Cardiac/Circulaton Flashcards
MEDICAL ARREST DIRECTIVE - COND

MEDICAL ARREST DIRECTIVE - CONT

MEDICAL ARREST DIRECTIVE - Tx

MEDICAL ARREST DIRECTIVE - Tx (3)

MEDICAL ARREST DIRECTIVE - Tx (2)

MEDICAL ARREST DIRECTIVE - Tx (4)

MEDICAL ARREST DIRECTIVE - CONSIDERATIONS
The initial rhythm interpretation/analysis and defibrillation should be performed as soon as possible. Following the initial rhythm interpretation/analysis, additional rhythm interpretations/analyses should occur at two (2) minute intervals with a focus on the delivery of high quality chest compressions.
The energy settings used for defibrillation typically follow specific manufacturer guidelines and are supported by each respective RBH program.
As a general rule, Paramedics do NOT count pre-arrival interventions into their patient care. Care delivered prior to arrival can be “considered” and documented. However, in the setting of cardiac arrest where a medical TOR might apply, the Paramedics will complete three (3) rhythm interpretations themselves rather than “count” the number completed prior to their arrival.
In all cardiac arrest directives, manual defibrillation has been moved ahead of AED defibrillation in keeping with the preferred treatment being listed first.
Compressions during the charge should be considered to minimize the peri-shock pause.
When en-route and using manual interpretation, the ambulance should be stopped to minimize artifact and the risk of an inaccurate rhythm.
When en-route and using semi-interpretation, the ambulance must be stopped to minimize artifact and the risk of an inaccurate rhythm.
Supraglottic Airways (SGA):
The sequence listed for the advanced airways is deliberate, and based on:
- The reduced importance on the airway as outlined AHA
- The ease of supraglottice airway insertion vs. the complexity and risks of intubation.
- The emphasis placed on minimally interrupted compressions.
and does not preclude the ACP from placing an Endotracheal Tube (ETT) when there is airway compromise of in a prolonged resuscitation. Intubation should normally not require compressions to be stopped or altered as any pause in compressions can lead to a poor outcome.
Once the ETT or supraglottic airway is placed, compressions should be continuous and ventilations provided asynchronously as a rate of 10 breaths/minute (one [1] every six [6] seconds).
Amiodarone:
Is the preferred antiarrhythmic medication if an alternate is available. This is demonstrated in the directive by the preferred medication being listed first.
Lidocaine:
Dosing (reference to weight and age) has been simplified.
Antiarrhythmic Administration:
Is Indicated in VF and pulseless VT that is refractory or recurrent following defibrillation.
Is indicated (if not previously maxed out) following the shock if the patient has been previously defibrillated or following a second defibrillation if none delivered previously.

TRAUMA ARREST DIRECTIVE - COND

TRAUMA ARREST DIRECTIVE - CONT

TRAUMA ARREST DIRECTIVE - TX

TRAUMA ARREST DIRECTIVE - COMPANION DOCUMENT
Fluid bolus is not listed in the directive and is not indicated.
The age difference between Medical and Truama TOR reflects the accepted definiftion of a pediatric trauma patient.
The 30 minute time reference is a reflection of transportation time and is relevant only in a PEA rhythms.
The flow chart had been updated to reflect the 2015 AHA guidelines.
HYPOTHERMIC VSA
IND - CON - CONT

HYPOTHERMIC VSA - TX

HYPOTHERMIC VSA - COMPANION DOCUMENT
Pulse check:
The specific reference to a prolonged pulse check was removed because the AHA guidelines advocate for a 10 second pulse check.
When treating the hypothermic arrest, the focus is on passive rewarming and gentle handling. Epinephrine is not indicated in this setting.
The expectation is that these patients will be transported. The old adage says that “the patient is not dead until they are warm and dead”
FBAO - IND - CON - CONT

FBAO - TX

FBAO - COMPANION DOCUMENT
NEONATE - IND / C&C

NEONATE - TX
Cardiac and pulse ox

NEONATE -CD

NEONATE CD 2

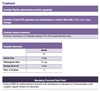
ROSC IND / C&C

ROSC - TX
12 lead & transport in parallel.

ROSC DOPAMINE DRIP SHEET