Block 6 Flashcards
Innervation of pec major
Lateral pectoral nerve
Action of pec major
Adductor and medial rotator of humerus
Which of the following methods is most effective at destroying spores of the tubercle bacilli?
Immersion in 0.5% chlorhexidine in alcohol
Immersion in aqueous iodine
Heating in a hot air oven
Immersion in 0.1% sodium hypochlorite
Autoclaving
The tubercle bacilli has a waxy outer membrane that renders it more resistant to sterilisation and cleaning methods. Whilst 0.1% sodium hypochlorite will destroy many microbes it is less reliable in destroying tubercle bacilli. Hot air ovens provide less reliable pathogen destruction than autoclaving, but may be indicated in situations where the equipment is sensitive to the autoclaving process. From the list of options above, autoclaving will most reliably destroy tubercle bacilli.
Def: cleaning
Removal of physical debris
Def: disinfection
Reduction in number of viable organisms
Sterilisation
Removal of all organisms and spores
Sterilisation technique options
Autoclaving
Glutaraldehyde solution
Ethylene oxide
Gamma irradiation
A 59 year old man is undergoing an extended right hemicolectomy for a carcinoma of the splenic flexure of the colon. The surgeons divide the middle colic vein close to its origin. Into which of the following structures does this vessel primarily drain?
Superior mesenteric vein
Portal vein
Inferior mesenteric vein
Inferior vena cava
Ileocolic vein
The middle colonic vein drains into the SMV, if avulsed during mobilisation then dramatic haemorrhage can occur and be difficult to control.
A 65 year old male with known nasopharyngeal carcinoma presents with double vision over a few weeks. On examination he is found to have left eye proptosis and it is down and out. He reports pain on attempting to move the eye. There is an absent corneal reflex. What is the most likely diagnosis?
Posterior communicating artery aneurysm
Cavernous sinus syndrome
Optic nerve tumour
Migraine
Cerebral metastases
Cavernous sinus syndrome is most commonly caused by cavernous sinus tumours. In this case, the nasopharyngeal malignancy has locally invaded the left cavernous sinus. Diagnosis is based on signs of pain, opthalmoplegia, proptosis, trigeminal nerve lesion (opthalmic branch) and Horner’s syndrome.
Medial relations of the cavernous sinus
Pituitary fossa
Sphenoid sinus
Lateral relations of the cavernous sinus
Temporal bone

Lateral wall components of the cavernous sinus
(from top to bottom:)
Oculomotor nerve
Trochlear nerve
Ophthalmic nerve
Maxillary nerve
Contents of the cavernous sinus
(from medial to lateral:)
Internal carotid artery (and sympathetic plexus)
Abducens nerve
Blood supply of the cavernous sinus
Ophthalmic vein, superficial cortical veins, basilar plexus of veins posteriorly.
Drains into the internal jugular vein via: the superior and inferior petrosal sinuses
In patients with an annular pancreas where is the most likely site of obstruction?
The first part of the duodenum
The second part of the duodenum
The fourth part of the duodenum
The third part of the duodenum
The duodeno-jejunal flexure
The pancreas develops from two foregut outgrowths (ventral and dorsal). During rotation the ventral bud and adjacent gallbladder and bile duct lie together and fuse. When the pancreas fails to rotate normally it can compress the duodenum with development of obstruction. Usually occurring as a result of associated duodenal malformation. The second part of the duodenum is the commonest site.
Theme: Chest pain
A.Achalasia
B.Pulmonary embolus
C.Dissection of thoracic aorta
D.Boerhaaves syndrome
E.Gastro-oesophageal reflux
F.Carcinoma of the oesophagus
G.Oesophageal candidiasis
Please select the most likely cause for chest pain for the scenario given. Each option may be used once, more than once or not at all.
41.A 43 year old man who has a long term history of alcohol misuse is admitted with a history of an attack of vomiting after an episode of binge drinking. After vomiting he developed sudden onset left sided chest pain, which is pleuritic in nature. On examination he is profoundly septic and drowsy with severe epigastric tenderness and left sided chest pain.
A 22 year old man is admitted with severe retrosternal chest pain and recurrent episodes of dysphagia. These occur sporadically and often resolve spontaneously. On examination there are no physical abnormalities and the patient seems well.
An obese 53 year old man presents with symptoms of recurrent retrosternal discomfort and dyspepsia. This is typically worse at night after eating a large meal. On examination there is no physical abnormality to find.
Boerhaaves syndrome
In patients with Boerhaaves the rupture is often on the left side. The story here is typical. All patients should have a contrast study to confirm the diagnosis and the affected site prior to thoracotomy.
Achalasia
Achalasia may produce severe chest pain and many older patients may undergo cardiac investigations prior to endoscopy.
Endoscopic injection with botulinum toxin is a popular treatment (although the benefit is not long lasting). Cardiomyotomy together with an antireflux procedure is a more durable alternative.
Gastro-oesophageal reflux
Patients with GORD often have symptoms that are worse at night. In this age group an Upper GI endoscopy should probably be performed.
Tearing interscapular pain
Discrepancy in arterial blood pressures taken in both arms
May show mediastinal widening on chest x-ray
Dissection of thoracic aorta
Spectrum of oesophageal motility disorders
Caused by uncoordinated contractions of oesphageal muscles
May show “nutcracker oesophagus” on barium swallow
Symptoms include dysphagia, retrosternal discomfort and dyspepsia
Diffuse oesophageal spasm
Common cause of retrosternal discomfort
Usually associated with symptoms of regurgitation, odynophagia and dyspepsia
Symptoms usually well controlled with PPI therapy
Risk factors include obesity, smoking and excess alcohol consumption
Gastro-oesphageal reflux
Spontaneous rupture of the oesophagus
Caused by episodes of repeated vomiting often in association with alcohol excess
Typically there is an episode of repetitive vomiting followed by severe chest and epigastric pain
Diagnosis is by CT and contrast studies
Treatment is surgical; during first 12 hours primary repair, beyond this usually creation of controlled fistula with a T Tube, delay beyond 24 hours is associated with fulminent mediastinitis and is usually fatal.
Boerhaaves syndrome
Difficulty swallowing, dysphagia to both liquids and solids and sometimes chest pain
Usually caused by failure of distal oesphageal inhibitory neurones
Diagnosis is by pH and manometry studies together with contrast swallow and endoscopy
Treatment is with either botulinum toxin, pneumatic dilatation or cardiomyotomy
Achalasia
Theme: Nerve Injury
A.Median nerve
B.Ulnar nerve
C.Radial nerve
D.Musculocutaneous nerve
E.Axillary nerve
F.Anterior interosseous nerve
G.Posterior interosseous nerve
For each scenario please select the most likely underlying nerve injury. Each option may be used once, more than once or not at all.
44.A 10 year old boy is admitted to casualty following a fall. On examination there is deformity and swelling of the forearm. The ability to flex the fingers of the affected limb is impaired. However, there is no sensory impairment. Imaging confirms a displaced upper forearm fracture
A well toned weight lifter attends clinic reporting weakness of his left arm. There is weakness of flexion and supination of the forearm.
An 18 year old girl sustains an Holstein-Lewis fracture. Which nerve is at risk?
Anterior interosseous nerve
Forearm fractures may be complicated by neurovascular compromise. The anterior interosseous nerve may be affected. It has no sensory supply so the defect is motor alone.
Musculocutaneous nerve
Musculocutaneous nerve compression due to entrapment of the nerve between biceps and brachialis. Elbow flexion and supination of the arm are affected. This is a rare isolated injury.
Radial nerve
Proximal lesions affect the triceps. Also paralysis of wrist extensors and forearm supinators occur. Reduced sensation of dorsoradial aspect of hand and dorsal 31/2 fingers. Holstein-Lewis fractures are fractures of the distal humerus with radial nerve entrapment.
Location of brachial plexus roots?
Posterior triangle
Passage of the brachial plexus roots
Between scalenus anterior and medius
Location of brachial plexus trunks
Posterior to middle third of clavicle.
Relationship of the upper and middle third trunks to the subclavian artery?
Superior
Relation of the lower brachial plexus trunk to the subclavian artery
Posterior
Where are the divisions of the brachial plexus?
Apex of axilla
Draw the brachial plexus
https://www.youtube.com/watch?v=Z_Y_kVdH9zE
A 44 year old man recieves a large volume transfusion of whole blood. The whole blood is two weeks old. Which of the following best describes its handling of oxygen?
It will have a low affinity for oxygen
Its affinity for oxygen is unchanged
It will more readily release oxygen in metabolically active tissues than fresh blood
The release of oxygen in metabolically active tissues will be the same as fresh blood
It will have an increased affinity for oxygen
Stored blood has less 2,3 DPG and therefore has a higher affinity for oxygen, this reduces its ability to release it at metabolising tissues.
Haldane effect?
Left shit- increased saturation of Hb with oxygen for given O2 tension i.e. reduced delivery to tissue
Bohr shift
Shifts to right = for given oxygen tension there is reduced saturation of Hb with oxygen i.e. Enhanced oxygen delivery to tissues
Factors causing haldane effect
HbF, methaemoglobin, carboxyhaemoglobin
low [H+] (alkali)
low pCO2
low 2,3-DPG
low temperature
Factors causing Bohr effect
raised [H+] (acidic)
raised pCO2
raised 2,3-DPG*
raised temperature
A 32 year old male is receiving a blood transfusion after being involved in a road traffic accident. A few minutes after the transfusion he complains of loin pain. His observations show temperature 39 oC, HR 130bpm and blood pressure is 95/40mmHg. What is the best test to confirm his diagnosis?
USS abdomen
Direct Coomb’s test
Blood cultures
Blood film
Sickle cell test
The diagnosis is of an acute haemolytic transfusion reaction, normally due to ABO incompatibility. Haemolysis of the transfused cells occurs causing the combination of shock, haemoglobinaemia and loin pain. This may subsequently lead to disseminated intravascular coagulation. A Coomb’s test should confirm haemolysis. Other tests for haemolysis include: unconjugated bilirubin, haptoglobin, serum and urine free haemoglobin.
Note that delayed haemolytic reactions are normally associated with antibodies to the Rh system and occur 5-10 days after transfusion.
A 42 year old female presents with symptoms of biliary colic and on investigation is identified as having gallstones. Of the procedures listed below, which is most likely to increase the risk of gallstone formation?
Partial gastrectomy
Jejunal resection
Liver lobectomy
Ileal resection
Left hemicolectomy
Bile salt reabsorption occurs at the ileum. Therefore cholesterol gallstones form as a result of ileal resection.
Theme: Management of skin lesions
A.Excision biopsy
B.Excision with 0.5 cm margin
C.Excision with 2 cm margin
D.Shave biopsy and cautery
E.Punch biopsy
F.Excision and full thickness skin graft
G.Discharge
For each skin lesion please select the most appropriate management option. Each option may be used once, more than once, or not at all.
2.A 22 year old women presents with a newly pigmented lesion on her right shin, it has regular borders and normal appearing dermal appendages. However, she reports a recent increase in size.
A 58 year old lady presents with changes that are suspicious of lichen sclerosis of the perineum.
A 73 year old man presents with a 1.5cm ulcerated basal cell carcinoma on his back.
Excision biopsy
Lesion bearing normal dermal appendages and regular borders are likely to be a benign pigmented naevi. Therefore diagnostic and not radical excision is indicated.
Punch biopsy
Punch biopsies are a useful option for obtaining a full thickness tissues sample with minimal tissue disruption. In this situation the other differential would be AIN or VIN and punch biopsies would be useful in distinguishing thes
Excision with 0.5 cm margin
A small lesion such as this is adequately treated by local excision. The British Association of Dermatology guidelines suggest that excision of conventional BCC (<2cm) with margins of 3-5mm have locoregional control rates of 85%. Morpoeic lesions have higher local recurrence rates.
When should UFH be considered in PE?
(a) as a first dose bolus, (b) in massive PE, or (c) where rapid reversal of effect may be needed.
Management of massive PE with cardiovascular compromise
Thrombolysis is 1st line for massive PE (ie circulatory failure) and may be instituted on clinical grounds alone if cardiac arrest is imminent; a 50 mg bolus of alteplase is recommended.
Invasive approaches (thrombus fragmentation and IVC filter insertion) should be considered where facilities and expertise are readily available.
A 32 year old man is diagnosed as having a carcinoma of the caecum. On questioning, his mother developed uterine cancer at the age of 39 and his maternal uncle died from colonic cancer aged 38. His older brother developed a colonic cancer with micro satellite instability aged 37. What is the most appropriate operative treatment?
Limited ileocaecal resection
Right hemicolectomy
Extended right hemicolectomy
Panproctocolectomy
Sub total colectomy
Panproctocolectomy
The likely diagnosis is one of a familial cancer syndrome and now that he has developed a colonic cancer the safest operative strategy is a total colectomy and end ileostomy.
A laceration of the wrist produces a median nerve transection. The wound is clean and seen immediately after injury. Collateral soft tissue damage is absent. The patient asks what the prognosis is. You indicate that the nerve should regrow at approximately:
0.1 mm per day
1 mm per day
5 mm per day
1 cm per day
None of the above
Transection of a peripheral nerve results in hemorrhage and retraction of the severed nerve ends. Almost immediately, degeneration of the axon distal to the injury begins. Degeneration also occurs in the proximal fragment back to the first node of Ranvier. Phagocytosis of the degenerated axonal fragments leaves neurilemmal sheath with empty cylindrical spaces where the axons were. Several days following the injury, axons from the proximal fragment begin to regrow. If they make contact with the distal neurilemmal sheath, regrowth occurs at about the rate of 1 mm/day. However, if associated trauma, fracture, infection, or separation of neurilemmal sheath ends precludes contact between axons, growth is haphazard and a traumatic neuroma is formed. When neural transaction is associated with widespread soft tissue damage and hemorrhage (with increased probability of infection), many surgeons choose to delay reapproximation of the severed nerve end for 3 to 4 weeks.
Seddon classification of nerve injury
Neuropraxia
Axonotmesis
Neurotmesis
Neuropraxia
Nerve intact but electrical conduction is affected
Full recovery
Autonomic function preserved
Wallerian degeneration does not occur
Axonotmesis
Axon is damaged and the myelin sheath is preserved. The connective tissue framework is not affected.
Wallerian degeneration occurs.
Neurotmesis
Disruption of the axon, myelin sheath and surrounding connective tissue.
Wallerian degeneration occurs.
Axonal degeneration distal to the site of injury.
Typically begins 24-36 hours following injury.
Axons are excitable prior to degeneration occurring.
Myelin sheath degenerates and is phagocytosed by tissue macrophages.
Wallerian Degeneration
Theme: Head injury
A.Subdural haematoma
B.Extradural haematoma
C.Subarachnoid haemorrhage
D.Basal skull fracture
E.Intracerebral haematoma
F.Le fort 1 fracture of maxilla
G.Le fort fracture 3 affecting maxilla
H.Mandibular fracture
What is the most likely diagnosis for the scenario given? Each option may be used once, more than once or not at all.
9.A 32 year old female hits her head on the steering wheel during a collision with another car. She has periorbital swelling and a flattened appearance of the face.
A 29 year bouncer is hit on the side of the head with a bat. He now presents to A&E with odd behaviour and complaining of a headache. Whilst waiting for a CT scan he becomes drowsy and unresponsive.
A 40 year old alcoholic presents with worsening confusion over 2 weeks. He has weakness of the left side of the body.
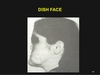
Le fort fracture 3 affecting maxilla
The flattened appearance of the face is a classical description of the dish/pan face associated with Le fort fracture 2 or 3 of the maxilla.
Extradural haematoma
The middle meningeal artery is prone to damage when the temporal side of the head is hit.
Note that there may NOT be any initial LOC or lucid interval
Subdural haematoma
Subdural haematomas can have a history over weeks/months. It is common in alcoholics due to cerebral atrophy causing increased stretching of veins.
ICP monitoring in head injury
GCS 3-8 with normal CT scan is appropriate
Mandatory in those with abnormal CT scan
What is minimal CPP in adults?
70mmHg in adults
40-70 in children
Management of depressed skull fractures
Depressed skull fractures that are open require formal surgical reduction and debridement, closed injuries may be managed non operatively if there is minimal displacement.
Main component of colloid.
Thyroglobulin
It is high molecular weight protein that acts as a storage form of thyroid hormones.
Which of the following is not true of hyper acute solid organ transplant rejection?
It may occur during the surgical procedure itself.
May occur as a result of blood group A, B or O incompatibility.
May be due to pre existing anti HLA antibodies.
On biopsy will typically show neo intimal hyperplasia of donor arterioles.
Complement system activation is one of the key mediators.
On biopsy will typically show neo intimal hyperplasia of donor arterioles.
These changes are more often seen in the chronic setting. Thrombosis is more commonly seen in the hyperacute phase.
Theme: Management of abdominal aortic aneurysms
A.Immediate laparotomy
B.Immediate CT
C.AAA repair during next 48 hours
D.USS in 6 months
E.CT scan during next 4 weeks
F.Endovascular aortic aneurysm repair
G.Discharge
H.Palliate
I.None of the above
Please select the most appropriate management for the scenario given. Each option may be used once, more than once or not at all.
16.A 66 year old man is referred via the aneurysm screening programme with an abdominal aortic aneurysm measuring 4.4 cm. Apart from well controlled type 2 DM he is otherwise well
A 72 year old man has a CT scan for abdominal discomfort and the surgeon suspects AAA. This shows a 6.6cm aneurysm with a 3.5cm neck and it continues to involve the right common iliac. The left iliac is occluded. He is hypertensive and has Type 2 DM which is well controlled.
An 89 year old man presents with hypotension and collapse and is found by the staff in the toilet of his care home. He is moribund and unable to give a clear history. He had suffered a cardiac arrest in the ambulance but has since been resuscitated and now has a Bp of 95 systolic. He has an obviously palpable AAA.
USS in 6 months
At this point continue with ultrasound surveillance
AAA repair during next 48 hours
Assuming he is fit enough. This would be a typical ‘open ‘ case as the marked iliac disease would make EVAR difficult
Palliate
He will not survive aortic surgery and whilst some may disagree, I would argue that taking this case to theatre would be futile
Difference between true and false aneurysm
They may occur as either true or false aneurysm. With the former all 3 layers of the arterial wall are involved, in the latter only a single layer of fibrous tissue forms the aneurysm wall.
Epidemiology of AAA
True abdominal aortic aneurysms have an approximate incidence of 0.06 per 1000 people. They are commonest in elderly men and for this reason the UK is now introducing the aneurysm screening program with the aim of performing an abdominal aortic ultrasound measurement in all men aged 65 years.
Causes of AAA
The commonest group is those who suffer from standard arterial disease, i.e. Those who are hypertensive and have been or are smokers.
Other patients such as those suffering from connective tissue diseases such as Marfan’s may also develop aneurysms. In patients with abdominal aortic aneurysms the extracellular matrix becomes disrupted with a change in the balance of collagen and elastic fibres.
Rupture of AAA
20% rupture anteriorly into the peritoneal cavity with very poor prognosis
80% rupture posteriorly into the retroperitoneal space
Risk of AAA rupture
The risk of rupture is related to aneurysm size, only 2% of aneurysms measuring less than 4cm in diameter will rupture over a 5 year period. This contrasts with 75% of aneurysms measuring over 7cm in diameter.
Imaging in AAA
most vascular surgeons will subject patients with an aneurysm size of 5cm or greater to CT scanning of the chest, abdomen and pelvis with the aim of delineating anatomy and planning treatment. Depending upon co-morbidities, surgery is generally offered once the aneurysm is between 5.5cm and 6cm.
Indications for surgery in AAA
Symptomatic aneurysms (80% annual mortality if untreated)
Increasing size above 5.5cm if asymptomatic
Rupture (100% mortality without surgery)
Procedure in AAA repair
GA
Invasive monitoring (A-line, CVP, catheter)
Incision: Midline or transverse
Bowel and distal duodenum mobilised to access aorta.
Aneurysm neck and base dissected out and prepared for cross clamp
Systemic heparinisation
Cross clamp (proximal first)
Longitudinal aortotomy
Atherectomy
Deal with back bleeding from lumbar vessels and inferior mesenteric artery
Insert graft either tube or bifurcated depending upon anatomy
Suture using Prolene (3/0 for proximal , distal anastomosis suture varies according to site)
Clamps off: End tidal CO2 will rise owing to effects of reperfusion, at this point major risk of myocardial events.
Haemostasis
Closure of aneurysm sac to minimise risk of aorto-enteric fistula
Closure: Loop 1 PDS or Prolene to abdominal wall
Skin- surgeons preference
ITU
Complications of AAA repair
Greatest risk of complications following emergency repair
Complications: Embolic- gut and foot infarcts
Cardiac - owing to premorbid states, re-perfusion injury and effects of cross clamp
Wound problems
Later risks related to graft- infection and aorto-enteric fistula
Management of suprarenal AAA
These patients will require a supra renal clamp and this carries a far higher risk of complications and risk of renal failure.
Management of ruptured AAA
Stratified based on haemodynamic status
Compromise- laparotomy
Stable- CT ?rupture.
Operative details are similar to elective repair although surgery should be swift, blind rushing often makes the situation worse. Plunging vascular clamps blindly into a pool of blood at the aneurysm neck carries the risk of injury the vena cava that these patients do not withstand. Occasionally a supracoeliac clamp is needed to effect temporary control, although leaving this applied for more than 20 minutes tends to carry a dismal outcome.
Outcome of retroperitoneal AAA rupture
These patients will tend to develop retroperitoneal haematoma. This can be disrupted if BP is allowed to rise too high so aim for BP 100mmHg.
AAA features suitable for EVAR
Long neck
Straight iliac vessels
Healthy groin vessels
(fenestrated grafts can allow suprarenal AAA to be treated)
Procedure in EVAR AAA
GA
Radiology or theatre
Bilateral groin incisions
Common femoral artery dissected out
Heparinisation
Arteriotomy and insertion of guide wire
Dilation of arteriotomy
Insertion of EVAR Device
Once in satisfactory position it is released
Arteriotomy closed once check angiogram shows good position and no endoleak
Complications of EVAR AAA
Endoleaks depending upon site are either Type I or 2. These may necessitate re-intervention and all EVAR patients require follow up . Details are not needed for MRCS.
A 50 year old lady presents with pain in her proximal femur. Imaging demonstrates a bone metastasis from an unknown primary site. CT scanning with arterial phase contrast shows that the lesion is hypervascular. From which of the following primary sites is the lesion most likely to have originated?
Breast
Renal
Bronchus
Thyroid
Colon
Renal metastases have a tendency to be hypervascular. This is of considerable importance if surgical fixation is planned.
The typical tumours that spread to bone include:
Breast
Bronchus
Renal
Thyroid
Prostate
Commonest bony met sites
Vertebrae (usually thoracic)
Proximal femur
Ribs
Sternum
Pelvis
Skull
Which of the following is true regarding the Salmonella species?
Rose spots appear in all patients with typhoid
They are normally present in the gut as commensals
Subsequent chronic biliary infection occurs in 75% of cases
A relative bradycardia is often seen in typhoid fever
Salmonella typhi can be categorised into type A, B and C
A relative bradycardia is often seen in typhoid fever
initially systemic upset as above
relative bradycardia
abdominal pain, distension
constipation: although Salmonella is a recognised cause of diarrhoea, constipation is more common in typhoid
rose spots: present on the trunk in 40% of patients, and are more common in paratyphoid
Salmonella
Possible Cx of salmonella infection
osteomyelitis (especially in sickle cell disease where Salmonella is one of the most common pathogens)
GI bleed/perforation
meningitis
cholecystitis
chronic carriage (1%, more likely if adult females)
A 43 year old lady undergoes a day case laparoscopic cholecystectomy. The operation is more difficult than anticipated and a drain is placed to the operative site. Whilst in recovery, the patient loses 1800ml of frank blood into the drain. Which of the following will not occur?
Release of aldosterone via the Bainbridge reflex
Reduced urinary sodium excretion
Increase in sympathetic discharge to ventricular muscle
Fall in parasympathetic discharge to the sino atrial node
Decreased stimulation from atrial pressure receptors
The Bainbridge reflex is the increase in heart rate mediated via atrial stretch receptors that occurs following a rapid infusion of blood.
A 48 year old lady has a metallic heart valve and requires a paraumbilical hernia repair. Perioperatively she is receiving intra venous unfractionated heparin. To perform the surgery safely a normal coagulation state is required. Which of the following strategies is routine standard practice?
Administration of 10 mg of vitamin K the night prior to surgery and stopping the heparin infusion 6 hours pre operatively
Stopping the heparin infusion 6 hours pre operatively
Stop the heparin infusion on induction of anaesthesia
Stopping the heparin infusion 6 hours pre operatively and administration of intravenous protamine sulphate on commencing the operation
None of the above
Patients with metallic heart valves will generally stop unfractionated heparin 6 hours pre operatively. Unfractionated heparin is generally cleared from the circulation within 2 hours so this will allow plenty of time and is the method of choice in the elective setting. Protamine sulphate will reverse heparin but is associated with risks of anaphylaxis and is thus not generally used unless immediate reversal of anticoagulation is needed, e.g. coming off bypass.
MOA heparin
Causes the formation of complexes between antithrombin and activated thrombin/factors 7,9,10,11 & 12
Which of the following statements relating to biliary atresia is untrue?
It most commonly presents as prolonged conjugated jaundice in the neonatal period.
Evidence of portal hypertension at diagnosis is seldom present in the UK.
It may be confused with Alagille syndrome.
The Kasai procedure is best performed in the first 8 weeks of life.
Survival following a successful Kasai procedure is approximately 45% at 5 years.
Biliary atresia usually presents with obstructed jaundice. A Kasai procedure is best performed in the first 8 weeks of life. If a Kasai procedure is successful most patients will not require liver transplantation. 45% of patients post Kasai procedure will require transplantation. However, overall survival following a successful Kasai procedure is 80%.
Alagille syndrome
Alagille syndrome autosomal dominant disorder characterised by presence of paucity of bile ducts and cardiac defects. Only the embryonic form of biliary atresia is associated with cardiac and other embryological defects.

Biliary atresia
Biliary tree lumen is obliterated by an inflammatory cholangiopathy causing progressive liver damage
Infant well in 1st few weeks of life
No family history of liver disease
Jaundice in infants > 14 days in term infants (>21 days in pre term infants)
Pale stool, yellow urine (colourless in babies)
Associated with cardiac malformations, polysplenia, situs inversus
Biliary atresia
Ix in biliary atresia
Conjugated bilirubin (prolonged physiological jaundice or breast milk jaundice will cause a rise in unconjugated bilirubin, whereas those with obstructive liver disease will have a rise in conjugated bilirubin)
Ultrasound of the liver (excludes extrahepatic causes, in biliary atresia infant may have tiny or invisible gallbladder)
Hepato-iminodiacetic acid radionuclide scan (good uptake but no excretion usually seen)
Mx of biliary atresia
Early recognition is important to prevent liver transplantation.
Nutritional support.
Roux-en-Y portojejunostomy (Kasai procedure).
If Kasai procedure fails or late recognition, a liver transplant becomes the only option.
A 23 year old man is stabbed in the chest approximately 10cm below the right nipple. In the emergency department a abdominal ultrasound scan shows a large amount of intraperitoneal blood. Which of the following statements relating to the likely site of injury is untrue?
Part of its posterior surface is devoid of peritoneum.
The quadrate lobe is contained within the functional right lobe.
Its nerve supply is from the coeliac plexus.
The hepatic flexure of the colon lies posterio-inferiorly.
The right kidney is closely related posteriorly.
The right lobe of the liver is the most likely site of injury. Therefore the answer is B as the quadrate lobe is functionally part of the left lobe of the liver. The liver is largely covered in peritoneum. Posteriorly there is an area devoid of peritoneum (the bare area of the liver). The right lobe of the liver has the largest bare area (and is larger than the left lobe).
A 22 year old man is involved in a fight and sustains a skull fracture with an injury to the middle meningeal artery. A craniotomy is performed, and with considerable difficulty the haemorrhage from the middle meningeal artery is controlled by ligating it close to its origin. What is the most likely sensory impairment that the patient may notice post operatively?
Parasthesia of the ipsilateral external ear
Loss of taste sensation from the anterior two thirds of the tongue
Parasthesia overlying the angle of the jaw
Loss of sensation from the ipsilateral side of the tongue
Loss of taste from the posterior two thirds of the tongue
The auriculotemporal nerve is closely related to the middle meningeal artery and may be damaged in this scenario. The nerve supplied sensation to the external ear and outermost part of the tympanic membrane. The angle of the jaw is innervated by C2,3 roots and would not be affected. The tongue is supplied by the glossopharyngeal nerve.

Course of the middle meningeal artery?
Middle meningeal artery is typically the third branch of the first part of the maxillary artery, one of the two terminal branches of the external carotid artery. After branching off the maxillary artery in the infratemporal fossa, it runs through the foramen spinosum to supply the dura mater (the outermost meninges) .
What are the other arteries supplying the meninges?
Anterior and posterior meningeal arteries
Where is the MMA vulnerable to injury?
Where it runs beneath the pterion
What nerve is closely associated to the MMA?
The middle meningeal artery is intimately associated with the auriculotemporal nerve which wraps around the artery making the two easily identifiable in the dissection of human cadavers and also easily damaged in surgery.

A 72 year old man presents with haemoptysis and undergoes a bronchoscopy. The carina is noted to be widened. At which level does the trachea bifurcate?
T3
T5
T7
T2
T8
The trachea bifurcates at the level of the fifth thoracic vertebra. Or the sixth in tall subjects.
Arterial and venous supply of the trachea?
Inferior thyroid arteries and the thyroid venous plexus.
Theme: Hernias
A.Umbilical hernia
B.Para umbilical hernia
C.Morgagni hernia
D.Littres hernia
E.Bochdalek hernia
F.Richters hernia
G.Obturator hernia
Please select the hernia that most closely matches the description given. Each option may be used once, more than once or not at all.
27.A 1 day old infant is born with severe respiratory compromise. On examination he has a scaphoid abdomen and an absent apex beat.
A 2 month old infant is troubled by recurrent colicky abdominal pain and intermittent intestinal obstruction. On imaging the transverse colon is herniated into the thoracic cavity, through a mid line defect.
A 78 year old lady is admitted with small bowel obstruction, on examination she has a distended abdomen and the leg is held semi flexed. She has some groin pain radiating to the ipsilateral knee.
Bochdalek hernia
The large hernia may displace the heart although true dextrocardia is not present. The associated pulmonary hypoplasia will compromise lung development.
Morgagni hernia
Morgagni hernia may contain the transverse colon. Unless there is substantial herniation, pulmonary hypoplasia is uncommon. As a result, major respiratory compromise is often absent.
Obturator hernia
The groin swelling in obturator hernia is subtle and hard to elicit clinically. There may be pain in the region of sensory distribution of the obturator nerve. The defect is usually repaired from within the abdomen.
Interparietal hernia occurring at the level of the arcuate line
Rare
May lie beneath internal oblique muscle. Usually between internal and external oblique
Equal sex distribution
Position is lateral to rectus abdominis
Both open and laparoscopic repair are possible, the former in cases of strangulation
Spigelian hernia
Boundaries of the lumbar traingle?
Crest of ilium (inferiorly) External oblique (laterally) Latissimus dorsi (medially)
Treatment of lumbar hernia
- Direct anatomical repair with or without mesh re-enforcement is the procedure of choice
Herniation through the obturator canal
Commoner in females
Usually lies behind pectineus muscle
Elective diagnosis is unusual most will present acutely with obstruction
When presenting acutely most cases with require laparotomy or laparoscopy (and small bowel resection if indicated)
Obturator hernia
Condition in which part of the wall of the small bowel (usually the anti mesenteric border) is strangulated within a hernia (of any type)
They do not present with typical features of intestinal obstruction as lumenal patency is preserved
Where vomiting is prominent it usually occurs as a result of paralytic ileus from peritonitis (as these hernias may perforate)
Richters hernia
Occur through sites of surgical access into the abdominal cavity
Most common following surgical wound infection
To minimise following midline laparotomy Jenkins Rule should be followed and this necessitates a suture length 4x length of incision with bites taken at 1cm intervals, 1 cm from the wound edge
Repair may be performed either at open surgery or laparoscopically and a wide variety of techniques are described
Incisional hernia
Typically congenital diaphragmatic hernia
85% cases are located in the left hemi diaphragm
Associated with lung hypoplasia on the affected side
More common in males
Associated with other birth defects
May contain stomach
May be treated by direct anatomical apposition or placement of mesh. In infants that have severe respiratory compromise mechanical ventilation may be needed and mortality rate is high
Bochdalek hernia
Rare type of diaphragmatic hernia (approx 2% cases)
Herniation through foramen of Morgagni
Usually located on the right and tend to be less symptomatic
More advanced cases may contain transverse colon
As defects are small pulmonary hypoplasia is less common
Direct anatomical repair is performed
Morgagni Hernia
Hernia through weak umbilicus
Usually presents in childhood
Often symptomatic
Equal sex incidence
95% will resolve by the age of 2 years
Surgery performed after the third birthday
Umbilical hernia
Usually a condition of adulthood
Defect is in the linea alba
More common in females
Multiparity and obesity are risk factors
Traditionally repaired using Mayos technique - overlapping repair, mesh may be used though not if small bowel resection is required owing to acute strangulation
Paraumbilical hernia
Hernia containing Meckels diverticulum
Resection of the diverticulum is usually required and this will preclude a mesh repair
Littres hernia
A 23 year old man is injured during a game of rugby. He suffers a fracture of the distal third of his clavicle, it is a compound fracture and there is evidence of arterial haemorrhage. Which of the following vessels is most likely to be encountered first during subsequent surgical exploration?
Posterior circumflex humeral artery
Axillary artery
Thoracoacromial artery
Sub scapular artery
Lateral thoracic artery
The thoracoacromial artery arises from the second part of the axillary artery. It is a short, wide trunk, which pierces the clavipectoral fascia, and ends, deep to pectoralis major by dividing into four branches.
Passage of the thoraco-acromial artery
The thoracoacromial artery (acromiothoracic artery; thoracic axis) is a short trunk, which arises from the forepart of the axillary artery, its origin being generally overlapped by the upper edge of the Pectoralis minor.
Projecting forward to the upper border of the Pectoralis minor, it pierces the coracoclavicular fascia and divides into four branches: pectoral, acromial, clavicular, and deltoid.
Branches of the thoraco-acromial artery?
CAPD
Pectoral
Acromial
Clavicular
Deltoid

Descends between the two Pectoral muscles, and is distributed to them and to the breast, anastomosing with the intercostal branches of the internal thoracic artery and with the lateral thoracic.
Pectoral branch of the thoracoacromial artery

Runs laterally over the coracoid process and under the Deltoid, to which it gives branches; it then pierces that muscle and ends on the acromion in an arterial network formed by branches from the suprascapular, thoracoacromial, and posterior humeral circumflex arteries.
Acromial branch

Runs upwards and medially to the sternoclavicular joint, supplying this articulation, and the Subclavius.
Clavicular branch of the thoracoacromial

Arising with the acromial, it crosses over the Pectoralis minor and passes in the same groove as the cephalic vein, between the Pectoralis major and Deltoid, and gives branches to both muscles.
Deltoid branch of the thoracoacromial artery

The following are true of the femoral nerve, except:
It is derived from L2, L3 and L4 nerve roots
It supplies sartorius
It supplies quadriceps femoris
It gives cutaneous innervations via the saphenous nerve
It supplies adductor longus
Adductor longus is supplied by the obturator nerve.
Femoral nerve roots
L2, 3, 4
Innervated by femoral nerve?
Pectineus
Sartorius
Quadriceps femoris
Vastus lateralis/medialis/intermedius
Branches of the femoral nerve
Medial cutaneous nerve of thigh
Saphenous nerve
Intermediate cutaneous nerve of thigh
Femoral nerve supply
MISVQ Scan for PE
M edial cutaneous nerve of the thigh
I ntermediate cutaneous nerve of the thigh
S aphenous nerve
V astus
Q uadriceps femoris
S artorius
PE ectineus
ABC’s of Non- GI causes of vomiting
Acute renal failure
Brain (Increased ICP)
Cardiac (Inferior MI)
DKA
Ears (labyrinthitis)
Foreign substances (Tylenol, theo, etc)
Glaucoma
Hyperemesis Gravidarum
Infections (pyelonephritis, meningitis)
Approximately what proportion of salivary secretions is provided by the submandibular glands?
10%
70%
40%
90%
20%
Although they are small, the submandibular glands provide the bulk of salivary secretions and contribute 70%, the sublingual glands provide 5% and the remainder from the parotid.
Which of the following statements relating to gastric cancer is untrue?
It is associated with chronic helicobacter pylori infection
5% of gastric malignancies are due to lymphoma
In the Lauren classification the diffuse type of adenocarcinoma typically presents as a large exophytic growth in the antrum
Smoking is a risk factor
It is associated with acanthosis nigricans
The Lauren classification describes a diffuse type of adenocarcinoma (Linitis plastica type lesion) and an intestinal type. The diffuse type is often deeply infiltrative and may be difficult to detect on endoscopy. Barium meal appearances can be characteristic
Barium meal appearances of linitis plastica:
Due to the increased rigidity of the wall, the stomach cannot be adequately distended, with only a narrow lumen identified. The normal mucosal fold pattern is absent, either distorted, thickened or nodular.

Treatment of gastric cancer >5-10cm from the GOJ
Sub total gastrectomy
Treatment of gastric cancer if tumour <5cm from GOJ
Total gastrectomy
Prognosis in RO resection of gastric cancer
54%
5ys in early gastric cancer
91%
5ys in Stage 3 gastric cancer
18%
Procedure in Total gastrectomy, lymphadenectomy and Roux en Y anastomosis
General anaesthesia
Prophylactic intravenous antibiotics
Incision: Rooftop.
Perform a thorough laparotomy to identify any occult disease.
Mobilise the left lobe of the liver off the diaphragm and place a large pack over it. Insert a large self retaining retractor e.g. omnitract or Balfour (take time with this, the set up should be perfect). Pack the small bowel away.
Begin by mobilising the omentum off the transverse colon.
Proceed to detach the short gastric vessels.
Mobilise the pylorus and divide it at least 2cm distally using a linear cutter stapling device.
Continue the dissection into the lesser sac taking the lesser omentum and left gastric artery flush at its origin.
The lymph nodes should be removed en bloc with the specimen where possible.
Place 2 stay sutures either side of the distal oesophagus. Ask the anaesthetist to pull back on the nasogastric tube. Divide the distal oesophagus and remove the stomach.
The oesphago jejunal anastomosis should be constructed. Identify the DJ flexure and bring a loop of jejunum up to the oesophagus (to check it will reach). Divide the jejunum at this point. Bring the divided jejunum either retrocolic or antecolic to the oesophagus. Anastamose the oesophagus to the jejunum, using either interrupted 3/0 vicryl or a stapling device. Then create the remainder of the Roux en Y reconstruction distally.
Place a jejunostomy feeding tube.
Wash out the abdomen and insert drains (usually the anastomosis and duodenal stump). Help the anaesthetist insert the nasogastric tube (carefully!)
Close the abdomen and skin.
Enteral feeding may commence on the first post-operative day. However, most surgeons will leave patients on free NG drainage for several days and keep them nil by mouth.
Which is the least likely to cause hyperuricaemia?
Severe psoriasis
Lesch-Nyhan syndrome
Amiodarone
Diabetic ketoacidosis
Alcohol
Amiodarone
Decreased tubular secretion of urate occurs in patients with acidosis (eg, diabetic ketoacidosis, ethanol or salicylate intoxication, starvation ketosis). The organic acids that accumulate in these conditions compete with urate for tubular secretion.
Mnemonic of the drugs causing hyperuricaemia as a result of reduced excretion of urate
Can’t leap
C iclosporin
A lcohol
N icotinic acid
T hiazides
L oop diuretics
E thambutol
A spirin
P yrazinamide
Causes of increased uric acid synthesis
Lesch-Nyhan disease
Myeloproliferative disorders
Diet rich in purines
Exercise
Psoriasis
Cytotoxics
Causes of decreased uric acid excretion
Drugs: low-dose aspirin, diuretics, pyrazinamide
Pre-eclampsia
Alcohol
Renal failure
Lead
Theme: Right iliac fossa pain
A.Open Appendicectomy
B.Laparoscopic appendicectomy
C.Laparotomy
D.CT Scan
E.Colonoscopy
F.Ultrasound scan abdomen/pelvis
G.Active observation
For each scenario please select the most appropriate management option from the list. Each option may be used once, more than once or not at all.
37.A 21 year old women is admitted with a 48 hour history of worsening right iliac fossa pain. She has been nauseated and vomited twice. On examination, she is markedly tender in the right iliac fossa with localised guarding. Vaginal examination is unremarkable. Urine dipstick (including beta HCG) is negative. Blood tests show a WCC of 13.5 and CRP 70.
An 8 year old boy presents with a 4 hour history of right iliac fossa pain with nausea and vomiting. He has been back at school for two days after being kept home with a flu like illness. On examination he is tender in the right iliac fossa, although his abdomen is soft. Temperature is 38.3oc. Blood tests show a CRP of 40 and a WCC of 8.1.
A 21 year old women presents with right iliac fossa pain. She reports some bloodstained vaginal discharge. She has a HR of 65 bpm.
Laparoscopic appendicectomy
She is likely to have appendicitis. In women of this age there is always diagnostic uncertainty. With a normal vaginal exam laparoscopy would be preferred over USS
Active observation
This is mesenteric adenitis. Note history of flu like illness and temp > 38o c.
The decision as to how to manage this situation is based on the abdominal findings. Patients with localising signs such as guarding or peritonism should undergo surgery.
Ultrasound scan abdomen/pelvis
This patient is suspected of having an ectopic pregnancy. She needs an urgent β HCG and USS of the pelvis. If she were haemodynamically unstable then laparotomy would be indicated.
Which of the following nerves conveys sensory information from the laryngeal mucosa?
Glossopharyngeal
Laryngeal branches of the vagus
Ansa cervicalis
Laryngeal branches of the trigeminal
None of the above
The laryngeal branches of the vagus supply sensory information from the larynx.
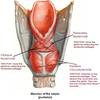
Location of the larynx?
C3-C6
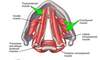
What are the paired cartilaginous segments of the larynx?
arytenoid, corniculate and cuneiform.

What are the single cartilaginous segments of the larynx?
single; thyroid, cricoid and epiglottic (cricoid forms a complete ring)

Extent of the laryngeal cavity?
From the laryngeal inlet to the inferior border of the cricoid cartilage
What are the divisions of the laryngeal cavity?
Laryngeal vestibule
Laryngeal ventricle
Infraglottic cavity

Laryngeal vestibule
Superior to the vestibular folds
Laryngeal ventricle
Lies between vestibular folds and superior to the vocal cords

Infraglottic cavity
From the vocal cords to the inferior border of the cricoid cartilage
Components of the vocal cord?
Vocal ligament
Vocalis muscle (most medial part of thyroarytenoid muscle)
Components of the glottis
The glottis is composed of the vocal folds, processes and rima glottidis. The rima glottidis is the narrowest potential site within the larynx, as the vocal cords may be completely opposed, forming a complete barrier.
What is the only muscle of the larynx not innervated by the recurrent laryngeal nerve?
Circothyroid
Muscles of the larynx
Posterior cricoarytenoid
Lateral cricoarytenoid
Thyroarytenoid
Transverse and oblique arytenoids
Vocalis
Cricothyroid
Action of the posterior cricoarytenoid
Abducts the vocal fold
Action of the lateral cricoarytenoid
Adducts vocal fold
Action of thyroarytenoid
Relaxes vocal fold
Action of transverse and oblique arytenoids
Closure of intercartilaginous part of the rima glottidis
Action of vocalis
Relaxes posterior vocal ligament, tenses anterior part
Action of cricothyroid
Tenses vocal fold
Origin and insertion of Posterior cricoarytenoid
Posterior aspect of lamina of cricoid
Muscular process of arytenoid
Origin and insertion of Lateral cricoarytenoid
Arch of cricoid
Muscular process of arytenoid

Origin and insertion of thyroarytenoid
Posterior aspect of thyroid cartilage
Muscular process of arytenoid
Origin and insertion of transverse and oblique arytenoids
Arytenoid cartilage
Contralateral arytenoid

Origin and insertion of vocalis
Depression between lamina of thyroid cartilage
Vocal ligament and vocal process of arytenoid cartilage

Origin and insertion of cricothyroid
Anterolateral part of cricoid
Inferior margin and horn of thyroid cartilage

Arterial supply of the larynx
Arterial supply is via the laryngeal arteries, branches of the superior and inferior thyroid arteries
To which nerve is the superior laryngeal artery closely related?
Internal laryngeal nerve
To which nerve is the inferior laryngeal artery related?
Inferior laryngeal nerve
Venous drainage of the larynx
Superior laryngeal vein-> superior thyroid vein
Inferior laryngeal vein-> middle or thyroid venous plexus
Lymphatic drainage of the vocal cords
No lymphatic drainage and act as a lymphatic watershed
Lymphatic drainage of the supraglottic part of the larynx
Upper deep cervical nodes
Lymphatic drainage of the subglottic part
Prelaryngeal and pretracheal nodes and inferior deep cervical nodes
Which of the following nerves passes through the greater sciatic foramen and innervates the perineum?
Pudendal
Sciatic
Superior gluteal
Inferior gluteal
Posterior cutaneous nerve of the thigh
The pudendal nerve innervates the perineum. It passes between piriformis and coccygeus medial to the sciatic nerve.
What are the three divisions of the pudendal nerve?
3 divisions of the pudendal nerve:
Rectal nerve
Perineal nerve
Dorsal nerve of penis/ clitoris
All these pass through the greater sciatic foramen.

What are the gluteal muscles and their action?
Gluteus maximus, medius, minimus.
All extend and abduct the hip
Insertion of gluteus maximus
Inserts into gluteal tuberosity of the femur and iliotibial tract

Attachment of gluteus medius
Attach to lateral greater trochanter

Attachment of gluteus minimis
Attach to anterior greater trochanter

What are the deep lateral hip rotators?
Piriformis
Gemeilli
Obturator internus
Quadratus femoris
What are the nerve roots of the superior gluteal nerve?
L5 S1
What muscles are innervated by the superior gluteal nerve?
Gluteus medius
Gluteus minimis
Tensor fascia lata
What innervates gluteus maximus?
Inferior gluteal nerve
Damage to which nerve causes a Trendelenberg gait?
Damage to the superior gluteal nerve will result in the patient developing a Trendelenberg gait. Affected patients are unable to abduct the thigh at the hip joint. During the stance phase, the weakened abductor muscles allow the pelvis to tilt down on the opposite side. To compensate, the trunk lurches to the weakened side to attempt to maintain a level pelvis throughout the gait cycle. The pelvis sags on the opposite side of the lesioned superior gluteal nerve.
A 60-year-old man presents with lower urinary tract symptoms and is offered a PSA test. Which one of the following could interfere with the PSA level?
Vigorous exercise in the past 48 hours
Poorly controlled diabetes mellitus
Drinking more than 4 units of alcohol in the past 48 hours
Smoking
Recent cholecystectomy
Vigorous exercise in the past 48 hours
What is prostate specific antigen?
Serine protease enzyme produced by normal and malignant prostate epithelial cells
What are the age-adjusted upper limits for PSA?
50-59- 3
60-69- 4
>70- 5
aide memoire for upper PSA limit: (age - 20) / 10
Other causes of raised PSA
benign prostatic hyperplasia (BPH)
prostatitis and urinary tract infection (NICE recommend to postpone the PSA test for at least 1 month after treatment)
ejaculation (ideally not in the previous 48 hours)
vigorous exercise (ideally not in the previous 48 hours)
urinary retention
instrumentation of the urinary tract
Specificity and sensitivity of PSA
around 33% of men with a PSA of 4-10 ng/ml will be found to have prostate cancer. With a PSA of 10-20 ng/ml this rises to 60% of men
around 20% with prostate cancer have a normal PSA
various methods are used to try and add greater meaning to a PSA level including age-adjusted upper limits and monitoring change in PSA level with time (PSA velocity or PSA doubling time)
Which of the following is true in relation to the sartorius muscle?
Innervated by the deep branch of the femoral nerve
Inserts at the fibula
It is the shortest muscle in the body
Forms the Pes anserinus with Gracilis and semitendinous muscle
Causes extension of the knee
Forms the Pes anserinus with Gracilis and semitendinous muscle
It is innervated by the superficial branch

Origin and insertion of sartorius
Anterior superior iliac spine
Medial surface of the of the body of the tibia (upper part). It inserts anterior to gracilis and semitendinosus
Innervation of sartorius
Superficial branch of femoral nerve
Action of sartorius
Flexor of the hip and knee, slight abducts the thigh and rotates it laterally
It assists with medial rotation of the tibia on the femur. For example it would play a pivotal role in placing the right heel onto the left knee ( and vice versa)
Important relations of sartorius
The middle third of this muscle, and its strong underlying fascia forms the roof of the adductor canal , in which lie the femoral vessels, the saphenous nerve and the nerve to vastus medialis.
Which of the following is a permanent suture material best suited for interrupted mattress dermal closure?
2/0 Polydiaxone
3/0 Polydiaxone
4/0 Polyglycolic acid
1/0 Dexon
3/0 Polypropylene
Of the sutures listed only prolene is a permanent suture material. It is a good agent for skin closure as it does not incite an inflammatory response and thus provides good cosmesis.
Features of suture size
The higher the index number the smaller the suture i.e. : 6/0 prolene is finer than 1/0 prolene.
Finer sutures have less tensile strength. For example 6/0 prolene would not be a suture suitable for abdominal mass closure but would be ideal for small calibre distal arterial anastomoses.
Theme: Nerve lesions
A.Sciatic nerve
B.Peroneal nerve
C.Tibial Nerve
D.Obturator nerve
E.Ilioinguinal nerve
F.Femoral nerve
G.None of the above
Please select the most likely nerve injury for the scenario given. Each option may be used once, more than once or not at all
9.A 56 year old man undergoes a low anterior resection with legs in the Lloyd-Davies position. Post operatively he complains of foot drop.
A 23 year old man complains of severe groin pain several weeks after a difficult inguinal hernia repair.
A 72 year old man develops a foot drop after a revision total hip replacement.
Peroneal nerve
Positioning legs in Lloyd- Davies stirrups can carry the risk of peroneal nerve neuropraxia if not done carefully.
Ilioinguinal nerve
The ilioinguinal nerve may have been entrapped in the mesh causing a neuroma.
Sciatic nerve
This may be done by a number of approaches, in this scenario a posterior approach is the most likely culprit.
Muscles in the anterior compartment of the leg
Tibialis anterior
EDL
Peroneus tertius
EHL

Innervation of the anterior compartment tof the lower limb?
Deep peroneal nerve
Muscles in the peroneal compartment of the lower limb
Peroneus longus
Peroneus brevis
Innervation of the peroneal compartment of the lower leg
Superficial peroneal nerve
Muscles in the superficial posterior compartment of the lower limb
Gastrocnemius
Plantaris (10%)
Soleus
Innervation of the superficial posterior compartment of the lower limb
Tibial nerve
Muscles in the deep posterior compartment of the lower limb
FDL
FHL
Tibialis posterior
Innervation of the deep posterior compartment of the lower limb
Tibial
Tibialis anterior
Dorsiflexes ankle joint, inverts foot
Extensor digitorum longus
Extends lateral four toes, dorsiflexes ankle joint
Peroneus tertius
Dorsiflexes ankle, everts foot
Extensor hallucis longus
Dorsiflexes ankle joint, extends big toe
Peroneus longus
Everts foot, assists in plantar flexion
Peroneus brevis
Plantar flexes the ankle joint
Gastrocnemius
Plantar flexes the foot, may also flex the knee
Soleus
Plantar flexor