Cell and Electrical Signalling, including immune system and muscles (4) + (5) Flashcards
(105 cards)
what is the autonomic nervous system
the part of the peripheral nervous system associated with involuntary responses and involuntary muscle movement
give two examples of auto-immune disease
DIABETES TYPE 1
MULTIPLE SCLEROSIS
give a description of the structure: motor neurone
a nerve cell that carries impulses away from the CNS to an effector eg. muscle or gland

give a description of the structure: Schwann cell
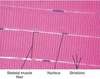
glial cells in the peripheral nervous system that produce the myelin sheath around neuronal axons

what is a synapse (1 mark)
a junction between two nerve cells, consisting of a minute gap across which impulses pass by diffusion of a neurotransmitter

what is the nervous system
a system for coordination and control in animals, along with the endocrine system

which specialised cells make up the nervous system + how does this process occur (2 marks)
stimuli are received from the internal/external environment by modified nerve cells called receptors in the sense organs or internal receptors
receptors convert the energy of the stimuli into electrical energy, a process called transduction
the electrical energy is transmitted as electrical impulses along a sequence of neurones/nerve cells- SENSORY NEURONE → INTER/RELAY NEURONE (CNS) → MOTOR NEURONE
motor neurones connect to effectors that carry out a response

outline the NS pathway
STIMULUS ⇒ RECEPTOR → SENSORY NEURONE- dendrites, dendron, soma, axon, axon terminals ⇒ INTERNEURONE (CNS) using relay neurone⇒ MOTOR NEURONE- dendrites*, axon, axon terminals → EFFECTOR (MUSCLE OR GLAND) → RESPONSE
*containing soma; motor neurone have soma in CNS, sensory neurones have it near CNS

what does the functioning of the NS require
an electrical potential difference across the plasma membrane; a membrane potential

how do the characteristics of a SENSORY neurone, INTERNEURONE and MOTOR neurone differ
Sensory neurone: from the effector a dendrite leads to the cell body and away via an axon
Interneurone: very short dendrites lead to the cell body and away via a very short axon, non-myelinated
Motor neurone: cell body with little dendrites branching off, a myelinated axon takes the electrical impulse to the effector

how is a membrane potential set up (4 marks)
- SODIUM/POTASSIUM PUMP: a transmembrane protein pump requiring ATP. It pumps 3 Na+ out of the cell for every 2 K+ pumped into the cell. Therefore there is more Na+ outside and K+ inside, polarising the cell to a membrane potential of -70mV.
- SODIUM CHANNELS ARE CLOSED (2nd pump)
- POTASSIUM CHANNELS ARE LEAKING (3rd pump) K+ does not all diffuse out of the cell because it is attracted to the negative region inside the cell.

what is a dendrite (2 marks)
(same as dendron) a short branched extension of a nerve cell, along which impulses received from other nerve cells at synapses are transmitted to the cell body

what are glial cells
non-neuronal cells that maintain homeostasis, form myelin and provide support and protection for neurones in the CNS and PNS eg. SCHWANN CELLS
what do reflex actions involve (1 mark)
+ what is their purpose (3 marks)
They are responses that do not involve conscious thought; involve involuntary movement and a reflex arc.
- response to danger
- to avoid damage to the body
- to maintain balance

what is the pathway for a reflex arc
RECEPTOR ⇒ SENSORY NEURONE ⇒ RELAY NEURONE in spinal cord or unconscious part of brain ⇒ MOTOR NEURONE ⇒ EFFECTOR
in a monosynaptic reflex, the sensory neurone connects directly to a motor neurone eg. the knee jerk reflex

give an example of a reflex arc and its purpose (3 marks)
KNEE JERK REFLEX

used by body to maintain balance and posture, allowing the person to stand with little effort or conscious thought
used by doctors to detect nervous problems eg. cerebellar disease
INTERNEURONES: compare structure and position in NS
- same structural components as motor and sensory neurones- dendrites, soma, axon, synaptic endings NO MYELIN SHEATH- no need for accelerated speed of conduction along axon/dendron bc they do not extend across long distances*
- found entirely in CNS and tf do not need extended axons or dendrons*

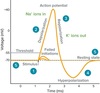
what is an action potential
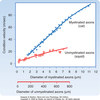
a momentary change in the membrane potential caused by a transient change in the membrane’s permeability to sodium and potassium ions
can be observed with an oscilloscope that monitors the electrical potential or voltage, recorded by a microelectrode
what is a membrane potential (3 marks)
In the neurone it is a resting potential, which is an electrical potential difference across the plasma membrane, typically between -60mV and -80mV. The inside is negative relative to the outside, the membrane is polarised

what causes an action potential (3 marks)
- It is initiated when a neurone or muscle cell (an excitable cell) is depolarised to threshold value (approx. -50mV)
- Initiated by a change in permeability of the membrane to Na+ and K+ ions; Na+ ions flow into the cell.
what happens after depolarisation (4 marks)
- During the AP, the inside of the cell becomes positively charged relative to the outside.
- Repolarisation/downstroke is caused by a change in the membrane permeability to Na+ and K+ ions; potassium ions flow out of the cell.
- The cell becomes negatively charged inside relative to the outside again.

what occurs at the end of an action potential (2 marks)
The membrane becomes more negative on the inside than at a resting potential; HYPERPOLARISATION. It is a necessary refractory period.

what is a voltage-gated ion channel?
Nerve axons contain two types of channels: Na+ specific and K+ specific, that are opened and closed by voltage dependent gates.
These enable neurones to produce action potentials because these are contained in their membranes.
what is a Node of Ranvier (1 mark)
a gap in the myelin sheath of a nerve, between adjacent Schwann cells