Block I: General Flashcards
sterile areas in the body (no association with bacteria)
-CSF, blood, lung, deep tissue
general mechanisms of antibiotic resistance
- de novo mutations causing antibioitc resistant traits
- transfer of preexisting resistant genes from the environment
- transver between bacteria (mobile DNA elements & horizontal DNA transfer)
Peptidoglycan
major feature of cell walls of bacteria
- gram-positives: thick peptidoglycan layers
- gram-negatives: thin peptidoglycan layers
**target for many abx because humans do not have peptidoglycans
- gives osmostic stability to cell (when acted on by abx, cells lose osmotic stability & lyse)
- consists of polysaccarhide chains crosslinked by peptide bridges
- subunit: disaccharide with peptide tail; peptide crossbridge attaches to peptide tail
- synthesized in cytoplasm, then transferred to membrane to rane, then to the cell wall
bacteria classification: presence of specific enzymes
- ex) catalase: if a bacteria has catalase, it will create bubbles when treated with peroxide (as it detoxifies reactive oxygen species)
- can also look for presence of: oxidase, urease, coagulase, hemolysin
**enzyme presence is diagnostic/identifying for a bacteria (but not used to classify virulence)
nomenclature of bacteria
genus species
(genus then species in italics)
Gram-negative rods
pseudomonas
vibrio
enteric: escherichia coli
obligate intracellular parasites: rickettsia, chlamydia
characteristics of the “perfect antibiotic”
- selective (for bacteria)
- specific
- lethal
AB Toxins
(exotoxins that act intracellularly)
- A subunit: active subunit that is responsible for enzymatic activity that affects host physiology
- B subunit: binding subunit that delivers the A subunit & determines which cell types are affected (binds to cell surface receptors)
Ways to distinguish AB toxins:
- potency (very toxic)
- ability to mimic infection
ex) Anthrax toxin is a model of AB toxin translocation
gram stain
1- stain with crystal violet (purple)
2- fix stain with potassium iodide
3-decolorize with alcohol (gram positives remain purple)
4- counterstain with safranin (gram negatives become pink)
benefits of the normal flora
- provide nutrients
- stimulate the immune system (espeically in the gut)
- compete with pathogens
(germ-free animals are much more susceptible to colonization by intestinal pathogens)
How do macrophages recognize LPS?
- LPS receptor complex (CD14, Toll-like receptor 4, MD2)
- -CD14= LPS binding portion (protein on surface, grabs LPS out o fsystem)*
- **if antibodies to CD14 inhibit inflammation induced by LPS and gram-negative bacteria*
(immune mediated tissue disease) acute local tissue damage
- local inflammation impairs tissue function
- edema
- neutrophil recruitment & activation
-
exotoxins that act on ECM
(extracellular)
- attack/bind to ECM rather than to host cell itself
- Staphylococcal scalded skin syndrome (SSSS)– toxin disrupts epithelial tight junctions by degrading desmosome components
- also: collagenases, elastases, hyaluronidases, DNAses, streptokinase
transpeptidation of peptidoglycan in bacterial cell wall
- when glycan chains are crosslinkjed to each other, losing the terminal D-alanine
- transpeptidation occurs in both gram positives and negatives, although the gram negative peptidoglycan structure differes soemwhat
**B-Lactam abx inhibit transpeptidation
synergy
when 2 antibiotics work better together than separately
(often bactericidal)
current therapy for sepsis
- immediate stabilization (ABCs)
- obtain initial database
- obtain appropriate cultures
- prompt use of antimicrobial agents (consider drainage/surgical drainage)
- idtenify & manage organ dysfunction
FLUIDS
monoclonal
cultured bacteria that consist of genetically identical individuals descended from a single ancestor
minimum bactericidal concentration (MBC)
minimum concentration of drug that kills the bacteria
Bacteria Capsule Histo

major factors that contribute to antimicrobial resistance epidemic in bacteria
1-non-prescription antibiotic use (creates strong environmental selection pressure)
-animal feeds, easy access to abx in developing countries, antibacterials present in household cleaners
2- misuse of abx
-lack of stewardship, noncompiance in patients
3-poor santiation (puts bacteria into environment)
4-lack of new abx in drug development pipeline
how bacteria overcome the innate defense of phagocytosis
- thick polysaccharide capsules
- resist lysosomal killing by growing within the phagolysosome
- prevent phagolysosome fusion, so that can’t be degraded
- escape from phagosome
-
transposition
(process of gene transfer within an organism)
- via transposons: small DNA elements that can cut themselves out of sequence and add themselves in elswehere
- transposons often carry additional genes to ensure their survivial– leading to abx resistance
critical microbial products involved in sepsis
gram negative: LPS, DNA
gram positive: protein toxins, lipotheichoic acid, lipoproteins, peptidoglycan
**gram positive and gram negative sepsis can not be distinguished clinically
elements of antimicrobial therapy
- selective toxicity of the agent
- susceptibility of the pathogen to the agent
- effective concentration at the site of infection
- maintenance of effective concentration for sufficient time
- side effects
phagocytosis as an innate defense in deep tissue/blood
- neturophils, monocytes, macrophages are all involved in phagocytosis
- phagocytes are recrutied during the inflammatory response
influx and efflux of gram negative bacteria
- in gram negatives, there is the inner membrane and outer membrane (serving as 2 checkpoints for any influx or efflux_
- outer membrane has porins: semi-selective energy-independent channels
- inner membrane has transporters/pumps
**these checkpoints control drug uptake & efflux into bacteria (effectiveness of abx)
chemotaxis
- important function of motility
- movement in response to chemical stimulus (attractants are bacteria that swim up concentration gradients, repellents swim down gradients)
Superantigens
(exotoxins that work extracellularly)
- bind to TCR and MHC outside of peptide-binding grooves, resulting in activation of all T-cells with a certain domain –> causing massive release of cytokines
ex) staphylococcal TSS
macrophage vs monocyte
- both are phagocytes
- longer-lived than neutrophils
- macrophages: in tissues
- monocytes: in circulation
(immune mediated tissue disease) chronic local tissue damage
-chronic inflammation eventually results in displacement of tissue cells with leukocytes & fibrin
what is a bacterium?
- microscopic
- haploid
- anucleate
- prokaryotic
mechanisms of bacterial pathogen damage to host
-either immune-mediated (collateral damage resulting from immune activation by bacteria; can be due to either innate or adaptive immune responses)
OR
-toxin-mediated damage (damage resulting from product of bacteria)
the human microbiome(s)
- composition of microbiome varies in different areas of the body
- mouth, skin, colon, esophagus, stomach, vagina
selective toxicity of an antimicrobial
STRATEGIES:
- lack of target in human host
- difference in target sensitivity
- differential concentration of antibiotic by bacterial & human cells
steps required of a bacterium to cause disease
1- encounter & enter host
2-establish an infectious niche
3- multiply, cause tissue damage
4-spread to other tissues, hosts, or both
blood agar
- medium containing RBCs
- frequently used for throat cultures
- hemolysins present (lyse RBCs) in host, and type of hemolysis seen in the blood agar is useful for distinguishing different species of streptococci
minimum inhibitory concentration (MIC)
-mimimum concentration of a drug that inhibits a bacteria
SOS response
- if a cell is exposed to DNA damage, it triggers RecA protein to be active, which induces mutations (under stress)
AB toxins that modulate cAMP levels intracellularly
- cholera & pertussis toxins: ADP-ribosylate G proteins–> actiavtion of adenylate cyclase
- anthrax EF toxin & pertuss AC toxins: adenylate cyclase enzymes
- increase cAMP: increases fluid secretion from epithelial cells, inhibits phagocyte chemotaxis & effector functions
Gram negative cocci
neisseria
& others
How to categorize microbes?
- phylogeny (based on 16S RNA)
- structure (shape & stain)
- nature of interaction with host (symbiosis, commensalism, parasitism)
- pathogenic strategies
sedementation coefficients (refers to molecular weight) of bacteria bacterial ribosomes
70S
-made of 2 subunits; in bacteria: 30S and 50S
direct detection method of diagnosing infection
- DNA or microbial antigen detection
- very specific & sensitive
- tests not always available
replisome
origin of DNA replication in bacteria
Phase Variation
-phase variation results in phenotypic heterogeneity in an organism
**important to vary antigens in host
-evade host defenses, adapt to different niches
mechanisms:
slipped strand mispairing
site-specific recombination
epigenetic regulation mediated by DNA methylation
therpeautic index
- ratio of the minimum toxic dose to the minimum effective dose
- this ratio must be >1 for an abx to be of use
**high therapeutic index= not generally toxic to patients
Gram-Negative Bacteria (structure)
- inner membrane (inside cell wall, consists of phospholipid)
- outer membrane (outside cell wall, consists of phospholipis & lipopolysaccharide LPS)
- LPS is the endotoxin of gram negative baceria (pathogenesis)
- 2 types of protein in outer membrane: porin & lipoprotein
how many toll-like receptors do humans have?
10
gram-positive cocci
staphylococcus
streptococcus
enterococcus
epidemiology of sepsis
- more common among men
- more common among nonwhite
- gram-positive more positive than gram-negative
colloquial name for streptococcus pneumoniae
pneumococcus
sepsis
formal definition: alterations in physiology (fever, respiratory rate, blood pressure, organ function)
accompanied by an infection
-life-threatening condition that arises when the body’s response to an infection injures its own tissues & organs
(local infection with profound systemic response)
-sepsis can be mimicked by other non-infectious disorders
transduction
(process of horizontal gene transfer between organisms)
- agent: phage (viruses that infect bacteria)
- virulent phages: replicate within host cell, then destory host, releasing infectioius virions
- temperate phages: replicate lytically or go latent
generalized transduction: phages with nonspecific DNA encapsulation package host DNA instead of phage DNA during lytic growth– then can inject DNA into new cell
specialized transduction: when bacterial genes transferred from one cell to another by becoming incorporated into a phage chromosome (phage uses SOS response to induce replication, then find a new host after excising itself)
teichoic acid
- polymer of ribitol-phosphate or glyercol-phosphate
- part of gram positive cell walls, confers stability of the peptidoglycan
- not yet used as target for abx
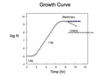
what kind of growth is characteristic of microbial growth?
- exponential growth: every cell takes the same amount of time to complete a binary fission event
- a limitation of exponential growth is having enough nutrition for this growth
- log phase cells show most consistent physiological parameter (so are the standard for most experiments in microbio)
why are bacitracin and vancomycin’s mechanisms unique?
they both bind to microbial metabolites rather than inhibiting an enzyme
gyrase & topoisomerase
- maintain the supercoiling of bacterial DNA
- recognize improperly coiled DNA and fix it
**protein-bound DNA is good target for antibioics (quinolones & fluoroquinolones)
EARLY GOAL-DIRECTED THERAPY (EGDT) for sepsis
-administration of IV fluids within the first 6 hours of presentation
bacteria classification: interaction with oxygen
- anaerobic: grow in oxygen-free environment
- obligate anaerobe: killed by oxygen (often form spores so that they can spread in environment)
- facultative anaerobe: can live in aerobic or anaerobic environment
- aerobic: grow in oxygen-containing environment
- obligate aerobe: need oxygen to grow
- some are “microaerophilic”- they ferment (metabolism without oxygen) for energy, but can grow in contact with oxygen at less than atmospheric pressure
4 categories of Immune-mediated tissue disease after bacterial infection
1- acute local damage
2-chronic local damage
3-acute systemic disease
4-chronic systemic disease
How do bacteria resist B-lactam antibiotics?
-they produce beta lactamase, which breaks down the B-lactam ring in the abx, making it ineffective
Spirochetes
treponema
borrelia
shapes of bacteria
- bacillus: rod
- coccus: sphere
- coccobacillus (oval)
- comma (vibrio)
- helical (spirochete)