Calcium Flashcards
(87 cards)
roles of calcium in the body
muscle contraction
transmission of nerve impulses
blood clottin
indirect action of PTH on the kidney
Inc the circulating VitD which inc the protein Calbindin which helps in the transport of Ca across the cell to the basolateral membrane, where it is secreted back into the circulation

diffusible vs non diffusible calcium?
nondiffusible - bound to protein - can’t be filtered by the kidney
diffusible - not bound to protein (ionized and complexed)

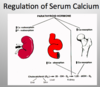
action of PTH on Vit D
PTH Also regulates the conversion of Vit D3 to its active form (1,25 DH Vit D) by activating the enzyme that catalyzes the conversion in the Kidney;
This active Vit D in turn facilitates increased absorption of Ca from the intestine(GIT). Thus Vit D facilitates utilization of Ca that we eat.

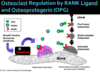
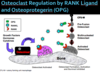
process of bone remodeling
Two important cells:
Osteoclasts: bone breakdown cell which is derived from a hematopoietic cell
Osteoblasts: bone formation cell, deriving from mesenchymal cells.
It’s a question of how much formation and how much breakdown that is going to determine what’s going on.

bone quality
architecture, turnover, damage accumulation, mineralization
indications for teriparatide
consider first therapy (2 years) followed by a bisphosphonate
severe osteoporosis (estabilshed and risk factors/prior fractures)
failed/intolerant of bisphosphonates)
what if PTH is high and 24h Ca is high?
primary hyperparathyroidism

blood supply to parathyroid glands?
thyroid arteries

Where is most of the calcium found in the body?
skeleton (99%)
lithium and calcium
lithium can cause hyperparathyroidism and decreased Ca

FRAX
to calculate 10 year probability ofhip fracture - takes many things into acct
bone densitiy and risk factors
intestinal Ca absorption?
With Calbindin (activated by Vit D)

where is vit D activated? How?
liver then kidney
Source-Diet or the Sun (UV light converts Vit D to active form)- Dietary 7 – dehdr cholesterol can be converted to Vit D via hydroxylation(25 hydroxy-D) (happens in the Liver) – This is still inactive à in the kidney à Hydroxylated at 25 or 24 position. If hydroxylated at the 25- its active
But if Ca/PO4 excess, it gets hydroxylated at the 24 position-leads to Inactive VIT D-Not usable/not available for activation; Points to the active form on the slide

central DXA
bone density measurement
It’s a really simple test with very low radiation, very easily done by a tech with experience.
Do the spine and do the hip (2 readings on the hip)
We only do the forearm where we think cortical bone will be more effected in a disease such a hyperparathyroidism, but otherwise we focus on the spine and the hip to get a risk profile in terms of their bone density.
The important think about DEXA’s are, in the spine if someone has significant arthritis or spinal abnormality (which you certainly will see in a lot of older people) then it may interfere and you may need to focus more on the hip reading.
Central DXA Measurement
•Dual x-ray absorptiometry (DXA) can be used to measure BMD at multiple skeletal sites, including spine, proximal femur, forearm, and total body.
–Uses x-rays of 2 different energy levels to distinguish bone from
soft tissue
–Advantage of being able to measure BMD of the central and most osteoporotic fracture-prone sites, the spine and hip
•DXA can be performed in the office. Scanning time is less than 5
minutes and the radiation dose is considerably lower than that for
conventional radiography.
•DXA has good overall accuracy and precision.
–Reproducible results make it useful for both baseline and
follow-up measurements.
–DXA has been used in most of the prospective epidemiologic
studies investigating the BMD/fracture risk relationship.
What is the activated Vit D?
1, 25
Source-Diet or the Sun (UV light converts Vit D to active form)- Dietary 7 – dehdr cholesterol can be converted to Vit D via hydroxylation(25 hydroxy-D) (happens in the Liver) – This is still inactive à in the kidney à Hydroxylated at 25 or 24 position. If hydroxylated at the 25- its active
But if Ca/PO4 excess, it gets hydroxylated at the 24 position-leads to Inactive VIT D-Not usable/not available for activation

chvostek’s sign
sign of hypocalcemia
tap the face at a point –> twitch
sign of neuromuscular excitability caused by hypocalcemia

where is the first activation step of Vit D?
liver

Treatment in hyperparathyroidism?
parathyroidectomy
based on CT scan (min invasive)
if decrease PTH by 50% during surgery - got it!
what happens if calcium levels are too low>
parathyroid releases PTH
increase Ca release from bones
increase Ca uptake in intestines
Increase Ca reabsorption from urine
calcium levels rise
Zoledronic Acid
IV bisphosphoate
1) Some patients have GI intolerance or think they have GI intolerance and can’t tolerate or won’t take these drugs.
2) And also it’s clear that some patients actually don’t take them. If you do these studies and see how many patients that are sent home with them actually take them. Large studies, not in a specialty practice like mine, but in a general medicine practice a lot of patients don’t take it.
So that’s where the IV drug comes – the patient who is intolerant of the oral one or someone where we’re concerned they’re not actually going to take the oral one.
●
Given through butterfly as an IV infusion once per year. It’s a long acting, potent bisphosphonate.
Vit D precursor from the sun?
7-dehydrocholesterol –> cholecalciferol

Calcitonin
secreted by C cells of the thyroid
lowers plasma calcium (can give exogenous)
stimulated by increase in plasma Ca, gastrin f

gene in familal hypocalciuric hypercalcemia?
CASR gene