, submucosal fibrosis & hypertrophy of muscularis propria
- extensive transmural dz –> creeping fat - mesenteric adipose tissue extend over the serosal surface

What are the characterisitics of Ascaris lumbricoides
ingest eggs hatch in intestines –> larvae penetrate mucosa –> migrate to systemic circulation –> enter the lungs & grow w/i alveoli –> cough up and swallowed –> mature into worms –> eosinophilic-rich inflam rxn –> physical obstruction/the intestine/biliary tree
eggs in stool
fecal-oral
What is the clinical presentation of Campylobacter enterocolitis
water/bloody diarrhea
(bloody - bacterial invasion; minority of Campylobacter strains)
enteric fever: when bacterial prolif w/i lamina propria & mesenteric LM
what are the clincal features of colon CA
screening colonoscopy does not equal staging
R vs L sided CA
- R side = fatigue, weak bc Fe def anemia; older M or postmenopausal F
- L side= occult bleeding, changes in bowel habits, cramping & LLQ discomfort
prognostic factors depth of invasion & presence of LN metastasis
metastasis MC to liver
5 yr survival - 65%
what genes are associated w/ Crohn’s dz & UC
Crohns: Th17 & Il-23(p40 & p19), IL-23 receptor complex, CCR6, TNFSF15, JAK2/STAT
UC: all EXCEPT TNFSF15
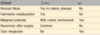
What are the difference of clinical presentation of crohns & UC
perianal fissures?
fat/vit malabs?
malignancy?
recurrence after SRG?
toxic megacolon?
what are the clinical manifestations of intestinal obstruction
Abd pain (localized or diffuse), abd distention
vomiting, constipation
*rmr these DO NOT tell etiology*
How do you confirm the Dx of Shigella
how do you treat
stool culture
Abx shorten the clincal course & duration of bacterial shedding
anti-diarrheal medications can prolong sxs & delay clearance
how can Yersinia present clinically
how does cause infxn
in ileum, R colon, appendix – abd pain, fever, bloody diarrhea (can mimic appendicitis)
prolif extracellularly in lymphoid tissue –> regional LN & Peyer path hyperplasia as well as bowel wall thickening
mucosa overlying lymphoid tissue –> become hemorrhagic & aphthous erosions & ulcers ; may appear w/ neutrophil infiltrates & granuloma
(may be confused w/ crohns dz (like shigella))
reactive arthritis, with urethritis, conjunctivitis, myocarditis, erythema nodosom, and kidney dz
what are specifics about C. jejuni
MC bacterial enteric pathogen in developed countries
traveler’s diarrhea (food poisoning - chicken, unpasteurized milk, contaminated water)
Whipple dz
geography
epidemiology
GI site
symptoms
complications
rural > urban
rare, white men (particularly farmers)
SI
Malabs- triad: diarrhea, wt. loss, arthralgia
arthritis, arthralgia, fever, LAD, neurologic, cardiac or pul dz, CNS dz (may present before malabs by mon-yrs)
what is the immune response in pts w/ intestinal inflam
==> increased bacterial exposure - disruption of mucus layer, dysreg of tight jxns, increased intestinal permeability, increased bacterial adherence to epithelial cells
innate cells –> increase leves of TNF-a, IL-1B, 6, 12, 23 and chemokines –> expansion of lamina propria w/ increased CD4 cells (esp pro-inflam T subgroup) –> secrete cytokines & chemokines –> recruit leukocytes –> cycle of inflam

define diarrhea
differentiate it from dysentery
increase in stool mass, freq, fluidity
typically > 200 gm/day
severe cases- stool vol can exceed 14 L/day
w/o fluid resuscitation –> Death
dysentery = painful, bloody, small volume diarrhea
Pseudomembranous colitis (C. Diff) - (aka ABx-associated colitis/diarrhea)
geography
transmision
epidemiology
GI site
reservoir
symptoms
complications
worldwide
ABx allow emergence
immunosuppressed, ABx-treated
colon
humans, hospitals
water diarrhea, fever
relapse, toxic megacolon
what category does shigella belong to
gram neg, unencapsulated, nonmotile, facultative anaerobe
what are characteristics of autoimmune enteropathy
how does it differ from celiac dz
X-linked (germline LOF FOXP3)- severe diarrhea & autoimmune dz in children
severe familal form = IPEX = immune dysreg, polyendocrionpathy, enteropathy & X-linkage
autoAb of enterocytes & goblet cells & some have autoAb to parietal/islet cells
neutrophils infiltrate intestinal mucosa (unlike celiac!)
=give immunosuppressive drugs
What are characteristics of Strongyloides stercoralis
penetrate unbroken skin –> migrate thru lungs –> induce inflam infiltrates –> reside in the intestines maturing into adult worms
autoinfection: eggs can hatch w/i the intestine and release larvae that penetrate the mucosa
infection can persist for life
larvae stage is OUTSIDE human host strong tissue rxn and induce peripheral eosinophilia
what are clinical features of IBS
abd pain 3 days/month over 3 months
improves w/ defecation
chronic, relapsing abd pain, bloating, changes in bowel habits without changes in the gross pathology or histology
dx based on clinical critera (Rome criteria)
what is the presentaton of pseudomembranous colitis
fever, leukocytosis, abd pain, cramps, water-diarrhea & dehydration
protein loss–> hypoalbuminemia
fecal leukocytes & occult blood
toxic megacolon - marked dilation of colon - marked injury to the colonic wall
What are juvenile polyps
<5 yo; sporadic or syndromic (AD)
rectal location (SB and stomach if syndromic)
dysplasia present –> risk of gastic, SI, colonic, pancreatic adenocarcinoma
can be associated w/ rectal bleeding intussusception, intestinal obstruction or polyp prolapse
congenital malformations, digit clubbing
mutation: SMAD4 –> affect TGF-B signaling

what are characteristics of Cryptosporidium spp
Chronic diarrhea- AIDs pts
oocysts resistant to chlorine - need to freeze/filter
ENTIRE life cycle in a single host
attach brush border & damage enterocyte –> malabs of sodium, chloride secretion, an increased tight junction permeability – non-bloody watery diarrhea
terminal ileum and proximal colon
present thru GIT, biliary tree, and the resp tract of immunodeficient hosts
diagnosis == oocysts in the stool
What is the pathogenesis/morphology of whipple dz
dense accumulation of distended foamy macrophages in small intestine lamina propria & many argyrophilic rods in LN
PAS-positive bacteria, diastase-resistant granules that represent partially digested bacteria w/i lysosomes
H&E stain- normal lamina propria by distended macrophages; micrograph of macrophase show bacilli w/i cell -seen at higher magnification
==> look similar to TB; acid fast stain help you differentiate TB (+) and Whipple dz (-)

what is the distribution and morphology of UC
ALWAYS involved rectum & extends proximally in contninous fashion
if entire colon = pancolitis –> backwash ileitis- mild inflam of distal ileum in pancolitis
limited = descriptive (ie ulcerative proctitis or proctosigmoiditis)
NOT transmural –> so colon wall = THIN, surface serosa normal & no strictures
what is the fxn of Th17 cells in intestinal inflam
express CCR6 & IL-23 receptors (include IL-23 receptor complex & IL-12 receptor B1)
APC secrete IL-23 (p19 & p40)
interact w/ receptor –> (+) JAK2 signal transducers –> (+) STAT3 –> regulate transcriptional activation
IL-23 –> contribute to Th-17 cell prolif, survival or both
actions of IL-23 enhanced by TNFS15
- which dz has a defect of only terminal digestion?
- which one is the only one w/ a defect in lymptic transport
- disaccharidase def
- whipple dz

what are hamarthomatous polyps
sporadic or due to genetic/acquired syndrome;
have underlying germline mutation in tumor suppressor gene/proto-oncogene
some increase risk for CA
how do you characterize E. coli
(what are specifics about each strain)
gram (-) bacilli; colonize healthy GI tract;most are nonpathogenic but subset cause human dz
ETEC: principal cause of traveler’s diarrhea, secretory, non-inflam diarrhea
EPEC: produce attaching/effacing lesions in which bacteria attach tightly to the enterocyte apical membrane & cause local loss
EHEC: O157:H7 –> HUS
EIEC: invade epithelial cells causing nonspecific, acute self-limited colitis

what are characteristics of Enterobius vermicularis (pinworm)
do NOT invade host tissue
entire life w/i the intestinal lumen == rarely cause illness
fecal oral
female migrates to anal orifice –> deposits eggs on perirectal mucosa –> lot of irritation, leads to itching
scotch tape test
what is clinical presentation of crohns
20% pt present w/ acute RLQ pain, fever, bloody diarrhea (mimic appendicitis/bowel perforation)
dz onset associated w/ initiation of smoking
malabs –> malnutrition, hypoalbeminemia, Fe def anemia
increased risk fo adenocarcinoma
Ab to saccharomyces cervisiae (not in UC!)
what is the clinical presentation of Shigella
incubation up to 1 wk
self limited dz
7-10 days of diarrhea, fever, abd pain
watery diarrhea –> dysenteric phase (50%)
persist as long as 1 month (shorter in children; but more severe)
adults: uncommon subacute weeks of waxing/waning diarrhea - mimic new-onset of UC
what is the clinical presentation of UC
inital attack may be severe –> medical/SRG emergency
bloody diarrhea w/ stringy, mucoid material & abd pain
triggers = infectious enteritis, psych stress, STOP smoking (smoking may relieve symps…..)
what is the epidemiology of salmonella
typhoid fever (enteric fever) - worldwide incidence of 30 mil
S. enterica; 2 subtypes (typhi -endemic countries & paratyphi-travelers)
children/teens - endemic areas
no age preference - non-endemic areas
infxn associated w/ travel to india, mexico, philippines, pakistan, el salvador, haiti
gallbladder colonization w/ S. typhi/paratyphi may be assocaited w/ gallstones & chronic carrier state
what is the most freq cause of intestinal obstruction world wide?
what are the associated characteristics & complications
hernias = 3rd MC in USA
most freq = inguinal (narrow orifice & large sac)
complications = pressure at the neck of the pouch may impair venous drainage of entrapped viscus –> stasis & edema –> increase bulk of herniation –> permanent entrapment –> strangulation –> infarcture
What is the MCC of acute gasteroenteritis requiring medical attn
what are its characterisitics
norovirus= ssRNA
fecal-oral
spreaad w/i schools, hospital, nursing homes, cruise ships
significant prob in immunocompromised pts
villous shortening, loss of brush borders, crypt hypertrophy, lymphocytic infiltration
Salmonella
geography
transmision
epidemiology
GI site
reservoir
symptoms
complications
worldwide
meat, poultry, eggs, milk
children, older adults (peak summer/fall)
colon & SI
poultry, farm animals, reptiels
watery/bloody diarrhea
sepsis, abscess
What does UC look like grossly
colonic mucosa - slightly red & granular or w/ extensive, broad based ulcers
abrupt transition- btn dz & uninvolved colon
ulcers along long axis of colon
isolated islands of regenerating mucosa bulge into lumen ==> pseudopolyps w/ tips that can fuse and create mucosal bridges
chronic –> mucosal atrophy w/ Sm. mucosal surface that lacks normal folds

what is infectious enterocolitis
presents w/ broad range of symps
=diarrhea, abd pain, urgency to defecaate, perianal discomfort, incontinence & hemorrhage
global problem w/ 2,000 deaths per DAY in kids & 10% of death worldwide by age 5
what is the fxn of STK11 gene
instruction for making Ser/Thr kinase 11
= tumor suppressor - help determine the amounf of energy a cell uses
promotes apoptosis
required for normal development in birth
What are characteristics of hyperplastic polyps
L colon, single/multiple
60-70s- bc decreased epithelial cell turnover & delayed shedding of surface epithelial cells –> goblet cells & absorptive cells pile up
what are the classic clinical presentations of a pt w/ ischemic bowel dz
MC > 70 yo, slightly more F
acute –> sudden cramps LLQ, desire to defecate, passage of blood/bloody diarrhea (BRB, hematochezia)
may progress to shock and vascular collapse w/i hrs in several cases
SRG needed if evidence of infarction –> paralytic ileus (decrease bowel sounds), gaurding/rebound tenderness
(CMV & radiation enteritic mimic ischemic bowel dz)
where are polyps most commonly located
what are possible characterisitics
colon & rectum
most begin as small elevations of mucosa = sessile (w/o stalk)
–> can enlarge, prolif into mass and the effects of traction of the luminal protrusion may create a stalk –> pedunculated
classification: neoplastic or not
What are characteristics of Entamoeba histolytica
*know!!*
fecal-oral; india, mexico, columbia
–> liver abscesses and dysentery; abdpain, bloody diarrhea, or wt loss
penetrate splanchnic vessels and embolize to liver producing abscesses
acute necrotizing colitis & megacolon – both = significant mortality
cysts w/ chitin wall and 4 nuclei and resistant to gastric acid
flask shaped ulcer with narrow neck and broad base
LACK mitochondria/Krebs cycles enzymes = obligate fermenters of glucose
what are causes of vascular lesions of the SI/LI
ischemic bowel dz
angiodysplasia
What is the presentation of intussusception
MC obstruction of kids <2 yo (spontaneous/viral infxn/rotovirus vaccine; lymphoid hyperplasia –> lead point; Peutz-Jegher) ==> Tx: contrast enema, air enema
adults: due to intraluminal mass/tumor (usually malignant) –> Tx: SRG
=segment telescopes into the immediately distal segment

How does erythema nodosum present
type of skin inflam
located in part of the fatty layers of skin
reddish, painful, tender lumps/nodule
*front of legs, below knees*

what is the outcome of acute compromise in ischemic bowel dz
mucosal & non-transmural infarct - may NOT be fatal
transmural ==> 10% mortality w/i 30 days bc full thickness necrosis (NEC - MC aquired GI in neonates can cause transmural necrosis)
worst outcome = SMA occlusion
What are characterisitics of rotovirus
MCC severe childhood diarhea & diarrheal mortality worldwide
= encapsulated dsRNA
6-24 months = most vulnerable (probably bc Ab in breast milk confer protection during 1st 6 months)
outbreak hostpital & daycare centers
enterocyte damage ==> loss of absorptive fxn & new secretion of water & electrolytes –> incomplete abs of nutrients –> osmotic diarrhea
what are diagnostic tests used for GI complaint
imaging: XR, barium, CT scan, US, angiography, CTE (best for SI)/MRE (enterography)
endoscopy: video capsule/ colonoscopy
labs: CBC, CMP, Micro, Genetics (malignancy/syndromes)
Bx: endoscopic, fine needle aspiration/core Bx, SRG, autopsy
what are types of polyps
hyperplastic
inflam
hamartomatous
adenoma
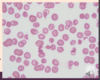
What is Abetalipoproteinemia
rare auto rec dz = inablity to assemble triglyceride-rich lipoprotein
infancy- FTT, diarrhea & steatorrhea
plasma = complete devoid of lipoprotein containing apolipoprotein B
fail to abs essential FA –> def in fat-soluble vits
lipid membrane defects –> acanthocytes in peripheral blood smear
What is the presentation of angiodysplasia
= malformed tortuous submucosal & mucosal blood vessels = dilated & thin
MC - cecum or R. colon; >60 y/o
anemia b/c slow GI bleed (= 20% of major lower GI bleeds in older pts)
chronic/intermittent/massive hemorrhage
what are the extra-intestinal manifestations of IBD
Mouth: aphthous ulcers
Eyes: uveitis
Biliary tract: sclerosing cholangitis 2.5-7.5% pt w/ UC, gallstones
Joints: migratory polyarthritis, sacroilitis, ankylosing spondylitis,
Skin: erythema nodosum, pyogerma grangrenosum
amyloidosis, finger clubbing

What are characteristics of internal cestodes
exclusively in intestinal lumen
does NOT penetrate intestinal mucosa –> NO peripheral eosinophilia
raw meat contain encysted larvae
proglottids & eggs are shed in the feces
Sxs: diarrhea, abdominal pain, nausea
3 primary species:
- Diphyllobothrium latum (fish tapeworm) ==> B12 def & megaloblastic anemia
- taenia solium (pork tapeworm)
- hymenolepis nana (dwarf tapeworm)
What is FAP
familial adenomatous polyposis
= AD disorder - pt develops numerous colorectal adenomas as TEENAGER
= somatic mutation in APC gene (75% inherited) –> may have biallelic mutation of MYH
associated w/ variety of extraintestinal manifestations - including congenital hypertrophy or the retinal prigment epithelium - detect @ birth
what is the relation of iron and Yersinia
iron enhances virulence –> stimulates systemic dissemination (occur w/ multiple transfusion)
==> greater risk for sepsis/death
non-heme related - chronic form of anemia/hemochromatosis
what is ischemic bowel dz
interconnection btn arcades (as well as collateral vessels of proximal celiac & distal pudendal/iliac circulation) allow slow, progressive blood loss
chronic - progressive hypoperfusion, acute (abrupt) compromise –> infarction of several meters of intestine

What is the morphology of colon CA
proximal colon tumors - grow as polypoid, exophytic mases –> extend along one wall of large-caliber cecum & ascending colon ==> rarely obstruct
distal colon tumors - annular lesions - make “napkin ring” constriction & lumincal narrowing –> sometimes obstruct
both invade bowel wall over time
Yersinia
geography
transmision
epidemiology
GI site
reservoir
symptoms
complications
N & central europe
pork, milk, water
clustered cases
ileum, appendix, R colon
pigs, cows, puppies, cats
Abd pain, fever, diarrhea
reactive arthritis w/ urethritis, conjunctivits, myocarditis, erythema nodosum & kidney dz
what dz’s have intraluminal digestion defects
chronic pancreatitis
CF –> pancreatitis
primary bile acid malabs (w/ defect in transepithelial transport)
IBD (w/ defect in terminal digetion & transepithelial transport)

what is hereditary nonpolyposis colorectal CA?
HNPCC = Lynch syndrome
= AD ; younger age *look for FHx*
MC syndromic form of colon CA
R-sided (ascending colon)
MSH2/MLH1 affected by DNA mismatch repair
what is the DDx for malabs diarrhea
CF
celiac
environmental enteropathy/ enteric dysfxn
autoimmune enteropathy
lactase (disaccharidase) def
abetalipoproteinemia
infectious entercolitis
what is the immune response in intestines of healthy ind
goblet cells –> mucus –> limit exposure to bacteria
antimicrobial peptides (a-defensins) by Paneth cells & IgA ==> protect luminal microbiota
innate sensing by TOL-R and NOD proteins –> dendritic cells present Ag to CD4 T cell in 2ndary lymphoid organ (peyer’s patches & mesenteric LNs) –> TGF-B & IL-10 modulate differentiation of CD4 T cells subgroups (Treg, Thelpers)–> induce enterotropic molecules
CD4 cells circulate intestinal lamina propria –> effector fx

What is a volvulus
feature of obstruction & infarction
most often = large redundant loops of sigmoid colon
(also by cecum, small bowel, stomach, transverse colon)
= rare; but seen in pts w/ mental deficits/in institutionalized facilities
can lead to gangrenous sigmoid colon –> rupture –> peritonitis & toxic megacolon
-emergency laprotomy w/ clinical signs/sxs of colonic ischemia, failed decpression & clinical features suggestive of colonic ischemia at colonoscopy

label this


what are the 4 types of diarrhea
- secretory: isotonic stool, persist during fasting
- osmotic: excess osmotic forces by luminal solutes; lactase def; stops w/ fasting
- malabs: general failure to abs nutrients; steatorrhea, stops w/ fasting
- exudative: due to inflam dz = purulent, bloody; persists w/ fasting
How do you treat pseudomembranous colitis
metronidazole & vancomycin
but prevalence of ABx resistant & hypervirulent C. diff is increasing
what is diverticular Dz
acquired pseudodiverticular outpouching of colonic mucosa & submucosa
rare < 40 yo; but common > 60 yo
asia & africa: R. side diverticula ; japan LESS common
western countries = L side
= intermittent cramping, continuous low abd discomfort, constipation, distention or sensation of never being able to completely empty rectum
can cause abscess, fistula or perforation
What is the etiology of acute obstruction to flow in ischemic bowel dz
thrombosis or embolism
severe athreosclerosis (likes to start in ostium)
AAA
cardiac mural thrombi - Afib or hypokinesia –> stasis
vasculitis
mesenteric venous thrombosis: hypercoag state, tumors, trauma, cirrhosis
what is caused by a mutation of the MTP gene
abetalipoproteinemia
gene is required for transfer of lipids to nascent apolipoprotein B polypeptide in the endoplasmic reticulum
w/o it –> lipids accumulate intacellularly

What are the therapeutic approaches to IBD
=focus on (-) proinflam cytokines, inhibit entry of cells into intestinal tissues & inhibit T-cell activation & prolif
block co-stimulatory signals that increase interaxn btn innate & adaptive cells
administer EGF
enhance tolerance
what are adenomatous polyps
MC neoplastic polyps
= intraepithelial neoplams that range from small pedunculated to large sessile
30% by age 60, M slightly more
hallmarks of epithelial dysplasia are nuclear hyperchromasia, elongation & stratification
sessile serrated lesions lack typical cytologic features of dysplasia
what syndromes may present with hamartomatous polps & what are extra-GI manifestations for each
- Cowden syndrome, Bannayan-Ruvalcaba-Riley syndrome: GI-lipomas, ganglioneuromas; benign skin tumors, benign/malignant thyroid/breast leions; NO increase in GI CA
- Cronkhite-Canada: GI: polyps in stomach, SI; abn nonpolypoid mucosa; nail atrophy, hair loss, abn skin pigmentation, cachexia and anemia
- tuberous sclerosis: mental retardation, epilepsy, facial angiofibroma, cortical tubers, renal angiomyolipoma
what is a fxnal bowel obstruction, aka paralytic ileus
=temporary disturbance of peristalsis (w/o mechanical prob)
=post-op ileus = MC etiology
also caused by metabolic probs, endocrinopathies, certain drugs
What is the etiology of chronic/hypoperfusion states in ischemic bowel dz
=non-obstructive
cardiac failure
shock
dehydration
drugs (vasoconstict) - cocaine
what are histological factors of Peutz-Jeghers syndrome
arborizing network of CT, Sm M, lamina propria & glands lined by normal appearing intestinal epithelium

what is the presentation of guillain-barre syndrome
demyelinating polyneuropathy
paresthesias in hands & feet
M weakness (start in legs and ascend)
severe resp M weakness
absent/depressed deep tendon reflexes

What is the function of APC
= one of tumor suppressors
degrade B-catenin –> downreg- growth promoting signaling paths
APC is a component of WNT signaling path –> major role in controlling cellular growth & differentiation during embryonic development
BOTH copies must be lost for adenoma to form
defect = b-catenin accumulate –> form complex w/ DNA binding factors TCF –> activate myc and cyclin D1 –> proliferate

What are characterisitics of giardia lamblia
MC parasitic pathogen in human; spread fecally contaminated water or food
cysts resistant to chlorine
flagellate protozoan decrease expression of brush border enzymes, including lactase
secretory IgA and mucosal IL-6 responses -important for clearance
= continuous modification of major surface Ag
Trophozoites = pear shape w/ 2 equal size nuclei
secretions damage brush border = malabs
How do you diagnose celiac dz
IgA Ab tTG or endomysial = sensitive & specific (95%)
tTG Ab = recommended single serologic test for celiac screening
test for gliadin Ab NOT recommended bc low sensitivity/specificity
intraepithelial lymphocytes & villous atrophy in histology not specifi, so combo of serolgy and histolgy = most specific dx
What is celiac dz
aka celiac sprue/ gluten-sensitive enteropathy
gluten (wheat, rye, barley) –> immune mediated enteropathy in genetically predisposed pts
autoimmunity arises from a combo of inheritance of susceptiblity of genes –> contribute to breakdown of self-tolerance, environmental triggers (infxn/tissue damage) –> activation of self-reactive lymphocytes
what are virulence factors due to for C. jejuni
motility
adherece
toxin production
invasion (dysentery)

Differentiate gastroschisis & omphalocele
gastroschisis: intestines protrude thru abd wall defect; but not covered by membrane
omphalocele: abd viscera herniate into base of umbilicus; covered by membrane

which dz’s have a defect of both terminal digestion and transepithelial transport
celiac dz
environmental enteropathy
autoimmune enteropathy
viral/bacteral/parasitic gasteroenteritis

what are the earliest lesions of crohns dz
& what are other morphological features
aphthous ulcers
may progress –> multiple lesions often coalesce into elongated, serpentine ulcers along the axis of the bowel
common: edema & loss of normal mucosal folds
ulcerations w/ sparing of interspersed mucosa –> irregular, cobblestone appearance
develop fissures & may become fistula tracts/perforation
which colon CA etiologies lead to tubular, villous, typical adenoCA
FAP = AD
Sporadic Colon CA (70-80%) - predom L side
both = APC/WNT pathway
What is Peutz-Jeghers syndrome
AD syndrome- LOF in STK11 50% pt
(10-15 yo)
multiple GI hamartomatous polyps & mucocutaneous hyperpigmentation
MC: SI (but can occur in stomach, colon, and less freq bladder/lungs)
intusussusception often fatal
pigmented macles; risk for colon, breast, lung, pancreatic and thyroid CA
Shigellosis
geography
transmision
epidemiology
GI site
reservoir
symptoms
complications
worldwide, endemic developing countries (poor sanitation)
fecal-oral, food, water
children, migrant workers, travelers, nursing homes
L colon, ileum
humans
MCC: bloody diarrhea - worldwide; death (limited to < 5 yo)
reactive arthritis, urethritis, conjunctivitis (HLA-B27 men 20-40 yo), HUS, toxic megacolon
what are the macroscopic differences btn crohn’s & UC
bowel region
distribution
strictures?
wall appearance
what is the morphology for ischemic bowel dz
lesions = patchy
mucosa = hemorrhagic/ulcerated
transmural infarct –> large portion affected; sharp line btn infarct & healthy tissue
chronic: fibrous scarring of lamina propria; pseudomembrane resembles c. diff
what is the most important characteristic that correlates w/ malignancy in polyps
SIZE
where does environmental enteric dysfxn present? ( aka environmental enteropathy, tropical enteropathy, tropical sprue)
how does it present
poor sanitation/hygiene
sub-saharan africa (zambia), aboriginal pop in N. australia (travel or live there)
=malabs, malnutrition & stunted growth
What is IBD
what is the epidemiology
=chronic; inappropriate mucosal immune response to normal gut flora = crohns & UC
teens/ early 20’s (UC slightly more F & 2nd peak 60s-70s)
white, ashkenazi jews
n. america, europe, australia
what are watershed zones?
most vulnerable for ischemic bowel dz
splenic flexure btn SMA & IMA (= marginal A)
sigmoid colon & rectum - IMA, pudendal & iliac A circulation ends
who is at risk for salmonella infxns
CA
immunosuppression
EtOH
CV
sickle cell (osteomyletis)
hemolytica anemia
what is the pathogenesis of celiac dz
triggered by ingestion of gluten –> gliadin (alc soluble fraction) = most of dz-producing component (resistant to breakdown by proteases)
innate response= induce IL-15 –> (+) CD8 - express NKG2D –> attack enterocytes w/ MIC-A –> damage increases chance of gliadin to enter lamina propria –> deaminated by tTG
–> interact w/ HLA-DQ2 & HLA-DQ8 –> (+) adaptive response –> CD4 make cytokines –> tissue damage

how is IBS defined
what pop does it present in most
=chronic relapsing abd pain, bloating & changes in bowel habits w/o obvious gross/histological features
3 types: diarrhea predom, constipation predom & mixed
pathogenesis = psychologic stressors, diet, gut microbiome, abn GI motility & increased enteric sensory response
Female, 20-40 yo, high income countries
E. coli
geography
transmision
epidemiology
GI site
reservoir
symptoms
complications

what are characterisitcs of inflammatory polyps
may be part of solitary rectal ulcer syndrome (SRUS)
triad = rectal bleeding, mucus discharge, inflam lesions on anterior rectal wall
–> chronic cycles of injury/healing
histology: mixed inflam infiltrates, erosion & epithelial hyperplasia w/ prolapse induced lamina propria firbomuscular hyperplasia
what are causes of GI obstruction (which are most often in the SI, bc of the narrow lumen)
80%:
- hernia = MC worldwide
- adhesions
- volvulus
- intussuseption
tumors, infarctions, other strictures = 10-15%

how does dermatis herpetiformis present
microabscess- papillae
subepidermal blisters
granular IgA deposits
(associated w/ celiacs)
What is the morphology of salmonella
peyer patches in the terminal ileum - enlarge into sharply delinated, plateau-like elvation
enlarge mesenteric LN
acute/chronic inflam cell recruited to lamina propria –> necrotic debris & overlying mucosal ulcers along the axis of the ileum (may perforate)
spleen = enlarged & soft w/ uniform pale red pulp & obliterated follicular markings
typhoid nodules: focal hepatocyte necrosis w/ macrophage aggregates
What is the morphology of pseudomembranus colitis
associated w/ C.diff
pseudomembrane - made up of an adherent layer of inflam cells & debris are non specific & may also be present in ischemia/necrotizing infxn
histopath = damaged crypts - distended by mucopurulent exudate that form an eruption-like volcano –> form membrane

how does celiac dz present in adults
Females (autoimmune)
30-60 yo
silent or symptomatic
chronic diarrhea, bloating, chronic fatigue, anemia (chronic iron and vitamin malabsorption)
Dermatitis herpetiformis: itchy, blistering skin lesion (10%)
How does celiac present in children
M=F
6-24 months: irritable, abd distention, chronic diarrhea, FTT, wt. loss, M. loss
older = abd pain, N/V, bloating, constipation
extraintestinal: arthritis/joint pain, aphthous ulcers, stomatitis, anemia, delayed puberty, short stature
what is malabsorption
what is the MC malabs disorder
= defective abs of fats, h2o-soluble vits, proteins, carbs, electrolytes, minerals & water
hallmark = steatorrhea -excessive fecal fat -bulky, frothy, greasy, yellow, clay colored stool
pancreatic insufficiency, celiac dz & crohns dz MC chronic malabs prob in USA
what are microscopic differences of crohns & UC
inflam:
pseudopolyps
ulcers
lymphoid rn
fibrosis
serositis
granulomas
fistulae/sinuses

what are characteristic of CF
= inherited; dysfxn ion transport –> affect fluid secretions in exocrine glands & epithelial lining of resp, GI, reproductive tract
=thick secrtions obstruct organs:
- infant: meconium ileus
- chronic lung dz 2ndary to recurrent infxn
- pancreatic insufficiency - 85-90 % pt; severe –> completely plugged glands –> atrophy of gland & fibrosis==> impair fat abs (avitaminosis A –> dermatitis, glossitis, squamous metaplasia)
- steatorrhea
- malnutrition
- hepatic cirrhosis
- intestinal obstuction
- male infertility
what are the chances of getting colorectal adenoCA in pts w/ untreated FAP
100%- before 30 & nearly all by age 50
common site = ampulla of vater & stomach
adenomatous polyps = known precursors to majority of colorectal adenoCA
adenoCA of colon = MC malignancy of GI (10% CA deaths worldwide)
what is indeterminate colitis
unable to make definitive dx bc overlap of UC and crohns
serologic studies useful in finding overlapping features (75% UC - antineutrophil cytoplasmic Ab & only 11% crohns)


