Cardiovascular Flashcards
LO 1.1 Describe the factors influencing the exchange of substances between the blood in capillaries and the surrounding tissues
Area available for exchange - Determined by the Capillary Density (Capillaries per unit volume). Is highest in tissues that are most metabolically active. Note that not all capillaries are always perused.
Diffusion Resistance – The difficulty of movement through the barrier A major component of diffusion resistance is the distance over which diffusion must occur, the path length.
The Concentration gradient - Helps drive diffusion,This gradient does depend on the concentration of substances in the blood, but the more important variable is the flow of blood through the capillary. Unless blood is supplied at an appropriate rate, the gradients driving exchange will dissipate.
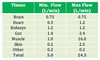
LO 1.3 List typical blood flows in ml/min/organ for major organs of the body, including the brain, kidneys, heart muscle, gut, skeletal muscle and skin, including both minimum levels and maximum levels.
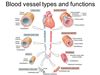
LO 1.5 Describe the major functional components of the circulation
A Pump - The Heart Distribution
Vessels - The Arteries
Flow Control - Cardiac output must be distributed appropriately by restricting flow to those parts of the body that are easy to perfuse, so as to drive blood to parts that are not so easy to perfuse. Flow control is via resistance vessels, the arterioles and pre-capillary sphincters
Capacitance - Capacitance is the ability to cope with changes in the cardiac output. This is a store of blood that can be called upon to cope with temporary imbalances between the amount of blood returning to the heart and the amount that it is required to pump out. This store is the veins.
LO 1.6 What is the typical blood volume in the body and describe the distribution of blood volume over the major parts of the circulation.
At rest, the blood volume is about 5 Litres
11% - Arteries and Arterioles
5% - Capillaries
17% - Heart and Lungs
67% - Veins
LO 1.7 Describe the different types of vessel, and be able to label the layers of each
LO 2.2 Describe in general terms the properties of cardiac muscle that allow the heart to operate as a pump. How is it organised to best pump blood?
- Striations
- Branching
- Centrally positioned nuclei (1 or 2 per cell)
- Intercalated discs (for electrical and mechanical coupling with adjacent cells)
- Adherens-type junctions (to anchor cells and provide anchorage for actin)
- Gap junctions (for electrical coupling)
- In contrast with skeletal muscle, the T tubules of cardiac muscle are inline with the Z bands and not with the A-I band junction
LO 2.3 Define the terms Systole and Diastole, how long do each last?
Systole is the period when the myocardium is contracting, initiated by the SAN and lasting ~280ms.
Diastole is the relaxation in-between contractions, lasting about 700ms.
LO 2.4 What is the Spread of Excitation in Systole
- The SA node fires an action potential, which spreads over the atria causing atrial systole. The AP reaches the AV node, where it is delayed for about 120ms.
- From the AV node, excitation spreads down the septum between the ventricles
- Excitation spreads from inner (endocardial) to outer (epicardial) surface
- Ventricle contracts from the apex up, forcing blood towards the outflow valves.
LO 2.5 Describe the main differences between the right and left heart
The left side of the heart has a thicker myocardium, as it must generate the force to get blood around the entire body compared to the right side that must only get it around the lungs.
The left heart has the mitral valve whereas the right has the tricuspid valve.
The right side of the heart has the pacemaker, the SA node.
LO 2.6 Describe the sequence of pressure and volume changes in the atria and ventricles over a complete cardiac cycle in the normal individual. What is the way that ventricles contract in the heart?

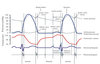
LO 2.8 Explain the Origin of the 1st and 2nd Heart Sounds (also 3rd and 4th)
First Sound - As the AV valves closes, oscillations are induced in a variety of structures, producing a mixed sound with a crescendo-descendo quality – ‘lup’
Second Sound - As the semi-lunar valves close oscillations are induced in other structures, including the column of blood in the arteries. This produces the sound of shorter duration, higher frequency and lower intensity than the first – ‘dup’
A 3rd sound may be heard early in diastole, associated with heart failure or athletes.
A 4th is sometimes associated with atrial contraction. In exercise, turbulent flow generates ‘murmurs’ in normal individuals, but at rest murmurs are associated with disturbed flow, e.g. through a narrowed valve or back flow through an incompetent valve.
LO 3.1 Describe the frequency and most common types of congenital malformation of the heart and great vessels
Congenital heart defects are common, with an incidence of 6-8 per 1,000 births.
The most common heart defects are Ventricular Septal Defects (VSD), followed by Atrial Septal Defects (ASD).
LO 3.2 Discuss Atrial Septal Defects
An ASD is an opening in the septum between the two atria, which persists following birth. They have an incidence of 67 in 100,000 live births. The foramen ovale exists to prenatally permit right -> left shunting of oxygenated blood and is designed to close promptly after birth.Failure of it to close, allows blood to continue to flow between the two atria postnatally. Because left atrial pressure > right atrial pressure, flow will be mainly from left -> right, meaning no mixing of deoxygenated blood with the oxygenated blood being pumped around the circulation. ASDs can occur almost anywhere along the septum, but the most common site is the foramen ovale (Ostium secundum ASD). An ostium primum ASD occurs at the inferior part of the septum, and is less common.
LO 3.2 Discuss Patent Foramen Ovale
PFOs are not a true ASD. PFOs may be present in ~20% of the population and are generally clinically silent, since the higher left atrial pressure causes functional closure of the flap valve. A PFO may however be the route by which a venous embolism reaches the systemic circulation if pressure on the right side of the heart increases even transiently. This is called a paradoxical embolism.
LO 3.2 Discuss Ventricular Septal Defect
VSDs are an opening in the Interventricular Septum. This most commonly occurs in the membranous portion of the septum, but can occur at any point. Since left ventricular pressure is much > than right, blood will flow left to right.
LO 3.2 Discuss Patent Ductus Arteriosus
The Ductus Arteriosus is a vessel that exists in the foetus to shunt blood from the pulmonary artery to the aorta before the lungs are functioning. This vessel should close shortly after birth as the pressure in the pulmonary artery drops following perfusion of the lungs. Failure to close leads to a PDA. Blood flow through a PDA will be from the aorta to pulmonary artery after birth (High to Low pressure). A Mechanical Murmur is heart constantly throughout systole/diastole, as pressure in the aorta is always greater than in the pulmonary artery. Although left to right shunting of blood does not cause cyanosis it can be problematic later on if untreated, with the extent of the problems depending on the degree of shunting. Chronic left to right shunting can lead to vascular remodelling of the pulmonary circulation and an increase in pulmonary resistance. If the resistance of the pulmonary circulation increases beyond that of the systemic circulation the shunt with reverse direction as pressures on the right side of the heart increase (Eisenmenger Syndrome).
LO 3.2 Discuss Coarctation of the Aorta
Coarctation of the Aorta is a narrowing of the aortic lumen in the region of the ligamemtum arteriosum (former ductus arteriosus). The narrowing of the aorta increases the afterload on the left ventricle and can lead to left ventricular hypertrophy. Because the vessels to the head and upper limbs usually emerge proximal to the Coarctation, the blood supply to these regions is not compromised. However blood flow to the rest of the body is reduced. The extent of the symptoms depends on the severity of the Coarctation. In very severe cases, an infant may present with symptoms of heart failure shortly after birth. In mild cases, the defect may be detected in adult life. Femoral pulses will be weak and delayed, with upper body hypertension.
LO 3.3 Discuss Tetralogy of Fallot
The Tetralogy of Fallot is a group of 4 lesions occurring together as a result of a single developmental defect placing the outflow portion of the interventricular septum too far in the anterior and cephalad directions. The four abnormalities are: - VSD - Overriding Aorta - Pulmonary Stenosis (variable degree) - Right Ventricular Hypertrophy (variable degree) Pulmonary stenosis causes persistence of the foetal right ventricular hypertrophy, as the right ventricle must operate at a higher pressure to pump blood through the pulmonary artery. The increased pressure on the right side of the heart, along with the VSD and overriding aorta allow right to left shunting and therefore the mix of deoxygenated blood with the oxygenated blood going to the systemic circulation, resulting in cyanosis. The magnitude of the shunt and level of severity depends on the severity of the pulmonary stenosis. Affected individuals may present with cyanosis in infancy, but mild cases can present in adulthood.
LO 3.3 Discuss Tricuspid Atresia
Tricuspid Atresia is the lack of development of the tricuspid valve. This leaves no inlet to the right ventricle. There must be a complete Right to Left shunt of all blood returning to the right atrium (ASD or PFO) and a VSD or PDA to allow blood to flow to the lungs.
LO 3.3 Discuss Transposition of the Great Arteries
Results in two unconnected parallel circulations instead of two in series. In this defect, the right ventricle is connected to the aorta and the left ventricle to the pulmonary trunk. This condition is not compatible with life after birth, unless a shunt exists to allow the two circulations to communicate. A shunt must be maintained or created immediately following birth to sustain life until surgical correction can be made. The ductus arteriosus can be maintained patent and/or an atrial septal defect formed.
LO 3.3 Discuss Hypoplastic Left Heart
In some cases the left ventricle and ascending aorta fail to develop properly resulting in a condition called Hypoplastic left heart. A PFO or ASD are also present and blood supply to the systemic circulation is via a PDA. Without surgical correction this is lethal.
LO 4.1 Understand the Anatomical and Pharmacological divisions of the autonomic nervous system (ANS)
The ANS is comprised of a series of 2 neurones – one pre-ganglionic and one post-ganglionic. The ganglion is the collection of cell bodies in the PNS . 1 cell has its cell body in the CNS. 1 cell has its cell body in the PNS.
Sympathetic Nervous System
Thoraco-Lumbar Outflow Nerve fibres have cell bodies in all 12 thoracic sections and the first 2 lumbar sections. Short pre-ganglionic nerve fibre – Long post-ganglionic nerve fibre May synapse at same level as origin (paravertebral origin), may synapse at different level to origin or may not synapse in paravertebral chain Pre-ganglionic neurones are cholinergenic (Ach) (Nicotinic) Post-ganglionic neurones express nicotinic receptors
Post-ganglionic neurones are noradrenergic (NA) (Two classes of adrenoceptors A(1 & 2) and B(1 & 2) Exception some synapses are cholinergic: perspiration and ejaculation pathways
Parasympathetic Nervous
System Cranio-Sacral Outflow Long pre-ganglionic nerve fibre – Short post-ganglionic nerve fibre Pre-ganglionic neurones are cholinergic (Nicotinic) Post-ganglionic neurones express nicotinic receptors Post-ganglionic neurones are cholinergic (Muscarinic, G-Protein coupled)
LO 4. 3 State the action of the sympathetic nervous system on blood vessels in different organs
The sympathetic branch of the autonomic nervous system innervates the smooth muscle in the walls of arteries, arterioles and veins. Except in specialised vessels (e.g. erectile tissue with parasympathetic innervation), sympathetic activity causes constriction of arterioles, vasoconstriction, via 1 adrenoceptors. There is constant activity of the sympathetic nervous symptom – Vasomotor Tone. This tone varies from organ to organ. In skin for example, vasomotor tone is high, so arterioles, pre-capillary sphincters and arterio-venous anastomoses are generally shut down. Variation in sympathetic outflow produces large changes in skin blood for, for thermoregulation. In skeletal muscles, vasomotor tone is high at rest, but in exercise is antagonised by vasodilator metabolites. In the gut, vasomotor activity is high until a meal is consumed, when various vasodilators produced in the gut tissue antagonise it. Circulation to the brain is virtually unaffected by sympathetic activity. The interplay between sympathetic vasoconstrictor tone and the action of vasodilator substances is the principal means by which the distribution of flow around the CVS is controlled. Vascular tone in the skin and skeletal muscle is also a mechanism for controlling the total peripheral resistance. Sympathetic outflow to blood vessels is controlled from the brainstem, via the ‘vasomotor’ centres in the medulla oblongata.
LO 4.4 State the action of the sympathetic and parasympathetic system upon heart rate and force of contraction
Both the parasympathetic and sympathetic branches of the ANS, which innervate both the SA and AV nodes, affect heart rate. Parasympathetic activity slows the heart rate and sympathetic speeds it up. Both are controlled by centres in the medulla oblongata, which themselves receive information from the Baroreceptors, which are located in the arch of the aorta and carotid sinuses. There is a basal activity of both systems at rest, but if all autonomic inputs are pharmacologically blocked, the intrinsic heart rate is ~100bpm. The normal resting HR of ~60bpm is produced because the parasympathetic dominates the sympathetic at rest. Initial increases in heart rate are brought about by reduction in parasympathetic outflow. Increasing Sympathetic outflow makes further increases. Sympathetic nerve fibres also innervate ventricular cardiac myocytes, increasing the force of contraction and cardiac output. Sympathetic – NA - B1 Receptors Parasympathetic – Ach – M2 Receptors Adrenaline from the adrenal medulla can also act on the heart
LO 4.2 State in broad terms the distribution of different types of adrenoceptor around the body
Organ
Sympathetic Effect
Receptor
Parasympathetic Effect
Receptor
Heart
Increase rate/force of contraction
b1
Decrease rate
M2
Airways
Relax
b2
Contract
M3
Pupil
Dilation
a1
Contraction
M3
Sweat Glands
Localised secretion
General Secretion
a1
M3
No effect
LO 5.1 Define the terms ‘Flow’ and ‘Velocity’ with respect to the movement of fluids through tubes and state the relationship between them
Flow – The volume of fluid passing a given point per unit time Flow=Volume/Time Velocity – Rate of movement of fluid particles along the tube Velocity=Distance/Time
LO 5.2 Describe what is meant by ‘Laminar’ and ‘Turbulent’ flow
Laminar Flow In laminar flow, there is a gradient of velocity from the middle to the edge of the vessel. Velocity is highest in the centre, and fluid is stationary at the edge. The flow in most blood vessels is laminar. Turbulent Flow As the mean velocity increases, flow eventually becomes turbulent. The velocity gradient breaks down as layers of fluid try to move over each other faster than physics will allow. The fluid tumbles over, greatly increasing flow resistance.
LO 5.3 Describe what is meant by viscosity, and the effect of viscosity on flow
Viscosity – The extent to which fluid layers resist sliding over one another. The higher the viscosity, the slower the central layers will flow, and the lower the average velocity. In a low viscosity fluid, the difference between the centre and edge is large, and in a high viscosity fluid the difference is smaller.
LO 5.4 Describe the effects of changes in tube diameter on flow rate
Viscosity determines the slope of the gradient of velocity. At a constant gradient, the wider the tube the faster the middle layers move, so mean velocity it proportional to the cross sectional area of the tube.
LO 5.5 Define the term ‘resistance’ to flow and state the factors which affect flow resistance, describing the relationship between pressure, resistance and flow
The flow of fluid along tubes is comparable to the flow of electricity along wires (V = IR) Pressure=Flow × Resistance Resistance=Pressure/Flow Resistance increases as viscosity increases. The ‘thicker’ the blood, the harder it is to push around blood vessels Resistance decreases with the fourth power of the radius. Because of the 4th Power, a very small change in the tube’s radius makes a very big change to resistance. It is much more difficult to push blood through small vessels than big ones If flow is fixed: The higher the resistance, the greater the pressure change from one end of the vessel to the other If pressure is fixed: The higher the resistance, the lower the flow
LO 5.6 Describe the effects of combining flow resistances in series and in parallel
Resistances in blood vessels combine just like electrical resistances. For vessels in series, resistances add together. For vessels in parallel, the effective resistance is lower, as there is more than one path for the current to flow down. E.g. Two vessles in series: The resistance of one of the vessels in series is half of the original, as the blood has two paths Re=(R1×R2)/(R1+R2)
LO 5.7 Describe the pattern of flow resistance and pressure over the systemic circulation
Over the whole circulation, flow is the same at all points Arteries are low resistance Thus Pressure drop over arteries is small Arterioles are high resistance So Pressure drop over arterioles is large Venules and veins are low resistance And so Pressure drop over venules and veins is small The pressure within arteries is high because of the high resistance of the arterioles. It is difficult to push blood into them, therefore pressure increases. For a given total flow, the higher the resistance of the arterioles the higher the arterial pressure. If the heart pumps more blood and the resistance of arterioles remains the same, the arterial pressure will rise.
LO 5.8 Describe how the distensibility of blood vessels affects the relationship between flow and pressure
Blood vessels have distensible walls, and the pressure within the vessel generates a transmural pressure across the wall. This stretches the vessel. As the vessel stretches, the diameter of the lumen increases, so resistance falls and flow increases. So the higher the pressure in a vessel, the easier it is for blood to flow through it. As the pressure within a distensible vessel falls, the walls eventually collapse, and blood flow ceases before the driving pressure falls to zero.
LO 5.9 Describe how the distensibility of blood vessels produces the property of capacitance
As vessels widen with increasing pressure, more blood transiently flows in than out. This allows distensible vessels to ‘store’ blood – They have capacitance. Veins are the most distensible vessel, with 67% of the blood in them at rest.
LO 5.10 Define the terms ‘Systolic’ and ‘Diastolic’ arterial pressure and ‘Pulse Pressure’
Systolic Pressure o The maximum arterial pressure o Typically 120 mmHg o Affected by: • How hard the heart pumps • Total Peripheral Resistance • Compliance (‘stretchiness’) of the arteries Diastolic Pressure o The minimum arterial pressure o Typically 80 mmHg o Affected by: • Systolic Pressure • Total Peripheral Resistance Pulse Pressure o The difference between Systolic and Diastolic Pressure o Typically 40 mmHg Average Pressure Diastolic plus 1/3rd pulse pressure (Systole is shorter than diastole)
LO 5.11 Define the term ‘Total Peripheral Resistance’
Total Peripheral Resistance – The sum of the resistance of all of the peripheral vasculature in the systemic circulation.
LO 5.12 Describe how the elastic nature of arteries acts to reduce arterial pressure fluctuation between systole and diastole
If arteries had rigid walls, the pressure in them would rise enough in systole to force the whole stroke volume through the total peripheral resistance, and fall to zero in diastole. But arteries have distensible walls, allowing them to stretch in systole. More blood flows in than out, so pressure does not rise so much. The arteries recoil in diastole and flow continues through the arterioles.
LO5.14 Describe the pulse wave
Contraction of the ventricles generates a pulse wave, which propagates along the arteries faster than blood. This is felt at a variety of locations where arteries come close to the surface and can be pushed against a reasonably hard surface.
LO 5.15 Describe the role of arterioles as resistance vessels
Arterioles control blood flow to tissues by variable flow restriction. Their walls contain much smooth muscle, and it’s state of contraction determines lumen diameter and therefore flow resistance (see above). Vasoconstriction leads to Decrease in Flow Vasodilation leads to Increase in flow
LO 5.16 Describe what is meant by ‘vasomotor tone’ and list the main factors which affect it
Muscles do not actively relax, so except under maximum flow conditions there must always be some vasoconstriction. Vasodilation is therefore reduces vasoconstriction. This continuous contraction of the muscle is known as vasomotor tone. Vasomotor tone is mainly produced by the sympathetic branch of the ANS (1 adrenergic receptors). This tone is antagonised by vasodilator factors, and the actual resistance is determined by a balance between the two.
LO 5.17 Describe how ‘vasodilator metabolites’ modify vasomotor activity to permit local control of blood flow
Metabolically active tissues produce vasodilator metabolites. E.g: o H+ o K+ o Adenosine These metabolites cause the relaxation of local smooth muscle, lowering resistance and increasing blood flow.
LO 5.18 Describe reactive hyperaemia
If the circulation to an organ or limb is cut off for a minute or two, then restored, a large amount of blood enters after a period of no blood flow. As the organ/limb has continued metabolising and producing vasodilators during the period of no circulation, with no blood flow to remove them, when circulation is restored, the local arterioles dilate maximally and blood flow is very high.
LO 5.19 Describe auto-regulation
At most levels of metabolic activity, most organs can automatically take the blood flow they need so as long as the pressure in the arteries supplying them is kept within a certain range.
LO 5.20 Define the terms ‘central venous pressure’ and ‘venous return’
Central Venous Pressure – The pressure in the great veins supplying the heart. Venous Return – The rate of flow of blood back to the heart. Limits cardiac output.
LO 6.1 Describe the effects of changes in total peripheral resistance, at a given cardiac output, on arterial and venous pressures
TPR falls, arterial pressure will fall, and venous pressure will rise. TPR rises, arterial pressure will rise, and venous pressure will fall.
LO 6.2 Describe the effects of changes in cardiac output, at a given total peripheral resistance, on arterial and venous pressure
CO falls, arterial pressure falls and venous pressure will rise. CO rises, arterial pressure will rise and venous pressure will fall.
LO 6.3 Explain how the cardiovascular system will be stable if the cardiac output is increased by rises in venous pressure and falls in arterial pressure and vice versa
The system is demand led and stable, the TPR changes in response to metabolic demand, altering arterial and venous pressure and the CO changes in response to this.
LO 6.4 Define the terms stroke volume, end diastolic volume and end systolic volume
End Diastolic Volume The volume of blood in the ventricle at the end of diastole End Systolic Volume The volume of blood in the ventricle at the end of Systole Stroke Volume The difference between end diastolic/systolic volume
LO 6.5 Describe the factor’s which determine how much the ventricles fill during diastole, and draw a graph of the relationship between end-diastolic volume in the left ventricle and venous pressure
In diastole, the ventricle is isolated from the arteries, and connected to the veins. Therefore the amount the ventricle fills depends on the venous pressure. The ventricle fills until the walls stretch until it has filled with enough blood to equal the venous pressure. The higher the venous pressure, the more the heart fills in diastole. This relationship can be plotted on a graph known as the ventricular compliance curve.
LO 6.6 Definine the terms ‘pre-load’ and ‘after-load’ on the ventricular myocardium
Pre-Load is the end diastolic stretch of the myocardium. It is determined by venous pressure (see above). After-load is the force necessary to expel blood into the arteries.
LO 6.7 Describe how changes in end-diastolic volume affect the force of contraction of the myocardium during the following systole
The more the heart fills, the harder it contracts (up to a limit). The harder it contracts, the bigger the stroke volume. This is Starling’s Law of heart, and can summarised simply – More in means More out.
LO 6.8 Draw a graph of the relationship between venous pressure and stroke volume at a constant after-load (The Starling Curve)
The more the heart fills due to increased venous pressure, the harder it contracts (at a constant after load). There is however a limit, when the heart becomes over-filled and the myocardium is overstretched.
LO 6.9 Define the term ‘contractility’ and describe, in principle, how the Starling curve is changed by factors which increase the contractility of the ventricular myocardium
The gradient is the contractility of the heart. Contractility is not the force of contraction of the heart, rather the stroke volume you get for a given venous pressure. Contractility is increased by sympathetic activity. Sympathetic activity therefore makes the heart more susceptible to venous pressure. Autonomic outflow to the heart is controlled by signals from the baroreceptors, which are located in the arch of the aorta and the carotid sinus. The baroreceptors sense arterial pressure and send signals to the medulla, which controls the heart.
LO 6.10 State in words the effect of increases and decreases in venous return (and therefore venous pressure) on cardiac output
If venous pressure rises, cardiac output rises (increased pre-load). If venous pressure falls, cardiac output falls (decreased pre-load). If arterial pressure rises, cardiac output falls (increased afterload). If arterial pressure falls, cardiac output rises (decreased afterload).
LO 6.11 Discuss the response of the cardiovascular system to eating a meal
Increased activity of the gut leads to the release of metabolites and local vasodilation. The total peripheral resistance falls, causing the arterial pressure to fall and the venous pressure to rise. The rise in venous pressure causes a rise in cardiac output. The fall in arterial pressure triggers a rise in heart rate and cardiac output. The extra pumping of the heart reduces venous pressure The extra pumping of the heart raises arterial pressure Demand met – System Stable
LO 6.12 Discuss the response of the cardiovascular system to exercise
Enormous increase in demand ‘Muscle pumping’ forces extra blood back to the heart With no other changes, venous pressure would rise greatly, and arterial pressure would fall greatly. These changes may be too big to cope with. The large increase in venous pressure pushes starling’s curve onto the flat part (over filling of the ventricles leading to stretching, see above). There is a risk of pulmonary oedema, because the outputs of the right and left ventricle can only be matched by stroke volume, which relies on Starling’s curve. If the right heart pumps more, the left fills more and so pumps more. But if at the top of the starling curve the left heart cannot respond to the right, blood accumulates in the lungs. Overfilling of the ventricles is prevented by a rise in heart rate When venous pressure starts to rise, heart rate is already high Stroke volume kept down, but CO increased Demand met – System Stable
LO 6.13 Discuss the response of the cardiovascular system to Standing Up, and postural hypotension
On standing, blood pools in the superficial veins of the legs (Great/Short Saphenous veins) due to gravity Central venous pressure falls Cardiac output falls due to the fall in venous pressure (starling’s law) Arterial pressure falls Both arterial and venous pressure falling Baroreceptors detect fall in arterial pressure Raise HR, but venous pressure is still low TPR increased to defend arterial pressure (skin, gut) Sometimes these reflexes (Baroreceptor Reflex) don’t work. This is referred to as postural hypotension.
LO 6.14 Discuss the response of the cardiovascular system to Haemorrhage
Reduced blood volume lowers venous pressure So cardiac output falls (Starlings law) Arterial pressure falls Baroreceptors detect fall in arterial pressure, HR rises, TPR increased Rise in HR lowers venous pressure further Problem is worse, not better HR can become very high Venous pressure needs to be increased to solve original problem Veno-constriction Blood transfusion to replace lost volume
LO 6.15 Discuss the response of the cardiovascular system to a long term increase in blood volume
Blood volume is under the control of the kidney If blood volume increases for days Increase in venous pressure Cardiac output rises Arterial pressure rises More blood peruses tissues, which auto-regulate and increase TPR Arterial pressure rises further, and stays up
LO 7.1 Describe the processes which generate the resting membrane potential of cardiac cells
The cardiac resting membrane potential is the potential inside a cardiac cell relative to the extracellular solution. The difference between the two is achieved by the selective permeability of the membrane to different ions, by way of channel proteins. The cell membrane of myocardial cells is mostly permeable to K+ ions. So the cardiac resting membrane potential of ~ -90mV is largely due to the K+ equilibrium potential of -80mv (see membranes and receptor module). K+ ions move down their concentration gradient, from the inside to the outside of the cell, taking their positive charge with them.
LO 7.2 Draw and explain the membrane permeability changes, resulting in membrane potential changes of (i) ventricular cells (ii) pacemaker cells over the cardiac cycle only part i
Ventricular Cells In diastole, the resting membrane potential of cardiac cells is close to the equilibrium potential of K+ (4). Initial depolarisation due to spread of electrical activity from pacemaker cells. Once threshold has been reached, fast voltage gated sodium channels are opened, causing depolarisation towards Na+’s equilibrium potential (0). Following the rapid depolarisation, a brief repolarisation caused by the outward flow of K+ returns the membrane potential to ~0. (1) Na+ channels deactivate, but the depolarisation causes the opening of voltage gated Ca2+ channels, which take longer to activate, keeping the membrane depolarised (2). Influx of Ca2+ causes the release of further Ca2+ from cellular stores, causing contraction (See M&R Session 5). After ~250ms, Ca2+ channels close. Efflux of K+ returns membrane potential to resting (3).
LO 7.2 Draw and explain the membrane permeability changes, resulting in membrane potential changes of (i) ventricular cells (ii) pacemaker cells over the cardiac cycle only part ii
Pacemaker Cells The maximum –‘ve voltage of pacemaker cells is ~-60mv, less than the -90mv of ventricular muscle cells. This persistently less –‘ve membrane voltage causes the fast Na+ channels to remain inactivated. The spontaneous gradual depolarisation of pacemaker cells, the pacemaker or ‘funny’ current (If) is carried by Na+ ions through slow Na+ channels that open during the repolarisation of the cell as the potential approaches its most –‘ve values. Once the cell reaches its threshold voltage due to the If, Ca2+ channels open, giving a relatively slow depolarisation. This is due to the deactivation of the fast Na+ channels. Once Ca2+ channels close, the cell repolarises due to K+ efflux.
LO 7.2 Describe the membrane potential changes in pacemaker cells associated with increases and decreases in heart rate, and the cellular mechanisms controlling heart rate
Increasing Heart Rate The interval between beats depends on how fast the pacemaker potential depolarises. The interval is shortened by the action of the Sympathetic nervous system on the SAN. Noradrenaline (α2 Receptor) speeds up the heart rate by making the pacemaker potential steeper. Decreasing Heart Rate The interval between pacemaker potentials is lengthened by the action of the Parasympathetic nervous system on the SAN. Acetylcholine (M3 Receptor) slows the heart rate by making the pacemaker potential shallower. Baroreceptors Baroreceptors, located in the arch of the aorta and the carotid sinus have a role in controlling Heart rate. When arterial blood pressure is high, the aorta/carotid arteries are stretched, activating the stretch sensitive baroreceptors. The baroreceptors pass the information to the medulla, which in turn causes parasympathetic innervation of the SAN. Parasympathetic innervation causes the pacemaker potential to become shallower, slowing the heart rate. Low BP has the opposite effect.
LO 7.3 Describe the types of drugs used to treat patients with common cardiovascular disorders
Cardiovascular drugs are used to treat: - Arrhythmias - Heart Failure - Angina - Hypertension - Risk of thrombus formation Cardiovascular drugs can alter: - The rate and rhythm of the heart - The force of myocardial contraction - Peripheral resistance and blood flow - Blood volume
LO 7.4 Understand how arrhythmias can arise
Causes of arrhythmias include: Ectopic Pacemaker activity Damaged area of myocardium because depolarised and spontaneously active. Latent pacemaker region activated due to ischaemia Dominate over SA node After-Depolarisations Abnormal depolarisations following the action potential Thought to be caused by high intracellular Ca2+ Longer AP leads to longer QT interval Re-entry loop Conduction delay Normal spread of excitation disrupted due to damaged area Incomplete conduction damage (uni-directional block) It is possible to get several small re-entry loops in the atria, e.g. from being stretched over time, leading to atrial fibrillation.
LO 7.5 Describe the classes of anti-arrhythmic drugs and the principles of their therapeutic use
Class I. (Voltage Gated Na+ Channel Blockers) A typical example is the local anaesthetic lidocaine. Only channels that are in an open or inactive state are blocked, and it dissociates rapidly in time for the next AP. Normal firing of AP’s is not stopped, but it prevents the firing of AP’s too close to one another. As Na+ channels are blocked, after-depolarisations cannot trigger another AP. Class II. (B-adrenoceptor antagonists) E.g. Propranolol, Atenolol (Beta Blockers) Block sympathetic action by acting on 1 receptors in the heart, decreasing the slope of the pacemaker potential in the SAN. Inhibits adenyl cyclase, decreasing inotropy. Used after an MI, to combat increases sympathetic activity and to reduce the O2 demand of the myocardium. Class III. (Drugs that block K+ channels) Prolong the action potential, by blocking K+ channels (which are responsible for repolarisation). The absolute refractory period is lengthened, preventing another AP from occurring too soon. They are not generally used because they can also be pro-arrhythmic. Class IV (Drugs that block Ca2+ channels) E.g. Verapamil Decreases slope of pacemaker action potential at SA node. Also decreases AV nodal conduction and decreases the force of contraction. Some coronary and peripheral vasodilation. Adenosine Adenosine is produced endogenously and acts on A1 receptors (Note – NOT α1) (GPCR, inhibits adenylyl cyclase) at the AV node. Enhances K+ conductance and hyperpolarises cells of conduction tissue. It is anti-arrhythmic, but doesn’t belong in any of the 4 categories. “Resets” the heart.
LO 7.6 Define the term inotropic drug and the circumstances under which these drugs can be used
Inotropic drugs are drugs that affect the force of contraction of the heart. Negatively inotropic drugs are used in circumstances where it is beneficial to reduce the workload of the heart, for example after a myocardial infarction. This reduces the O2 requirement of the heart and limits further damage. B-blockers are examples of negative inotropic drugs. Positive Inotropic drugs are used in circumstances where the heart needs to beat more strongly, for example cardiogenic shock or acute but reversible heart failure (eg following cardiac surgery). -adrenoceptor agonist, e.g. dobutamine are examples of positive inotropic drugs.
LO 7.7 Describe how drugs can be used in the treatment of heart failure
ACE-inhibitors and diuretics have an important role in the treatment of chronic heart failure. ACE-inhibitors prevent the formation of the vasoconstrictor angiotensin II, thus promoting vasodilation of arterioles and venous dilation. This decreases both afterload and preload to the heart. ACE-inhibitors also have a diuretic action since angiotensin II promotes aldosterone release from the adrenal cortex (zona glomerulosa). Aldosterone causes Na+ and water retention, increasing blood volume – so reducing it decreases blood volume and decreases pre-load to the heart.
LO 7.8 Describe how drugs can be used in the treatment of Angina
Angina occurs when O2 supply to the heart does not meet its need. Ischemia of the heart tissue leads to chest pain, usually on exertion and relieved by rest. It is due to narrowing of the coronary arteries (atheromatous disease) Angina is treated by reducing the work load of the heart, with B-blockers, Ca2+ channel blockers, and organic nitrates. Organic nitrates and Ca2+ channel blockers also improve Blood supply to the heart. Action of Organic Nitrates The reaction of organic nitrates with thiols (-SH groups) in vascular smooth muscle causes NO2- to be released. NO2- is reduced to NO, which is a powerful vasodilator. NO activates guanylate cyclase, increasing cGMP and lowering intracellular Ca2+ to cause relaxation of vascular smooth muscle. Primary Action Acts on the venous system as a venodilator (Note – VENOdilator), lowering central venous pressure and preload. The heart fills less; therefore force of contraction is reduced (Starling’s Law). Secondary Action Acts on the coronary arteries, improving O2 delivery to the ischaemic myocardium.
LO 7.9 Understand the risk of thrombus formation with certain cardiovascular conditions and understand how to treat this
Certain heart conditions, such as atrial fibrillation and valve disease carry an increased risk of thrombus formation. Anti-thrombotic drugs such as warfarin may be used in these cases. The anti-platelet drug aspirin is used following MI or in coronary artery disease where there is a risk of MI to reduce the risk of platelet rich arterial clots forming.
LO 7.10 Describe how drugs can be used in the treatment of Hypertension
Hypertension is an important cardiovascular condition since it carries the risk of developing cardiovascular disease of stroke. Drugs used in the treatment of hypertension act to reduce cardiac output and/or peripheral resistance. These include ACE-inhibitors (Angiotensin Converting Enzyme inhibitors), diuretics, adrenoceptor blocks and calcium channel blockers.
LO 8.1 Describe in general terms and draw a diagram of the pattern of spread of excitation over the normal heart from the SA node to the AV node to the ventricles
An action potential is generated by the pacemaker cells in the SAN (1), and electrical activity spreads over the surface of the heart to the AV node, where there is a delay of ~120ms (2). After the delay, the excitation spreads down the septum via the right and left bundle branches (3), then out over the ventricular myocardium, from inside to outside (endocardial to epicardial surface) until all ventricular cells are depolarised. (4/5) After ~280ms the cells begin to repolarise. Repolarisation spreads in the opposite direction over the ventricle to depolarisation (epicardial to endocardial surface).
LO 8.2 Describe the signal recorded by an extracellular electrode placed near a myocardial cell during systole
At each systole, each cell fires an action potential, including a depolarisation and re-polarisation. However, electrodes that are outside cells view this differently to those inside cells. Extracellular electrodes only record changes in membrane potential, therefore skin electrodes ‘see’ two signals with each systole.
LO 8.3 Be able to state rules governing the sign of the signal recorded by a positive recording electrode when depolarisation and repolarisation spread towards and away from that electrode
What an electrode ‘sees’ depends on its position relative to the spread of activity. There are simple rules to predict the signal: Depolarisation moving towards an electrode – Upward Signal Depolarisation moving away from an electrode – Downward Signal Repolarisation moving towards an electrode – Downward signal Repolarisation moving away from an electrode – Upward Signal The more muscle depolarising and the more directly towards the electrode the signal is moving, the bigger the amplitude.
LO 8.4 Describe the form of signal recorded by a single electrode ‘viewing’ the heart from the apex.
1.Atrial depolarisation will produce a small upward deflection. It is small because there is little muscle, and upward as it is moving towards the electrode. 2.~120ms delay 3.Excitation spreads about halfway down the septum, then out across the axis of the heart. Produces a small downward deflection, downward as it is moving away and small because it is not moving directly away. 4.Depolarisation spreads through the ventricular muscle along an axis slightly to the left of the septum, producing a large upward deflection. Upwards because it is moving towards the electrode, and large because there is lots of muscle and the signal is moving directly towards the electrode. 5.Depolarisation spreads upwards to the base of the ventricles, producing a small downward deflection. Downwards because moving away, small because not moving directly away. 6.Ventricular contraction (~280ms) 7.Repolarisation begins on the epicardial surface. Spread through the ventricular myocardium in the opposite direction to depolarisation. Produces a medium upward deflection. Upwards because it is moving away, medium because timing in different cells is dispersed.
Identify the signals associated with atrial depolarisation, ventricular depolarisation and ventricular repolarisation PQRST?
P wave Atrial Depolarisation Q wave Septal depolarisation spreading to ventricle R wave Main ventricular depolarisation S wave End ventricular depolarisation T wave Ventricular repolarisation
LO 8.5 Describe how the QRS will change if the viewing electrode is moved around a circle with the heart at its centre
As the electrode moves around the heart, the directions and amplitude of the waves changes predictably. An electrode viewing the R wave head on will see a large upward deflection, viewing sideways on sees no signal, viewing end of sees a large downward signal.
LO 8.6 Be able to place electrodes correctly to record from ECG leads I, II, III, aVR, aVL, aVF and chest leads V1-6
Even though this is a 12 lead ECG, it is actually conducted with 10 electrodes (4 limb and 6 chest), and only 9 of these are recording (right lower limb is neutral). Limb leads: One on each limb Provides a vertical view of the heart. Ride – Red, right upper Your – Yellow, left upper Green – Green – Left lower Bike – Blue – Right lower Chest leads: Must be placed in correct anatomical position (as shown in the picture on that handsome ripped young male model). Provides a horizontal view of the heart.
LO 8.8 Calculate the heart rate from a rhythm strip for a regular and irregular heart rhythm
Rate All ECG machines run at a standard rate of 300 squares per minute. Therefore to calculate heart rate, you divide 300 by the number of squares of the R – R interval. Heart Rate=300/(No.of squares in the R-R Interval) For irregular rhythms it is important to use a larger interval than one R-R interval. For example, multiplying the number of beats in 10 seconds by 6.
Learn how to read ECG abnormalities
Use pics
LO 9.1 State the major differences between the properties of the systemic and pulmonary circulations
The lungs have two circulations – pulmonary and bronchial. The bronchial circulation is part of the systemic circulation, and meets the metabolic requirements of the lungs. The pulmonary circulation is the blood supply to the alveoli, required for gas exchange. The pulmonary circulation must accept the entire cardiac output, and works with low resistance due to short, wide vessels, lots of capillaries connected in parallel (lower resistance) and arterioles with relatively little smooth muscle. This low resistance leads to the circulation operating under low pressure.
LO 9.2 State the normal pressures in the pulmonary artery, pulmonary capillaries and pulmonary veins
Pulmonary Artery 12-15mm/hg Pulmonary Capillaries 9-12mm/hg Pulmonary Veins 5mm/hg
LO 9.3 Explain the concept of ventilation perfusion matching in the pulmonary circulation
For efficient oxygenation, ventilation of the alveoli needs to be matched with perfusion. The optimal Ventilation/Perfusion ratio is 0.8. Maintaining this means diverting blood from alveoli that are not well ventilated. This is achieved by hypoxic pulmonary vasoconstriction. Alveolar hypoxia results in vasoconstriction of pulmonary vessels, and the increased resistance means less flow to the poorly ventilated areas and greater flow to well ventilated areas. Chronic hypoxic vasoconstriction can lead to right ventricular failure. The chronic increase in vascular resistance puts a high afterload on the right ventricle, leading to its failure.
LO 9.4 Describe the forces which are involved in the formation of tissue fluid in the lungs and in the systemic circulation
Starling forces determine the formation of tissue fluid. Hydrostatic pressure of blood within the capillary pushes fluid out, and oncotic pressure (colloid osmotic pressure) exerted by large molecules such as plasma proteins draws fluid back in. Venous pressure has the greatest effect on capillary hydrostatic pressure, so in the low pressure pulmonary system, only a small amount of fluid leaves the capillaries. If capillary pressure increases, pulmonary oedema can occur. In an upright position there is greater hydrostatic pressure on vessels in the lower lung due to gravity. Pulmonary oedema impairs gas exchange, and is also affected by posture. The fluid is mainly at the base of the lungs when upright, and throughout the lung when lying down.
LO 9.5 Describe the relationship between the mechanical work and oxygen demand of the myocardium
The coronary circulation must deliver O2 at a high basal rate, which must rise to meet increased demand as cardiac work rate can increase five fold. There is an almost linear relationship until very high O2 demand, where there is a small increase in the amount of O2 extracted.
LO 9.6 Describe the particular features of the coronary circulation
The right and left coronary arteries arise from the right and left aortic sinuses, and fill during diastole. In systole, the contraction of the heart muscle makes the pressure in the coronary arteries too high for filling. Cardiac muscle has a high capillary density to efficiently deliver O2, and the continuous production of NO by coronary endothelium maintains a high basal flow.
LO 9.7 Describe the consequences of partial or total occlusion of coronary arteries
Coronary arteries are functional end arteries, which are prone to atheromas. Narrowed coronary arteries lead to angina on exercise (inc. O2 demand). Stress and cold can also cause sympathetic coronary vasoconstriction and angina. Sudden obstruction by thrombus causes myocardial infarction
LO 9.8 Describe the factors which influence blood flow through the brain
The brain has a high O2 demand, receiving about 15% of Cardiac Output. The O2 consumption of Grey matter accounts for ~20% of total body consumption at rest. The cerebral circulation meets the high demand for O2 by having a high capillary density, with a large surface area for gas exchange and reduced diffusion distance (<10um), a high basal flow rate (x10 the body average) and high O2 extraction (35% above average) Secure O2 supply to the brain is essential as neurones are very sensitive to hypoxia. A few seconds of cerebral hypoxia will lead to a loss of consciousness (syncope) and irreversible damage occurs in ~4 minutes. Interruption to blood supply, e.g. stroke causes neuronal death. Secure blood supply is ensured: Structurally Anastomoses between basilar and internal carotid arteries Functionally Brainstem regulates other circulations Myogenic auto-regulation maintains perfusion during hypotension Metabolic factors control blood flow Myogenic Auto-Regulation Cerebral resistance vessels have a well developed myogenic response to changes in transmural pressure (pressure across the wall). Increased Blood Pressure leads to Vasoconstriction Decreased Blood Pressure leads to Vasodilation This serves to maintain cerebral blood flow when BP changes. Fails below 50mmHg. Metabolic Regulation Cerebral vessels are very sensitive to changes in arterial PCO2. Panic hyperventilation can cause hypercapnia and cerebral vasoconstriction leading to dizziness or fainting. Regional Activity Areas with increased neuronal activity have increased blood flow. Adenosine is a powerful vasodilator of cerebral arterioles. Cushing’s Reflex The rigid cranium protects the brain, but does not allow for volume expansion. Increased intracranial pressure, e.g. from a cerebral tumour or haemorrhage, impairs cerebral blood flow. Impaired blood flow to the vasomotor control regions of the brainstem increases sympathetic vasomotor activity, increasing arterial BP and helping to maintain cerebral blood flow. Increased Cerebral BP leads to Peripheral Vasoconstriction and thus leads to More flow to brain
LO 9.9 Describe in broad outline the factors which influence blood flow through skin
The Cutaneous Circulation Most blood flow through skin is not nutritive, and much of the blood flows through aterio-venous anastomoses (AVAs) rather than capillaries. The cutaneous circulation has a special role in temperature regulation, as the skin is the body’s main heat dissipating surface. The amount of blood flow to the skin, and therefore the degree of heat lost, is heavily influenced by the sympathetic nervous system. Decreased core temperate leads to sympathetic innervation causing increased tone in AVAs, decreasing blood flow to apical skin. Similarly when core temp is high, reduced vasomotor drive to AVAs allows them to dilate and there is a low resistance shunt of blood to the venous plexus, which is close to the surface and allows for the dissipation of heat.
LO 9.9 Describe in broad outline the factors which influence blood flow through skeletal muscle
Skeletal Muscle Circulation The metabolic activity of skeletal muscle varies over an enormous range and so does the blood flow. At rest most capillaries within a muscle are shut off by contraction of pre-capillary sphincters. Increases in blood flow are brought about mainly by opening up more capillaries under the influence of vasodilator nervous activity and local metabolites that tend to reduce sympathetic vasoconstrictor tone. Flow can be increased > 20x in active muscle. At rest only ~1/2 of capillaries are perfused at any one time.
LO 10.1 Identify the common causes of chest pain Mention all systmes
There are many causes of chest pain, not just to do with the CVS: Lungs and Pleura - Pneumonia - Pulmonary Embolism - Pneumothorax GI System - Oesophagus – Reflux - Peptic ulcer disease - Gall Bladder – Biliary colic, cholecystitis Chest Wall - Ribs – fractures, bone metastases - Muscles - Skin CVS – Heart & Great Vessels - Myocardium – Angina, MI - Pericardium – Pericarditis - Aorta – Aortic dissection
LO 10.2 Describe the risk factors for coronary atheroma
There are both modifiable and non-modifiable risk factors for coronary atheroma – and by extension Ischaemic Heart Disease. Non-Modifiable - Increasing Age - Male gender (females catch up after menopause) - Family history Modifiable * Top 4 most important - Hyperlipidaemia - Smoking - Hypertension - Diabetes mellitus – Doubles IHD risk - Exercise - Obesity - Stress
LO 10.3 Describe the pathophysiology and treatment of stable angina
Atheromatous plaques, with a necrotic centre and fibrous cap build up in the coronary vessels, occluding more and more of the lumen, leaving less space for the passage of blood. This leads to ischaemia of the myocardium. Angina occurs when the plaque occludes more than 70% of the lumen. Chest pain in stable angina is typical ischaemic chest pain in brief episodes, brought on by exertion, emotion particularly after meals and in cold weather. It is described as mild to moderate pain Treatment of Angina Acute Episodes – Sub lingual nitrate spray/tablet Prevent Episodes - -blockers, Ca2+ channel blockers, Oral nitrates Prevent Cardiac Events – Aspirin, Statins, ACE Inhibitors Long Term – Consider revascularisation
LO 10.3 Describe the pathophysiology and treatment of unstable stable angina
As angina worsens due to the progression of the formation of the Atheromatous plaque, it progresses from Stable to Unstable Angina. This happens due to increased occlusion of the lumen. Unstable Angina is classified as Ischaemic Chest Pain that occurs at rest (or with minimal exertion) described as severe pain and occurring with a crescendo pattern (distinctly more severe, prolonged, or frequent than before)
LO 10.3 Describe the pathophysiology and treatment of a myocardial infacrtion
A MI is a complete occlusion of a coronary vessel, leading to an infarct (death) of the myocardium it supplies. The fibrous cap of the Atheromatous plaque can undergo erosion or fissuring, exposing blood to the thombogenic material in the necrotic core. The platelet ‘clot’ is followed by a fibrin thrombus, which can either occlude the entire vessel where it forms or break off to form an embolism. MI presents with typical ischaemic chest pain (see above) that is very severe, persistent, at rest and often with no precipitant. It is not relieved by rest or nitrate spray. The patient may also be breathless, faint (due to LV dysfunction) have a ‘feeling of impending death’ and will have autonomic features present such as sweating, pallor, nausea and vomiting. NSTEMI – Non ST Elevated Myocardial Infarction – Infarct is not full thickness of myocardium STEMI - ST Elevated Myocardial Infarction - Infarct is full thickness of myocardium
LO 10.4 Describe the investigation of a patient with angina, including the principles of the exercise stress test
The clinical diagnosis of Angina is based on history. There are no specific signs on examination, but may show signs related to…: Risk Factors - Elevated BP - Corneal Arcus LV Dysfunction Evidence of atheroma elsewhere - E.g. signs of peripheral vascular disease The resting ECG is usually normal, but may show signs of a previous MI (pathological Q wave). To confirm angina and assess it’s severity, an exercise stress test is undertaken. Exercise Stress Test Graded exercise on a treatment connected to an ECG until: Target heart rate reached OR Chest Pain OR ECG changes OR Other problems – arrhythmias, low BP etc… Test is positive is the ECG shows ST Depressions of > 1mm. A strong positive test indicates critical stenosis.
LO 10.5 Understand the concept of ‘Acute Coronary Syndrome’ and explain the difference between unstable angina, NSTEMI and STEMI
Acute Coronary Syndrome (ACS) relates to a group of symptoms attributed to the obstruction of the coronary arteries. ACS is a result of: - Unstable Angina - NSTEMI - STEMI Clinically the three are often difficult to distinguish, and the priority is to split them into two groups, as the treatment is different. Unstable Angina Partial thrombus occlusion No myocardial necrosis Possible ST depression and T inversion No biochemical blood markers NSTEMI Partial occlusion by thrombus Some myocardial necrosis No ST depression Troponin detectable STEMI Total occlusion Large myocardial necrosis ST elevation Troponin levels raised
LO 10.7 Describe the use of cardiac biomarkers (troponin and cardiac enzymes) in the diagnosis of MI, distinguishing between NSTEMI and unstable angina in patients with Acute Coronary Syndrome
Troponins Cardiac Troponin I (cTnI) and Troponin T (cTnT) are proteins important in actin/myosin interaction, which are released in myocyte death. It is a very sensitive and specific marker, rising 3-4hrs after the first onset of pain and peaking at 18-36hrs. They will then decline slowly for up to 10-14 days. Creatine Kinase (CK) Three iso-enzymes present in the skeletal muscle, heart, brain. CK-MB is the cardiac iso-enzyme, rising 3-8hrs after onset, peaking at 24hrs. Levels will return to normal in 48-72hrs. The presence of either of these enzymes means there has been death of the myocardium. It therefore distinguishes between unstable angina and NSTEMI, as there is no tissue death in unstable angina and there is in NSTEMI
LO 10.8 Describe in principles the management of Unstable angina and acute MI
Treatment of Unstable Angina/MI Goal : Prevent UA from progressing to MI and limiting muscle loss in MI Prevent progression of thrombosis -Anti Thrombotic therapy o Anti platelet agents: Aspirin o Anticoagulants: Heparin Restore perfusion of partially occluded vessels High risk o Early Percutaneous Coronary Intervention (Angioplasty) (PCI) o Coronary Artery Bypass Graft (CABG) Low Risk - Initially General medical treatment o GTN Spray o Pain control o O2 o Organic Nitrates o B-blockers o Statins o ACE-Inhibitors
LO 10.9 Understand the use of surgical treatments in coronary artery disease
Angiography can be used to view any vessel occlusions, and from the findings choices can be made about revascularisation surgeries. Percutaneous Coronary Intervention (PCI) – Angioplasty and stenting. Inflation of a balloon inside the occluded vessel expands a mesh that holds the vessel open, increasing the lumen size and allowing for more blood to flow. Coronary By Pass Grafting (CBPG) involves taking an artery from elsewhere in the body, e.g. internal mammary artery, radial artery, saphenous vein (reversed because of valves) and grafting it to the heart.
LO 10.10 Describe the signs and symptoms of acute pericarditis
Causes - Infections (viral, TB) - Post MI/cardiac surgery - Autoimmune - Uraemia (kidney failure) - Malignant Deposits Symptoms - Central/left sided chest pain - Sharp, worse than inspiration - Improved by leaning forward
LO 11.1 Define heart failure
Heart failure is ‘a state in which the heart fails to maintain an adequate circulation for the needs of the body despite an adequate filling pressure’.
LO 11.2 Explain the pathophysiology of heart failure
Ischaemic Heart Disease is the primary cause of Systolic Heart Failure. Other causes of HF include: o Hypertension o Dilated cardiomyopathy - Bugs - Alcohol/Drugs/Poisoning - Pregnancy o Valvular heart disease / Congenital o Restrictive cardiomyopathy e.g. amyloidosis o Hypertrophic cardiomyopathy o Pericardial disease o High-Output heart failure o Arrhythmia
LO 11.3 Be able to draw and explain the normal relationship between central venous pressure (or end diastolic pressure) and cardiac output and how that relationship alters with increasing severity of heart failure
To understand heart failure you need to understand Starling’s Law of the Heart (LO 6.7). The force developed in the myocardium depends on the degree to which the fibres are stretched (or how much the heart is filled). In heart failure the heart can no longer produce the same amount of force (or cardiac output) for a given level of filling.
LO 11.4 Describe the clinical characteristics of the principal types (classes) of heart failure, and the circumstances that lead to its development
Class I o No symptomatic limitation of physical activity Class II o Slight limitation of physical activity o Ordinary physical activity results in symptoms o No symptoms at rest Class III oMarked limitation of physical activity o Less than ordinary physical activity results in symptoms o No symptoms at rest Class IV o Inability to carry out any physical activity without symptoms o May have symptoms at rest o Discomfort increases with any degree of physical activity Heart failure can affect one or both sides of the heart. However, right-sided heart failure rarely occurs on its own (although it can in the case of chronic lung disease). The most common scenario is one of left-sided heart failure that raises pulmonary arterial pressure leading to additional right-sided heart failure. When both ventricles are affected it is referred to as congestive heart failure. Clinical Signs of Heart Failure In clinical practice, heart failure is often divided into: Left sided heart failure Right sided heart failure Bi ventricular (congestive) cardiac failure and Systolic heart failure Diastolic Heart failure Signs/Symptoms of Left Sided Heart Failure Fatigue, shortness of breath upon exertion or when lying flat, waking from sleep with shortness of breath Tachycardia Cardiomegaly (displaced apex beat) 3rd or 4th heart sound (‘Gallop rhythm’) Functional murmur of mitral regurgitation Basal pulmonary crackles Peripheral oedema Right Sided Heart Failure Most common is 2ndary to Left Heart Failure Chronic lung disease Pulmonary embolism/hypertension Pulmonary/tricuspid Valvular disease LefttoRight shunts (ASD/VSD) Isolated right ventricular cardiomyopathy Signs/Symptoms of Right Sided Heart Failure Relate to distension and fluid accumulation (Peripheral Oedema) in areas drained by the systemic veins Fatigue, dyspnoea, anorexia, nausea Raised JVP Tender, smooth hepatic enlargement Dependent pitting oedema Ascites Pleural effusion
LO 11.5 Describe the involvement of the renin-angiotensin-aldosterone system and the sympathetic nervous system in heart failure
The Renin-Angiotensin-Aldosterone-System (RAAS) system are both activated in heart failure in an attempt to maintain cardiac output. This has the effect of making an already struggling heart work harder. A drop in blood pressure, such as in heart failure, stimulates renin release from the kidneys. Renin is an enzyme which catalyses the conversion of angiotensin to angiotensin I. Angiotensin I is converted to II by ACE. Angiotensin II is a powerful vasoconstrictor and promotes the release of aldosterone from the kidneys. Aldosterone causes salt and water retention in the kidneys, increasing blood volume. The sympathetic nervous system causes vasoconstriction of blood vessels via the 1 receptor. This increases blood pressure, increasing the workload of the heart by increasing both the preload and afterload on the heart. Sympathetic innervation of the heart’s 1 receptors will also cause an increase in both Chronotropy and Inotropy.
LO 11.6 Identify targets for drug action to manipulate cardiac output
ACE-Inhibitors are used in the treatment of heart failure to prevent the conversion of angiotensin I to II. ACE inhibitors thus have an indirect vasodilatory and diuretic effect, both of which are beneficially in the treatment of heart failure by reducing the work load of the heart. Diuretics are also important in the treatment of heart failure to reduce blood volume and thus oedema. B-blockers are used to prevent the sympathetic innervation of the myocardium, again in an attempt to reduce the heart’s work load.
LO 11.7 Describe the principles involved in the general management of heart failure, and the categories of drugs used in its therapy
Management of Heart Failure – Principles - Correct underlying cause - Non-pharmacological measures - Pharmacological therapy o Symptomatic improvement o Delay progression of heart failure o Reduce mortality - Treat complications/associated conditions/cvs risk factors o Eg arrhythmias Drugs used to Treat Heart Failure - B-blockers o Block B1 receptors on the myocardium - ACE-Inhibitors o Prevent conversion of Angiotensin I to II - Ca2+ channel blockers o Reduce contractility of the myocardium - Organic Nitrates o Veno/Vasodilator leads to a reduction in B.P. - Cardiac Glycosides o Increase CO and heart contractility by inhibiting the Na/K pump. Raising intracellular Na inhibits NCX, so intracellular Ca2+ increases in. contractility
LO 12.1 Describe the essential characteristics of shock
There is no unique definition of the term ‘shock’. It is used to describe acute circulatory failure with either inadequate or inappropriately distributed tissue perfusion, resulting in generalised lack of oxygen supply to cells.
LO 12.2 Describe the characteristics of the different types of shock
Cardiogenic Shock The inability of the heart to eject enough blood - Ischaemic cardiac damage - Arrhythmias Mechanical Shock Due to a restriction on the filling of the Heart - Cardiac tamponade o Pressure outside the heart impairs filling Obstruction to blood flow through the lungs - Pulmonary embolism o RV cannot empty, reduced return to LA Hypovolaemic Shock Loss of circulating fluid volume - Haemorrhage o Venous pressure falls, CO falls (Starling’s Law) o Treat by infusing fluid, colloid/blood Normovolaemic (distributive) Shock Due to uncontrolled falls in peripheral resistance - Dramatic drop in arterial pressure - Sepsis o Endotoxins released by circulating bacteria cause profound peripheral vasodilation o Treat with adrenaline (Vasoconstriction, A1 receptors) and antibioitcs - Anaphylaxis o Release of histamine from mast cells causing profound vasodilation o Treat with adrenaline (Vasoconstriction, A1 receptors)
What is this and label it?


How is the heart muscle structurally adapted/organised to best pump blood?
All the cells are connected electrically and so Electrical activity in one cell of the heart will lead to activity in all in normal circumstances.
Ventricular muscle is organised into figure of eight bands that squeeze the ventricular chamber forcefully in a way most effective for ejection through the outflow valve. The apex of the heart contracts first and relaxes last to prevent back flow.
LO 4.2 State the different types of signalling peptide and which receptor type each uses
Signal
Receptor
G-Protein
Effector
Physiological Response
Adrenaline/
Noradrenaline
b-Adrenoceptor
Gs
Stimulates Adenylyl Cyclase
Glycogenolysis, lipolysis
Acetylcholine
M3-Muscarinic
Gq
Stimulates Phospholipase C
Smooth Muscle Contraction
Acetylcholine
M2-Muscarinic
Gi
Inhibits Adenylyl Cyclase
Stimulates K+ Channel
Slowing of Cardiac Pacemaker
Light
Rhodopsin
Gt
Stimulates Cyclic GMP Phosphodiesterase
Visual Excitation


