Cardiovascular Flashcards
(34 cards)
what does the frank-starling curve relationship describe?
how the contractile force of the myocardium (stroke volume or cardiac output) is dependent on the sarcomere length (diastolic filling volume or preload) immediately before contraction.

Answer A: furosemide (correct)
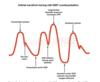
Answer B: Vasodilators, such as angiotensin-converting enzyme inhibitors or nitroglycerin, also move patients to improved ventricular function curves while reducing cardiac filling pressures, as seen by arrow B. Combinations of drugs often will yield additive effects on hemodynamics.
Answer C: Milrinone is a phosphodiesterase inhibitor that leads to improved inotropy and vasodilation. It causes a leftward and upward shift of the Frank-Starling curve as depicted by arrow C.
Answer D: Increases in contractility (e.g. associated with exercise, epinephrine, or milrinone) will lead to an increase in cardiac output. Inotropic agents will move patients to a higher ventricular function curve resulting in greater cardiac work for a given level of ventricular filling pressure. The ventricular pressure for a pure inotrope or one with vasoconstrictive properties (e.g. norepinephrine and epinephrine) will not change significantly but the contractile state will improve. This is represented by arrow D.

Wolff-Parkinson-White syndrome can be identified with the classical shortened PR interval and delta wave on ECG. Supraventricular tachycardia in patients with WPW can be safely managed with procainamide.
Avoid drugs that prolong av conduction…like adenosine or diltiazem
how can pericardial tamponade be differentiated from heart failure?
presence of pulsus paradoxus (a drop of at least 10 mm Hg (or >9%) in systolic arterial blood pressure on inspiration),
Beck’s Triad?
Cardiac tamponade:
Hypotension with narrow pulse pressure
JVD
Muffled Heart Sounds
what is the physiologic goals of HOCM?
Septal myectomy is the treatment of choice for HOCM refractory to medical treatment. Dual chamber pacing is a common red-herring. Treatment goals of HOCM and SAM are adequate preload, reduced contractility, avoidance of tachycardia, and adequate SVR.
What are absolute contraindications to TEE?
Relative?
Esophageal diverticulum (e.g. Zenker) is an absolute contraindication to TEE probe placement. The absolute contraindications to TEE include perforated injury to the esophagus, active upper GI bleed, esophageal tumor, esophageal stricture, and esophageal diverticulum.
The relative contraindications to TEE include history of radiation to neck/mediastinum, recent upper GI bleed, history of dysphagia, esophageal varices, symptomatic hiatal hernia, and coagulopathy.
tell me about fenoldopam?
Bottom Line: Fenoldopam has been shown to exert hypotensive effects characterized by a decrease in peripheral vascular resistance, along with an increase in renal blood flow, diuresis, and natriuresis.
TrueLearn Insight : Fenoldopam will lead to increases in intraocular pressure and should be administered with caution or avoided all together in patients with glaucoma or intraocular hypertension.
Which of the following medications would be the LEAST appropriate to use for induction during electroconvulsive therapy in a patient with coronary artery disease?
etomidate
methohexital
ketamine
propofol
Ketamine would be a less desirable agent for a patient with coronary artery disease compared to the other agents because it may potentiate the sympathetic surge often seen during electroconvulsive therapy (ECT) resulting in increased myocardial oxygen consumption and potentially ischemia.
How would you treat bradycardia in a heart transplant?
Direct acting β-adrenergic agents (e.g. isoproterenol, epinephrine) should be administered in the setting of bradycardia in a patient with a transplanted heart.


What is the wall blood supply in the 4 chamber TEE view?

what papillary muscle is most likely to rupture? why?
Posteromedial papillary muscle rupture is more common than anterolateral papillary muscle rupture due to the single blood supply (RCA or left circumflex artery) of the former and dual blood supply (LAD and left circumflex artery) to the latter.
what is inamrinone?
Milrinone and inamrinone (formerly called amrinone) are specific phosphodiesterase III (PDE III) inhibitors that function by interfering with the breakdown of cAMP. As cAMP levels increase in myocardial cells, intracellular calcium stores increase which improves contractility. Increased cAMP in vascular smooth muscle cells promotes vasodilation, and results in a reduction in systemic vascular resistance (SVR) and PVR. Overall, the net effect is improved cardiac output.
A 73-year-old male presents with dyspnea and pulmonary edema. He is admitted to the intensive care unit for stabilization. He has a decrescendo diastolic murmur as well as an increased pulse pressure. He also demonstrates bisferiens pulse waves.
what valve pathology?
Aortic Insufficiency
what is stroke volume index?
stroke volume * mean arterial pressure, normalized for body surface area
what is equation for ejection fraction?
EF = SV/EDV
what are the cardiac effects of sepsis?
CO?
Myocardial work?
Circulating cytokines and endotoxins in sepsis can cause myocardial depression despite a normal or elevated cardiac output.
what are the physiologic effects of pneumoperitoneum?
Laparoscopic surgery and the creation of a pneumoperitoneum increases intra-abdominal pressure and decreases abdominal end organ perfusion. Preload is decreased and afterload is increased when intra-abdominal pressure increases. Additionally, increased intra-abdominal pressure will decrease cerebral venous return and increase intracranial pressure.
Though a decrease in preload…there is an increase in CVP!!
MR is more likely with anterior or posterior MI?
Risk factors for acute MR following MI include: advanced age, prior myocardial infarction, infarct extension, inferior or posterior MI, multiple vessel coronary artery disease, and recurrent ischemia. The mainstay of treatment is afterload reduction and augmentation of coronary perfusion if needed following the infarction.
what can adenosine due to patients with respiratory disease?
adenosine should be cautiously used in patients with asthma or upper respiratory disease because adenosine can cause bronchoconstriction.
what can you tell me about long qt syndrome? cause? worsening drugs? treatements?
Congenital LQTS results from mutations in genes encoding sodium and potassium cardiac channels. Certain electrolyte abnormalities and pharmaceutical agents (e.g., certain antiarrhythmics, antipsychotics, antimicrobials, and volatile anesthetics) can worsen congenital LQTS or precipitate acquired LQTS. This increases the risk for ventricular arrhythmias, namely torsades de pointes. Beta-adrenergic receptor antagonists are the mainstay of therapy. Cardiac pacemakers or AICDs are indicated in patients for whom β-blockade is not efficacious (e.g., refractory or patient refusal).
drugs that can prolong QT?

what should the settings be for defib of v fib?
Defibrillation success decreases with arrhythmia time. Factors that improve defibrillation include quick electrode gel, biphasic defibrillation, and larger electrodes.
Lower-energy biphasic waveform defibrillation has equivalent or higher success for termination of VF than monophasic waveform defibrillation. There are multiple randomized and observational studies demonstrating the benefit of biphasic waveforms of relatively low energy (< 200 J) is considered safe and has equivalent or higher efficacy for ventricular fibrillation than monophasic waveform of equivalent or higher energy.