Cardiopulm Flashcards
Major ADLs Addressed in Cardiac Rehab
ABCDTT
A- Ambulating
B- Bathing
C- Continence
D- Dressing
T-Toileting
T-Transfers
Phase 1 (Inpatient) Cardiac Rehab
The goal for patients typically in ICU is 3-5 days. Then to Cardiac Stepdown unit.
Goals of PT Cardiac Rehab are:
• Activate; Get the patient moving in order to
combat effects of bed rest. (BSChair)
• Educate; Promote lifestyle modifications and
educate about recovery process
• Initiate; Begin process of returning patient
back to independent functioning (ADLS)
- Physical Therapy Exercise Guidelines:
- ADL’s, Ambulation, some UE/LE exercises (UE
avoid for CABG – 6-8wks)
• Low Intensity exercise (2-3 METS) -> 5 METS
by DC because 5 METS is what is required to perform ADLs.
- = 70% of max HR (greater is = high risk rMI)
- Duration: 5-10 minutes progressing duration
over days (maintain intensity within protocol)
• Frequency: 2-4x per day (ACSM)
*It takes 4-6 weeks to develop effective scar tissue
*MI strength training ACSM guidelines start at 5 weeks. CABG at 8 weeks because of sternal precautions
Contraindications:
- Exercise Discontinuation Criteria
- Diastolic blood pressure (DBP) >/= 110
- Decrease in systolic blood pressure >/=10
mmHg during exercise with increasing
workload (other symptoms don’t matter)
• Significant ventricular or atrial arrhythmias
with or without associated signs or
symptoms
- Second or third degree heart block*
- Signs and Symptoms of exercise intolerance
(angina, marked SOB, ECG changes related
to ischemia, >1mm dep)
Nitroglycerin Protocol
If symptoms persist, the patient is having a MI. If chest pain EVER worsens, you call EMS! First thing you do: stop the exercise. Second: Wait for 5 min Third: Reassess pain Fourth: If pain is still there, take a 2nd Fifth: Repeat Sixth: If pain is gone, restart at lower instensity. Seventh: After 3 Nitros and 15 min, and pt still have pain, call EMS!!
Phase 2 Cardiac Rehab
- Process (weeks to months)
- Patients enter a specialized cardiac rehabilitation outpatient program with qualified staff with ability to monitor vitals, EKG, and understand the patient’s medication regimen.
- Prior to entering Phase II it is recommended that the patient have a symptom-limited ETT at the 4-6 weeks mark.
- Phase II can begin immediately after phase I but will begin at a exercise prescription determined by the low level GXT
- Physical Therapy Goals
- Develop and facilitate a safe and effective formal exercise program
- Provide supervision and monitoring
- Return the patient to vocational and recreational activities or modify these activities to fit the patient clinical status
- Educate on secondary prevention measures (risk factor modification)
Physical Therapy Exercise Guidelines
- Intensity: Based on exercise test
- When The Test is Negative
- Common exercise prescription is 70-85% of
Max HR
- When The Test is Positive
- You must keep RPP below ischemic
threshold
- RPP = SBP x HR
- Stay >/=10 beats below ischemic threshold
Physical Therapy Exercise Guidelines
- Type: Aerobic and Strengthening
- Circuit training is optimal
- Train large mm groups before
small
• Strengthening @ 5wks post MI
/8 wks CABG
• Duration: 20-60 (5-10 minute warm
up/cool down)
• Frequency: 2-3x week
Exercise Discontinuation Criteria
- Diastolic blood pressure (DBP) >/= 110
- Decrease in systolic blood pressure >/=10
mmHg during exercise with increasing
workload (other symptoms don’t matter)
• Significant ventricular or atrial arrhythmias
with or without associated signs or
symptoms
- Second or third degree heart block*
- Signs and Symptoms of exercise
intolerance (angina, marked SOB, ECG
changes related to ischemia, >1mm dep)
*D/C Criteria is 9 METS
Phase 3 Cardiac Rehab
Process (Indefinitely)
• Patients enter a community based
exercise program, unsupervised,
maintenance
• Prior to entering Phase III the patient
must be able to complete 5 MET’s of
activity without symptoms, have stable
angina, and have medically controlled
arrhythmias during exercise.
- Physical Therapy Goals
- Improve and maintain functional
capacity
• Promote self regulation of
exercise programs
• Promote lifelong commitment to
risk factor modification
Physical Therapy Exercise Guidelines
- Intensity
- 50-85% of functional capacity
- Type
- Aerobic
- Strengthening
- Duration:
- 45-60 minutes (5-10 minute
warm up/cool down)
- Frequency:
- 3-5x week (begin following
CDC’s exercise guidelines)
Pulmonary Function Tests
Pulmonary tests that measure
lung volumes and capacities and
gas flow rates
- Lung Volumes (TLC, VC, IRV, ect)
- FEV1/FVC, FVC
- Allow us to determine if the
condition is obstructive or
restrictive
PULMONARY FUNCTION TESTS: GAS FLOW RATES
• Measure air flow rates during force breathing to provide information about the lung function and severity of lung impairment.
Forced vital capacity (FVC)
• Maximum amount of air that you can actually
move in and out of the lungs (3.5 – 4.5 L)
- Step one: Exhale deeply
- Step two: Take a maximum inhalation
- Step three: Maximally exhale as quickly as possible
- TELLS US IS THERE A LUNG PROBLEM
- Reduced in both restrictive and obstructive
conditions
Pulmonary Function Tests: Forced Vital Capacity 1 Sec
(FEV1)
• Maximum volume of air that can be
exhaled in one second
- Why do we care?
- Tells us information about airflow in the
large airways
• Determine restrictive or obstructive lung
condition
• TELLS US SEVERITY OF LUNG OBSTRUCTION
Forced Expiratory Volume
Forced Expiratory Volume
• Can be expressed as a fraction or
percentage (FEV1/FVC or FEV1%)
- Interpretation
- FEV1/FVC < .70 = Obstructive
Condition
• FEV1/FVC > .80 = Restrictive
Condition
• FEV1% of greater than 80% indicates
restrictive disease as long as FEV1/FVC is > .70
COPD Gold Stages
Stages 1-4, 1 being mild, 4 being severe

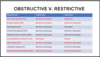
Measurements for Obstructive vs. Restrictive Lung Diseases
Check Picture
Normal Breath Sound-Tracheal
- Harsh, high-pitched sounds
- Above supraclavicular notch (1)

Normal Breath Sound- Bronchial
- Loud, high-pitched, tubular sounds
- Heard during inspiration &
expiration with a pause
• Just above clavicles on each side of
the sternum, over the manubrium (2)

Normal Breath Sound- Bronchovesicular
• Softer, tubular sounds heard between the
scapulae
- Continuous during inspiration & expiration
- Next to the sternum, & between scapulae (3)

Normal Breath Sound- Vesicular
• Low pitched soft sounds heard during
inspiration
• Remainder of lungs (Purple Part)

Abnormal (Adventitious) Breath Sound- Crackles
• “popping/crackling” discontinuous
sounds associated w/fluid in alveoli
& airways
• Heard during late inspiration as air
suddenly opens closed airways
• Pulmonary edema, pneumonia,
chronic bronchitis, pulmonary
fibrosis
Abnormal (Adventitious) Breath Sound- Wheezes
• continuous whistling,
high pitched noise
• Loudest on expiration,
caused by air forced thru
narrowed airways
• Asthma, bronchiectasis,
bronchitis

Abnormal (Adventitious) Breath Sound- Rhonchi
• “Gurgling or snore-like”
low pitched type noise,
caused by fluid in large &
medium sized airways
•Bronchitis, Bronchiectasis
pneumonia, CHF
Abnormal (Adventitious) Breath Sound- Stridor
• Inspiratory, high pitched
wheezing sound due to
tracheal narrowing and/or
disrupted airflow
• Anaphylactic shock, object
lodged in throat

Abnormal (Adventitious) Breath Sound- Pleural Friction Rub
• Scratching, grating noise
heard during inspiration and
expiration.
• Pleural effusion, pleurisy
(pleuritis), pneumonia
Abnormal Breathing Pattern- Cheyne-Stokes Respirations
• Breathing characterized by
progressively deeper, and
sometimes faster, breathing
followed by a gradual decrease that
results in a temporary stop in
breathing called an apnea (up to 60
sec)
• CHF, Stroke, TBI, End of life
respirations, opioids

Abnormal Breathing Pattern- Kussmaul Respirations
• Deep and labored (gasping)
breathing pattern
• Associated with decreased blood
pH caused by
- DKA (EMS)
- Metabolic acidosis (ABG question)
- Carbon monoxide poisoning

Abnormal Breathing Pattern- Fremitus
• Defined as the vibration that is
produced by the voice or by the
presence of secretions or increased
tissue density in the airways
• Increased fremitus = increased
density in the lung spaces
(consolidation/collapse**)
- Examples of increased fremitus
- Pneumonia
- Tumor or mass
- Cystic Fibrosis (Mucus plugs)
- Bronchitis
- Examples of decreased
fremitus
- Pneumothorax
- Hemothorax
- Pleural Effusion
- Emphysema
Abnormal Breathing Pattern- WHISPERING PETROLILOQUOY
While the examiner
auscultates over the lung
fields, the patient is asked to
whisper “one, two, three.
•When consolidation is
present..1,2,3 is heard
clearly
Abnormal Breathing Pattern- Egophony
Select sound frequencies are
able to pass through
consolidation and tend to
distort the sound of the
vowel “E” so that it is
perceived by the examiner as
“A” or “AAAH.”
Abnormal Breathing Pattern- Bronchophony
• Select sound frequencies are able to
pass through consolidation and
become louder over areas of
consolidation
• Patient repeats the numbers “99” or
”66”
• If the sound becomes louder over
suspected lung fields, consolidation is
present.
A High Frequency Chest Wall Oscillation (HFCWO)
vest that is attached to an air pulse
generator which rapidly inflates
and deflates the vest.
- Moves mucus to large airways
- Shouldn’t be used with intubated
patients or post op patients
FLUTTER VALVE THERAPY/ACAPELLA DEVICE
Handheld device that utilizes a
stainless steel ball that vibrates
back and forth, opening and
closing the devices air hole,
pulsing the air back into the
airways.
• Independent use some
children and most
adolescents/adults

Pulmonary Intervention Formula
Are the secretions stuck?
Vibration and/or Percussion, The Vest, Flutter Device
Does the patient need mobilization and
clearance?
ACBT, Autogenic Drainage
Does the patient just need clearance? If so, how
much assistance can they provide?
Huffing/Coughing, Manually assisted cough, MI/E, suctioning
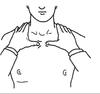
BRONCHO PULMONARY HYGIENE / POSTURAL DRAINAGE
Look at picture

PERCUSSION
• Manual percussion consists of a
rhythmical clapping with cupped hands
over the affected lung segment in PD
positions
- NPTE Reminders:
- No percussion with conditions/meds that
create brittle bones, contusions, or blood
thinning
• Percussion is used for mobilizing restricted
mucus not clear
Vibration
Vibration consists of placing the palmar
aspect of the clinician’s hands in full
contact with the patient’s chest wall. At
the end of a deep inspiration, the clinician
exerts pressure on the patient’s chest wall
and gently oscillates it through the end of
expiration.
- NPTE Reminders:
- More gentle than percussion but similar
contraindications because of pressure
provided
ACTIVE CYCLE OF BREATHING
• Sequence of maneuver used to mobilize
mucus to larger airways and clear
secretions
- Procedure:
- Breathing Control (Diaphragmatic Breathing)
- Thoracic Expansion (Deep Inhalation)
- Breathing Control
- Thoracic Expansion (Deep Inhalation)
- Breathing Control
- Forced expiration (Huffing)

AUTOGENIC DRAINAGE
• Sequence of maneuver used to mobilize
mucus to larger airways and clear secretions
- Procedure:
- 3 rounds of shallow breathing
- 3 rounds of medium volume breathing
- 3 rounds of deep volume breathing
- NPTE reminder:
- Difficult to teach <8yo or cognitively impaired
Huffing (Clearance)
• A deep inspiration
followed by a forced
expiration without glottal
closure. It is often used
in post-op patient who
find it painful to cough
MANUAL COSTOPHRENIC ASSIST / MANUAL ABDOMINAL THRUSTS
Active-assistive approach where
the therapist places his or her hand
on the child’s abdomen (just below
the diaphragm). The patient takes a
large breath in and holds it for 1 to
3 seconds.
• The patient then attempts to cough
as hard as possible while the
therapist provides compression
with an upward thrust in the
direction of the diaphragm.
MECHANICAL INSUFFLATION/EXSUFFLATION
(MIE)
• Assisted Coughing Machine
that adds in a high level of
positive pressure followed by
negative pressure to stimulate
a cough
• Typically added with a
manually assisted cough for
more effective removal of
secretion

SUCTIONING
• Passive elimination of secretions
through using a suctioning tube
within the tracheostomy.
- NPTE reminders:
- All active options were exhausted
- Patient has a tracheostomy
- Suction tube should be with drawn
using a rotational technique NOT
pistoning
• 5-10 second suction time
Endotracheal suctioning
Rotational motion for 5-10 second suction then 10 sec rest. Anything longer makes them hypoxic.


