Biology New Information Flashcards
Where is blood pumped into in the heart?
aorta, which branches into a series of arteries
What do the arterie the branch into?
arterioles and then into microscopic capilaries
What is exchanged across the capillary walls?
gases, nutrients and cellular waste products occurs via diffusion
How is blood brought back to the heart?
The capillaries then converge into venules and eventually into veins, which carry deoxygenated blood back toward the heart
Explain the heart sides (right and left)
Right side = deoxygenated blood into pulmonary circulation (toward the lungs)
Left side = oxygenated blood into systematic circulation (throughout the body)
What are the two upper chamber and two lower chambers of the heart called
Upper chambers = atria (thin walled)
lower chambers = ventricles (muscular)
The left ventricle is more muscular than the right because it is responsible for generating the forse that propels the systemic circulation and because it pumps agains the higher resistance

In patients with increased systemic resistance (artaries clogged), what happens to the heart?
the left ventricle can become hypertrophied (enlarged) which over time can lead to congestive heart failure and other cardiovascular diseases

Explain the process of blood flow through the heart
- Blood returning from the body first flows through the right atrium, then through the tricuspid valve into the right ventricle
- finally through the pulmonary semilunar valve into the pulmonary arteries to continue to the lungs
- Blood returning from the lungs flows through the pulmonary veins into the left atrium
- then through the mitral valve into the left ventricle
- Finally through the aortic semilunar valve into the systemic circulation

What are the valves in the heart, location and purpose?
-
Atrioventricular valves, located between the atria and ventricles on both sides of the heart, prevent backflow of blood into the atria
-
right side = tricuspid valve
- because it has three cusps
-
left side = mitral valve
- becaue it has two cusps
-
right side = tricuspid valve
-
Semilunar valves
- have three cusps
- located between the left ventricle and aorta and between right ventricle and pulmonary artery
What is the “lub-dub” sound from?
made by the successive closing of the atrioventricular and semilunar valves
What is the heart’s pumping cycle described as?
- two alternating phases: = heatbeat
- Systole
- Period during which the ventricles contract, forcing blood out of the heart into the pulmonary and systemic circulation
- Blood vessel contraction pressure
- Diastole
- period of cardiac muscle relaxation during which the blood drains into all four chambers
- pressure during cardiac relaxation
- Systole
- Together they make blood pressure measurement
How is cardiac output defined by?
The total volume of blood the left ventricle pumps out per minute
Cardiac output = heart rate (number of beats per minute) x stroke volume (volume of blood pumped out of the left ventricle per contraction
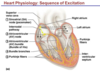
Explain how the heart rate is controlled by the body
- Cardiac muscle contracts rhythmically without stimulation from the nervous system, producing impulses that spread through its internal conduction system
- Ordinary cardiac contraction originates in, and is regulated by the sinoatrial (SA) node (the pacemaker) a small mass of specialized tissue located in the walls of the right atrium
- SA note spreads impulses through both atria, contracting simultaneously
- Impulses arrive at the atrioventricular (AV) node, which slowly conducts impulses to the rest of the heart, allowing enough time for atrial contraction and for the ventricles to fill with blood
- The impulses is then carried by the bundles of His (AV bundles), which branches into the right and left bundle branches
- Then through the Purkinje Fibers in the walls of both the ventricles, stimulating a strong contraction to rest of body
What innervates the heart
- The autonomic nervous system modifies the rate of the heart contraction
- The parasympathetic nervous system innervates the heart via the vagus nerves and causes a decrease in heart rate
- The sympathetic nervous system innervates the heart via the cervical and upper thoracic ganglia and causes an increase in heart rate
- Adrenal medulla exerts hormonal control via epinephrine (adrenaline) secretion, increasing heart rate
Name and describe the three types of blood vessels
-
Arteries = thick walled, muscular, elastic vessels that transport oxygenated blood from heart,
- except for the pulmonary arteries which transport deoxygenated blood
-
Veins = relatively thin walled, inelastic vessels that conduct deoxygenated blood to heart
- except for the pulmonary vein which transports oxygenated blood
- Most have valves, especially in legs, that prevent backflow
-
Capillaries = smallest diameter, red blood cells must often travel through them single file
- Location of where nutrients readily diffuse
Explain the lymph vessels
- secondary circulatory system distinct from the cardiovascular circulation
- vessels transport excess interstitial fluid, called lymph, to the cardiovascular system, thereby keeping fluid levels in the body consistant
- Smallest lymphatic vessels (lacteals) collect fats, in the form of chylomicrons, from the villi in the small intestine and deliver them into the bloodstream, bypassing the liver
- Lymph nodes are swellings along lymph vessels containing phagocytic cells (lymphocytes) that filter the lymph, removing and destroyign foreign particles and pathogens)
Explain the makeup of blood
- Contains four to six liters of blood
-
55% = liquid component
-
plasma
- aqueous mixture of nutrients, salts, repiratory gases, wastes, hormones, and blood proteins (eg. immunoglobulins, albumin, and fibronogen)
-
plasma
-
45% = cellular component
- erythrocytes, leukocytes and platelets
Explain Leukocytes
- Leukocytes = white blood cells (or WBCs)
- larger than erythrocytes and serves protective function
Explain Platelets
- Platelets
- cell fragments that lack nuclei and are involved in clot formation
- Many drugs inhibit platelet formation or adhesion to decrease clot development
- cell fragments that lack nuclei and are involved in clot formation
What are erythrocytes
-
Erythrocytes
- Red blood cells (RBC’s)
- oxygen-carrying components of blood
- contain ~250 million molecules of hemoglobin, each of which can bind up to four molecules of oxygen
- When hemoglobin binds to oxygen = oxyhemoglobin
- Primary form of oxygen transport in body
- Have distinct disk like shape that give them increased surface area for gas exchange and greater flexibility for movement
- Erythrocytes are formed from stem cells in the bone marrow; stimulated by erythropoietin, a hormone make in the kidnesy
What does it mean when you find immature erythrocytes circulating in the bloodstream?
- that is, before they have lost their organelles from the bone marrow -
- Can be an indicator of a number of disease states, such as hemolytic anemia, which is caused by a rapid destruction of red blood cells due to an infection or disorder
Explain ABO Blood types
-
Erythrocytes have characteristic cell-surface proteins (antigens)
-
Antigens = macromolecules that are foreign to the host organism and triggers an immune response
- two major antigens = ABO group and the Rh Factor
-
Antigens = macromolecules that are foreign to the host organism and triggers an immune response
- See attached for table with which Blood type has which antigen and antibody
- It is extremely important durign blood transfusions that donor and recipient blood types be appropriately matched

What is the universal recipient of blood?
Type AB
has neither anti-A nor anti-B

What is the universal Donor?
Type O
it will not elicit a response from the recipient’s immune system becaue it does not posses any surface antigens

Explain the Rf factor in blood
- is another antigen that may be present on the surface of red bloood cells
- Rh + = possesing the Rh antigen
- Rh - = lack the Rh antigen
Why is the Rh factor important for pregnancy?
- An Rh- woman can be sensitized by an Rh+ fetus if fetal red blood cells (which will have the Rf factor) enter maternal circulation during birth
- If this women subsequently carries another Rh+ fetus, the anti-Rh antibodies she produced when sensitized by the first birth may cross the placenta and destroy fetal red blood cells = erythroblastosis fetalis = severe anemia in the fetus
- not caused by anti - A and anti - B because they cannot cross the placenta
- Rhogam is a drug compreised of a mixture of anibodies given to mothers who are Rh- to prevent their immune system from attacking the fetal red blood cells
Explain the functions of the circulatory system
-
Transport of Gases:
- Erythrocytes transport O2 throughout the circulatory system
- Hemoglobin in erythrocytes bind to O2
- 1 hemoglobin = 4 oxygens because of the iron
- Hemoglobin also binds to CO2 - carbaminohemoglobin
- Hemoglobin in erythrocytes bind to O2
- Erythrocytes transport O2 throughout the circulatory system
-
Transport of nutrients and waste
- Amino acids and simple sugars are absorbed into bloodstream at the intestinal capillaries
- Throughout the body, metabolic waste products (water, urea, and CO2) diffuse into capillaries from surrounding cells, deliverd to appropriate excretory organs
-
Clotting
- When platelets come into contact with the exposed collagen of a damaged vessel, they release a chemical that causes neighboring platelets to adhere to one another = platelet plug
- Both the platelets and the damaged tissue release the clotting factor thromboplastin, which aid of its cofactors calcium and vitiamin K, converts the inactive plasma protein prothrombin** to its active for, **thrombin
- Thrombin converts fibrinogen** (another plasma protein) into **fibrin
- Threads of fibrin coat the damaged area and trap blood cells to form a clot
- Fluid left after the clotting is called serum

What is the airway passages?
Nose, pharynx (throat), larynx, trachea, bronchi, bronchioles and alveoli

Where does gas exchange between the lungs and the circulatory system?
in very thin walls of the alveoli
which ar air-filled sacs at the terminals of the airway branches
What are alternate functions of the respiratory system?
- Air over the vocal cords for the production of sound
- assists in the regulation of body pH by regulating he rate of carbon dioxide removal from the blood
Explain what happens during ventilation
-
Inhalation = diaphram contracts and flattens, and the external intercostal muscles contract, pushing the rib cage and chest wall up and out
- Phrenic nerve innervates the diaphram causing contraction and flattening
- action - thoracic cavity to increase volume
- reduces pressure, lungs expand
-
Exhalation = passive process. Lungs and chest walls are highly elastic and tend to recoil to their original position after inhalation
- Diaphragm and external intercostal muscles relax and chest wall pushed inward
- decreasing thoracic cavity volume, pressure increases
- Diaphragm and external intercostal muscles relax and chest wall pushed inward
What is surfactant used for in the lungs?
- Surfactant is a protein complex secreted by cells in the lungs to keep the lungs from collapsing by decreasing surface tension in the alveoli
How is ventilation controlled?
- Regulated by neurons (referred to as the respiratory center) located in the medulla oblongata
- when the partial pressure of CO2 in the blood rises, the medulla oblongata stimulates and increase in the rate of ventilation
How are oxygen levels monitored?
by peripheral chemoreceptors, which indirectly stimulate the respiratory center
changes in acid-base chemistry due to kidney function can also influence ventilation
Explain how gas is exchanged in the lungs
- Dense network of minute blood vessels called pulmonary capillaries surround the alveoli
- Gas exchange occurs by diffusion across the capillary walls and those of the alveoli
- gas moves from the higher partial pressure to the lower partial pressure
Explain the lung capacity diagram
- Total lung capacity - maximum volume of air the lungs can hold
- Tidal volume = volume of air moved during a normal resting breath , significantly less than lung capacity
- Inspiratory reserve volume = Volume of air that could be additionally inhaled into the lungs at the end of a normal, resting inhalation
- Expiratory reserve volume = the volume of air left in the lungs at the end of a normal, resting exhalation
- Vital capacity = volume of air moved during a maximum inhalation followed by a maximum exhalation
- Residual volume = even after maximum exhalation, there is always some air left in the lungs

What are the functions of the lymphatic system?
- Collect excess interstitial fluid and return it to the circulatory system, maintaining the balance of body fluid
- absorb chylomicrons from the small intestine and deliver them to cardiovascular circulation
What does hetrotrophic mean and what is an example?
- Heterotrophic = unable to synthesize all of their own nutrients
- humans
What is the path for raw material digestion?
- Ingested (eaten)
-
Digested (breakdown)
- consists of the degredation of large molecules into smaller molecules that can be absorbed into the bloodstream and used directly by cells
- Intracellular digestion: occurs within the cell, usually in membrane bound vesicles
- Extracellular digestion: digestive process that occurs outside the cell, within a lumen or tract
- consists of the degredation of large molecules into smaller molecules that can be absorbed into the bloodstream and used directly by cells
Explain the digestive tract
- Oral cavity
- pharynx
- esophagus
- stomach
- small intestine
- large intestine
- anus
- Accessory organs, such as the salivary glands, pancreas, liver and gallbladder, also play essential roles in digestion

Explain what occurs in the oral cavity
- mechanical and chemical digestion of food begins
- Mechanical - breakdown of large food particles into smaller particles through physical actions = mastication or churning motion
-
Chemical - enzymatic breakdown of macromolecules into smaller molecules when the salivary glands secrete saliva
- salive lubricates food to facilitate swallowing and provides a solvent for food particles
- Salive contains enzymes salivary amylase (ptyalin), which hydrolyzes starch to maltose (disaccharide)
- Creates a bolus
What is the function of salivary amylase (ptyalin)?
enzyme that hydrolyzes starch to maltose (disaccharide)
What is the function of the Esophagus in the digestive tract?
- Muscular tube leading from the mounth to the stomach
- Food is moved down esophagus by peristalsis
- The esophagus is closed off from the stomach by contraction of muscular structure called the lower esophageal (cardiac) sphincter
- Body of esophagus lies within the thoracic cavity, negatively pressured relative to the environment on inhalation
- abdominal cavity = positive pressure
- Therefore without normal defense mechanisms, leads to stomach acid in esophagus = aka, gastroesophageal reflux disease (GERD)
What are the physiologic changes associated with the gastroesophageal reflux (GERD)?
- Reflux can occur after spontaneous transient lower esophageal sphincter relaxation not associated with swallowing
- Patients with GERD usually have a decreased lower esophageal sphincter pressure (5-10 mmHg above gatric baseline pressure), leading to an increased passage of stomach contents into esophagus
- Resting pressures of the lower esophageal sphincter normally range from 15-35 mmHg above gastric baseline pressure
What is the function of the stomach in the digestive tract?
- Walls are lined by a gastric mucosa, contains gastric glands
- Mucous cells in gastric pits along the membrane secrete mucus to protect the stomach lining from the harsh acidic juices (pH = 2) in the stomach
- Chief cells found within the gastric glands synthesize pepsinogen, converted to pepsin upon contact with stomach acid and breaks down proteins
- Parietal cells, also present within gastric glands, synthesize and release HCL, which alters the pH of the stomach and kills bacteria and intrinsic factor, necessary for absorption of vitamin B12
- Churning of stomach (mechanical, combinded with enzyme activity (chemical) produces acidic, semifluid mixture of partially digested food = chyme
- passed to duodenum throug the pyloric sphincter
Explain the function of the small intestine in digestive tract
- Chemical digestion is completed in the small intestine
- Divided into three section:
- Duodenum
- Jejunum
- ilieum
- Highly adapted to absorption
- to max the SA, for digestion and absorption, the intestin is extremely long and highly coiled.
- Also contains projections called vili
- contain capillaries and lacteals (vessels of the lyphatic system)
- Amino acids and monosaccharides pass through the villi walls into the capillary system
- Blood from digestive tract enters portion of liver where it is detoxified and stripped of some of its nutrients
- Large fatty acids and glycerol pass into lacteals and are then reconverted into triglycerides in the liver
- Note glucose and Amino Acids are actively absorbed, require energy
Where does blood from the digestive tract enter from the small intestine?
- Into the liver
- Amino Acids and monosaccharides pass through the villi walls into capillary system (active transport)
- Large fatty acids and glycerol pass into the lacteals (lymphatic system vessels) and reconverted to triglyceride
Where does most of the digestion occur in the small intestines?
- Duodenum, where the secretions of the intestinal glands, pancrease, liver and gallbladder mix together with the acidic chyme entering from the stomach
What does intestinal mucosa secrete and what is it used for, digestion wise?
- Lipases - fat digestion
- aminopeptidase - polypeptide digestion
- disaccharideases - for maltose, lactose and sucrose digestion (eg. lactase)
What is the function of Gastrin hormone in the digestive tract
-
Gastin:
- Primary function = stimulate histamine and pepsinogen secretion as well as increase gastric blood flow
- Also stimulates parietal cells to produce HCL, which denatures proteins and activates digestive enzymes
- Produced in the G cells of the duodenum
- Primary function = stimulate histamine and pepsinogen secretion as well as increase gastric blood flow
What is the function of the Intrinsic factor hormone in the digestive tract
Intrinsic factor:
- Secretion of the parietal cells
- Function = facilitate the absorption of vitabmin B12 across the intestinal lining
What is the function of the Cholecystokinin (CCK) hormone in the digestive tract
Cholecystokinin (CCK):
- Produced and stored in the I cells of the duodenal and jejunal mucosa
- Function = stimulation of pancreatic enzymes and somatosatin secretion as well as gallbladder contraction
- acts as a hunger suppressant
What is the function of the Secretin hormone in the digestive tract
Secretin:
- Synthesized and stored in the S cells of the upper intestine
- Function = stimulates the secretion of bicarbonate-containing substances from the pancrease and inhibits gastric emptying and gastric acid production
What is the function of the liver in the digestive system?
-
Produces bile that is stored in the gallbladder before being released into the small intestine
-
bile contains no enzymes; it emulsifies fats, breaks down large globules into small droplets
- Emulsification of fat exposes a greater surface area of the fat to the action of pancreatic lipase
-
bile contains no enzymes; it emulsifies fats, breaks down large globules into small droplets
- Additional functions = storage of glycogen, converstion of ammonia to urea, protein synthesis, detoxification and cholesterol metabolism
What occurs in the absence of bile in the digestive system?
fats cannot be digested
What is the function of the pancrease in the digestive system?
-
Produces enzymes such as:
- amylase = carbohydrate digestion
- trypsin = protein digestion
- lipase = fat digestion
- When the pancrease releases chymotrypsin and enterokinase, enterokinase cleaves trypsinogen into trypsin
- Trypsin then cleaves and activates the other zymogens (enzyme precursors)
- Pancrease secretes a bicarbonate-rich juice that neutralizes acidic chyme from stomach
- Pancrease opperates optimally at this higher pH
What is the function of the large intestine in the digestive system?
approximately 1.5 m long and absorbs salts and any water not already absorbed by the small intesting
Rectum provides for transient storage of feces before elimination through the anus
What does deamination produce for metabolic waste and where?
Deamination of amino acids in the liver leads to the production of nitrogenous wastes, such as urea and ammonia
What are the principal organs of excretion in humans? explain each
-
lungs
- CO2 and H2O vapor diffuse from the blood and are continually exhaled
-
liver
- processes nitrogenous wastes, hemoglobin and other chemicals for excretion
- Urea is produced by the deamination of amino acids in the liver and diffuses into the blood for ultimate excretion in the kidnesy
-
skin
- excrete H2O and dissolved salts (urea)
- perspiration serves to regulate body temperature since the evaporation of sweat removes heat from the body
-
kidnesy
- functions to maintain the osmolarity of the blood, excrete numerous waste products and toxic chemicals and conserve glucose, salt and water
- Bile salts are excreted as bile and pass out with the feces
Explain the kidney’s overall function and location
- Function = regulate the concentration of salt and water in the blood through the formation and excretion of urine
-
Location/description = bean-shaped and located behind the stomach and liver
- each kidney is composed of approximately one million units called nephrons

Explain the structure of the kidney
- Kidney is divided into three regions:
- outer cortex
- Inner medulla
- renal pelvis
-
Nephron consists of:
- bulb = bowman’s capsule = embraces a special capillary bed called a glomerulus
- Bowman’s capsule leads to a long, coiled tube divided into funcionally distinct units:
- proximal convoluted tubule (cortex)
- Loop of Henle (medulla)
- distal convoluted tubule (cortex)
- collecting duct (medulla)
- Most of nephron is surrounded by a complex peritubular capillary network that facilitates reabsorption of amino acids, glucose, salt and water

Explain the steps to Urine Formation
-
Filtration:
-
Blood pressure forces 20% of blood plasma to glomerulus through capillary walls into Bowman’s capsule
- Fluid and small solutes entering = filtrate (isotonic with blood plasma)
- Passive process driven by hydrostatic pressure of blood
- high BP = high hydrostatic P and can lead to kidney damage overtime
- Passive process driven by hydrostatic pressure of blood
- Fluid and small solutes entering = filtrate (isotonic with blood plasma)
-
Blood pressure forces 20% of blood plasma to glomerulus through capillary walls into Bowman’s capsule
-
Secretion:
- nephron secretes waste substances such as acids, ions and other metabolites from the interstitial fluid into the filtrate by passive and active transport
-
Reabsorption:
- Essential substances (glucose, salts and amino acids) and water are reabsorbed from the filtrate and returned to the blood
- primarily occurs in proximal convoluted tubule and is an active process (water passive process)
- forms concentrated urine, hypertonic to the blood
- primarily occurs in proximal convoluted tubule and is an active process (water passive process)
- Essential substances (glucose, salts and amino acids) and water are reabsorbed from the filtrate and returned to the blood

Which particles are too large to filter through the glomerulus?
blood cells and albumin which remain in the circulatory system
What is the primary function of the nephron?
clean the blood plasma of unwanted substances as the filtrate passes through the kidney
Where is the primary site of nutrient reabsorption in the nephron?
proximal convoluted tubule

What function does the loop of henle and collecting duct play?
regulation of water, sodium and potassium concntrations in the nephron

What is the function of the distal confoluted tubule?
major site for secretion of substances into the filtrate

Explain each part of the loop of Henle
- Each part plays a distinct role in regulating water absorption and electrolyte concentration
- Descending = very permeable to water, but not to ions or urea
-
Ascending =
- thin = impermeable to water but permeable to ions, allowing for passive diffusion of ions
- thick = sodium, potassium and chloride are actively reabsorbed from the urine

Explain the osmolarity gradient that allows for the production of concentrated urine
- Osmolarity gradient between the tubules and the interstitial fluid surrounding them
- By exiting and re-entering at different segments of the nephron, solutes such as Na+ and Cl-, create this osmolarity gradient, with tissue osmolarity increasing from the cortex to the inner medulla
- gradient depends on the counter-current-multiplier system
- system in which energy is used to create a concentration gradient
- gradient depends on the counter-current-multiplier system

Explain the counter-current multiplier on the kidney, what hormone regulates it?
- Causes the interstitial space in the medulla to be hyperosmolar with respenct to the dilute filtrate in the renal tube
- filtrate travels down the collecting ducts to pelvis and ureter
- water flows from the ducts to the interstitial fluid through osmosis
-
The reabsorption zone of H2O in the kidneys depends on the permeability of the collecting ducts to water
-
regulation of the permeability of the ocllecting ducts to water is accomploished by antidiuretic hormone (ADH) = vasopressin
- ADH increases =increase permeability of collecting ducts to H2O,
- more water to be absorbed and higher urine concentration
*
- more water to be absorbed and higher urine concentration
- ADH increases =increase permeability of collecting ducts to H2O,
-
regulation of the permeability of the ocllecting ducts to water is accomploished by antidiuretic hormone (ADH) = vasopressin
Explain the two hormones that impact urine formation in the kidneys
-
Aldosterone:
- causes increased transport of sodium and potassium ions along the distal convoluted tubule and collecting duct
- results = decreased excretion of Na+ and increased excretion of K+ in urine
- additional water reabsorption
- results = decreased excretion of Na+ and increased excretion of K+ in urine
- causes increased transport of sodium and potassium ions along the distal convoluted tubule and collecting duct
-
Antidiuretic hormone (ADH):
- same effect, increased water reabsorption
- ADH directly affects water absorption by the distal convoluted tubules and collecting ducts, opening additional aquaporins (water channels) allowing water to reabsorbed more readily
Both Aldosterone and ADH cause a decrease in urine output and increase in blood pressure, allowing human body to compensate for periods of dehydration or other causes of low blood pressure
What are diuretics?
drugs that target different parts of the kidneys to cause an increase in urine production
increaseing the amount of water preent in the urine and therefore increasing urine secretion
Explain the maintenance of pH
- pH remains relatively constant at 7.4
- removal of CO2 by the lungs and hydrogen ions by kidneys
What laboratory tests for pH
- arterial pH
- arterial partial pressure of carbon dioxide (Pco2)
- plasma bicarbonate (HCO3-)
What are two types of acid-base disorders, name and describe
-
Respritory: affects the blood acidity by causing changes in the Pco2
- Compensation performed by respiratory system
-
Metabolic: affects the blood acidity by causing changes in the HCO3-
- Compensation performed by kidneys
- therefore take long time
- Compensation performed by kidneys

Which region of the kidney has the lowest solute concentration?
Cortex
In the nephron, amino acids enter the peritubular capillaries via?
reabsorption
Glucose reabsorption in the nephron occurs in the?
proximal tubule
Urin is ______ to blood?
hypertonic
What is the difference between Endocrine glands and Exocrine glands?
- Endocrine glands = synthesize and secrete chemical substances called hormones directly into the circulatory system
- Exocrine glands = such as the gallbladder, secrete substances trensported by ducts
Name the endocrine glands
- pituitary
- hypothalamus
- thyroid
- parathyroid
- adrenal
- pancrease
- testes
- ovaries
- pineal gland
- kidneys
- gastrointestinal glands
- heart
- thymus

Explain where the adrenal glands are and the overall components of it?
- Location: on top of the kidneys
- Consist of:
- Adrenal cortex
- Adrenal medulla
Explain the main way the Adrenal cortex responds to stress
- In response to stress, adrenocorticotropic hormone (ACTH), produced in the anterior pituitary, stimulates the adrenal cortex to produce more than two dozen different steroid hormones, collectively known as adrenocortical steroids (or corticosteroids):
- There are three major classes of corticosteroids:
- Glucocorticoids
- Mineralocorticoids
- Cortical sex hormones
- There are three major classes of corticosteroids:
In the bloodstream what is corticosteroids bound to?
bound to transport proteins called transcortins
Explain Glucocorticoids
Adrenal cortex
- such as cortisol** and **cortisone, involved in glucose regulation and protein metabolism
-
raise blood glucose levels by promoting protein breakdown and gluconeogenesis
- decreasing protein synthesis
- glucocorticoids are antagonistic to the effects of insulin
- release amino acids from skeletal muscles as well as lipids from adipose tissue
- permote the peripheral use of lipids and have anti-inflammatory effects
-
raise blood glucose levels by promoting protein breakdown and gluconeogenesis
Explain Mineralocorticoids
Adrenal Cortex
-
Aldosterone, regulate plasma levels of sodium and potassium and the total extracellular fluid volume
- Aldosterone causes active reabsorption of sodium and passive reabsoprtion of water in the nephron of kidney
- increase in blood volume and blood pressure
- Excess aldosterone = excess retention of water, hypertension (high blood pressure)
- Aldosterone causes active reabsorption of sodium and passive reabsoprtion of water in the nephron of kidney
- Mineralocorticoids are stimulated by angiotension II and inhibited by ANP (atrial natriuretic peptide)
Explain Cortical sex hormones
Adrenal Cortex
- In both men and women, AC secretes small quantities of androgens (male sex hormones) like androstenedione and dehydroepiandrosterone
- In men, most androgens are produced by testes, so the physiologic effect of the andrenal androgens is quite small
- Women, however, overproduction of adrenal androgens may cause excess facial hair, etc.
What is the adrenal medulla responsible for?
- “Fight or flight”
- Two hormones:
-
Epinephrine (adrenaline)
- Increases the conversion of glycogen to glucose in liver and muscle tissue, increase in blood glucose and basal metabolic rate
- Norepinephrine (noradrenaline)
- Both:
-
increase rate and strength of the heartbeat and dilate and constrict blood vessels,
- increase blood supply to skeletal muscles, heart and brain
- decrease blood supply to kidneys, skin and digestive tract
- promote release of lipids by adipose tissue
- also neurotransmitters
-
increase rate and strength of the heartbeat and dilate and constrict blood vessels,
-
Epinephrine (adrenaline)
- Both of which belong to the class of amino acid-derived compounds called catecholamines
Explain the Pituitary gland
- The pituitary (Hypophysis) is a small, trilobed gland at the base of the brain
-
two main lobes:
- Anterior
- Posterior
- Hangs below the hypothaamus and is connected to it by a slender cord = infundibulum
Explain the Anterior pituitary function
-
Synthesizes both:
- direct hormones - directly act on target organs
- tropic hormones - stimulate other endocrine glands to release hormones
- Hormonal secretion of the anterior pituitary are regulated by hypothalamic hormones = releasing/inhibiting hormones or factors
What are the direct hormones that the anterior pituitary produces (name and describe)?
Direct hormones - direct effect
-
Growth hormones (GH, somatotropin):
- Promotes bone and muslce growth
- promotes protein synthesis and lipid mobilization and catabolism
- deficiency - dwarfism, over production = gigantism
- adults over production = acromegaly
-
Prolactin:
- stimulates milk production in female mammary glands
What are the tropic hormones that the anterior pituitary produces (name and describe)?
tropic = stimulate other endocrine glands
-
Adrenocorticotropic hormone (ACTH):
- stimulates adrenal cortex to synthesize and secrete glucocorticorids and regulate corticotropin-releasing factors (CRF)
-
Thyroid-stimulating hormone (TSH):
- stimulates thyroid gland to synthesize and release thyroid hormone, including thyroxin
-
Lutenizing hormone (LH):
- Women: stimulates ovulation and maintenance of corpus luteum and regulates progesterone secretion
- Men: stimulates interstitial cells of testes to synthesize testosterone
-
Follicle-stimulating hormone (FSH):
- Women: maturation of ovarian follicles, turn secrete estrogen
- Men: maturation of the seminiferous tubules and sperm production
-
Melanocyte-stimulating hormone (MSH):
- secreted by intermediate lobe of pituitary. Mammals function unclear, darkening of skin pigment melanophore cell dispersion
-
Endorphins:
- neurotransmitters that help pain-relieving properties
Describe the posterior pituitary and its hormones
- The posterior pituitary (neurohypophysis) does not synthesize hormones; it stores and releases the peptide hormones:
-
Oxytocin:
- secreted during childbirth, increases the strenth and frequency of uterine muscle contractions
- stimulates milk secretion in mammary glands
-
Antidiuretic hormone (ADH, vasopressin):
-
increases the permeability of the nephron’s collecting duct to water
- promoting water reabsorption, increase blood volume, increases blood pressure
- Secreted when plasma osmolarity increases, sensed by osmoreceptors in hypothalamus,
- or when blood volumes decreased, sensed by baroreceptors in the circulatory system
-
increases the permeability of the nephron’s collecting duct to water
-
Oxytocin:
- Which are both produced by the neurosecretory cells of the hypothalamus
- hormone secretion is stimulated by action potentials descending from the hypothalamus
Explain the hypothalamus
- part of forebrain and located directly above the pituitary gland
- receives neural transmission from ther parts of the brain and from peripheral nerves, triggering response from neurosecretory cells
- these cells regulate pituitary gland secretion via negative feedback and inhibiting/releasing hormones
Explain the function of GnRH
stimulates the anterior pituitary to secrete FSH and LH
Explain the feedback when plasma levels of adrenal cortical hormones drop
- hypothalamic cells (via a negative feedback mechanism) release corticotropin-releasing factor (CRF) into the portal system, which signals the pituitary cells to release ACTH
- ACTH then acts on the adrenal cortex to increase glucocorticoid levels
- when the plasma concentration of corticosteroids exceeds the normal plasma level the steroids themselves exert an inhibitory effect on the hypothalamus
Explain the hypothalamus interaction with the posterior pituitary
Neurosecretory cells in the hypothalamus synthesize both oxytocin and ADH and transport them via their axons into the posterior pituitary for starage and secretion
Explain the thyroid gland
- Thyroid hormones affect the function of nearly every organ system in the body
- children, these hormones are essential for growth and neurological development
- adults, hormones increase the rate of metabolism throughout the body and maintenance of metabolic stability
What are the thyroid hormones, name and describe
- Thyroxine (T4)
- Triiodothyronine (T3)
-
Calcitonin: “tones the bone”
- antagonist to parathyroid hormone (PTH)
- T4 and T3 formed from glycoprotein thyroglobulin, synthesized in thyroid cells
Explain the characteristics between thyroxine (T4) and triiodothyronine (T3) hormones of the thyroid
- T3 is 5 times more potent than T4
- T4 and T3 are transported via plasma proteins
- All of the T4 in the body is formed and secreted by the thyroid gland; however, 20% of T3 is produced by the thyroid gland
- The majority of T3 is produced by conversion of T4 to T3 by the enzyme 5’-monodeiodase, found primarily in the peripheral tissues
Explain the common issues/illnesses with thyroid
-
Hypothyroidism = thyroid hormones are undersecreted or not secreted at all
- Symptoms = slowed heart rate, respiratory rate slowed, fatigue, cold intolerance, weight gain
- Infants = cretinism - mental retardation and short stature
-
Hyperthyroidism = thyroid is overstimulated, over secretion of thyroid hormones
- Symptoms = increased metabolic rate, feels of excessive warmth, profuse sweating, palpitations, weight loss, and protruding eyes
Both normally due to a thyroid enlarged, formoing a bulge in the neck called a goiter
Explain the function of the pancrease in the endocrine system
- The pancrease is both an exocrine organ and an endocrine organ
- exocrine function = performed by the cells that secrete digestive enzymes into the small intestine via series of ducts
-
endocrine function = performed by small glandular structures called the islets of Langerhans, alpha and beta cells
- alpha cells = glucagon
- beta cells = insuline
Name and describe the function of the pancreas hormones
-
Glucagon
- stimulates protein and fat degradation, conversion of glycagen to glucose, and gluconeogenesis = increase blood glucose
- antagonist to insulin
-
Insulin
- stimulates uptake of glucose by muscles and adipose cells and storage of glucose as glycagen in muscles and liver cells = lowering blood glucose
- Stimulates synthesis of fats from glucose and uptake of amino acids
- antagonistic to glucagon and glucocorticoids
Explain diabetes mellitus
underproduction of insulin, or insensitivity to insulin
= hyperglycemia (high blood glucose levels)
Explain the difference between type I and type II diabetes
see attached

Explain the parathyroid glands
- Four small, pea-shaped structures embedded in the posterior surface of the thyroid
- Synthesize and secrete parathyroid hormone (PTH), which regulates plasma Ca2+ concentration
- PTH raises the Ca2+ concentration in the blood by breaking down bone and decreasing Ca2+ excretion in the kidneys
- Calcium is bound to phosphate in bone, PTH compensates for the increase in phosphate by stimulating excretion of phosphate by the kidneys
Explain the kidneys as an endocrine system
- When blood volume falls, the kidneys produce renin
- enzyme that converts plasma protein angiotensinogen to angiotensin I
-
Angiotensin I is converted to angiotensin II, stimulates the adrenal cortex to secrete aldosterone
- Aldosterone = helps restore blood volumes by increasing sodium reabsorption by kidneys = increased fluid retention
-
Angiotensin I is converted to angiotensin II, stimulates the adrenal cortex to secrete aldosterone
- enzyme that converts plasma protein angiotensinogen to angiotensin I
- Kidneys also produce erythropoietin (EPO)
- glycoprotin that stimulates red blood cell production
What does erythropoietin (EPO) cause?
stimulates red blood cell production, produced in the Kidneys
- Stimulation of the stem cells to differentiate into rubriblasts (least mature erythrocytes)
- Increased rate of mitosis
- Increased release of reticulocytes from the bone marrow
- Increased hemoglobin (HgB) formation, which results in the critical HgB concentration necessary for RBC maturity to be reached at a more rapid rate












































