Biochemistry of Vision - SRS Flashcards
The retina is made up of the Ora Serrata, nonsensory retinal pigment epithelium, and sensory retina. What are the three parts of the sensory retina?
–Macula lutea
–Fovea centralis
–Optic disk
What are the cell types of the retina?
Neurons
Retinal Pigment cells (RPE)
Neuron support cells
What types of neurons are found in the retina?
Photoreceptor cells (rods and cones)
Retinal ganglion cells
Interneurons (integrating neurons)
What are the types of interneurons found in the retina?
Bipolar cells
Horizontal cells
Amacrine cells
Where are RPE’s found?
Retinal pigment epithelial cells are found in the outermost layer seperating the retina from the choroid.
What are the neuron support cells of the retina known as?
Mueller cells
In order of signal transduction, name the ten layers of the retina! Go!
- Pigment epithelial cells (RPE)
- Photoreceptor cells
- Outer limiting membrane
- Outer nuclear layer
- Outer plexiform layer
- Inner nuclear layer
- Inner plexiform layer
- Ganglion cell layer
- Optic nerve fibers
- Inner limiting membrane
Rods pick up light of differing intensities and are peripheral, what photopigment do they posess?
Rhodopsin
Cones are located in the fovea and detect blue, red and green. What photopigment do they contain?
Iodopsin
What connects the photoreceptors and the RPE?
Interphotoreceptor matrix
The interphotoreceptor matrix is important in recycling and uses the interstitial retinoid binding protein (IRBP) to do what?
What else does this matrix do?
Transports retinol to the RPE and Retinal to the photoreceptor
Also, shedding of older disks
RPE contains melanin grandules and phagocytose shed disks. These disks are degraded in lysosomes and released into choriocapillaries. What enzye does the RPE express and what function does it serve?
Retinol re-isomerization enzyme
•Enzymatic conversion of 11-cis retinal to retinol
Rods end in rod sperule, what components of cells are involved in this?
Dendrites of bipolar cells
Neurites of horizontal cells
Cones end in cone pedicles, what cell processes are involved here?
Dendrites of bipolar cells
Neurites of horizontal cells
What is iodopsin composed of?
Opsins and chromophore (11-cis retinal)
When blue, green and red are stimulated together, what light is seen?
White
In a process called bleaching, a photopigment absorbs a photon of light and changes conformation of 11-cis-retinal. What does the photopigment then act as?
A GPCR -
- Induces GMP from cGMP
- cGMP dependent Na+ channels close
Leber congenital amaurosis type II involves the RPE65 gene and isomerohydrolase conversion of all-trans retinol to 11-cis-retinal. What is the inheritance pattern? What is the delivery vector?
Autosomal recessive
Adenoviral delivery vector
Bipolar cells recieve impulses from photoreceptor cells . What are the types that recieve input from multiple photoreceptors?
Diffuse cone bipolar cells
Rod bipolar cells
Midget cone receptors recieve input from one photoreceptor and communicate with?
One ganglion cell
Ganglion cells have dendrites in the inner plexiform layer and come in two varieties. What are they?
Diffuse ganglion cells - contact with several bipolar cells
Midget ganglion cells - contact with a single bipolar cell
Association neurons integrate signaling. What are the two types of these?
Amacrine cells
Horizontal cells
Where do amacrine neurites end?
Axon terminals of bipolar cells and the ganglion cell dendrites and bodies
Where do the neurites of horizontal cells end?
On cone pedicals and rod spherules
The fovea is the visual axis of the cornea, and is a depression in the retina or a flattening of the inner layers that serves to let light in. This area has the greatest visual discretion. Why?
»The most neuronal interconnections for the most representation in the visual cortex
What are the photoreceptors of the fovea?
Under what conditions does the fovea perform poorly?
–Almost exclusively cones
»Poor in low light
Age-related macular degeneration occurs rapidly and with painless vision loss. It comes in two varieties, wet and dry. What is the etiology of each?
Dry: photoreceptor cells and the RPE at the macula break down
Wet: abnormal blood vessels grow under the macula. The new blood vessels leak blood and fluid, raising the macula from its close association with the choriocapillaris.
The optic nerve is the convergence of the axons of retinal ganglion cells, which are unmyelinated afferent fibers. Where does myelination begin?
The optic disc
What is the blood supply of the retina provided by?
Choroid: outer retina
Central retinal artery
The central retinal artery rises from the optic nerve head and supplies the inner retina via brances that supply three layers of capillary networks. How do these branches run?
How deep can capillaries be found?
•Branches run posterior to the inner limiting membrane, within the nerve fiber layer
–Capillaries can be found running through the retina but generally no deeper than the outer plexiform or nuclear layer
What happens in retinal detachment?
The photoreceptor cell layer is detached from the pigment epithelial layer. This can lead to blindness.
Why is detachment of the photoreceptor cell layer from the RPE and Choroid such a huge problem?
RPE is needed to maintain support of visual function
Choroid is needed to nourish and maintain cells.
What percentage of diabetics will develop some kind of retinopathy?
How long after diagnosis does this typically occur?
How is this different for DM I?
60-80%
15-20 years after diagnosis
Nearly all type I diabetics will develop after 20 years, of which 50% will be proliferative
What do microaneurysms look like in histopathology?
Small outpouchings from retinal capillaries
What causes cotton-wool spots?
Regional failure of retinal microvascular circulation resulting in ischemia.
Describe the histopathology of diabetic retinopathy.
(This is a pretty robust slide, but I think it’ll be a test question. So stick with it!)
- –Microaneurysms
- Small outpouchings from retinal capillaries
- –Cotton-wool spots
- Regional failure of retinal microvascular circulation resulting in ischemia
- –Retinal veins
- Dilated and tortuous
- –Retinal arteries
- White and non-perfused
- Eventually absent of endothelial cells
- –Solely basement membrane
- –Selective loss of pericytes
- From retinal capillaries
- –Pericytes contain smooth muscle actin and help regulate capillary blood flow
- –Apoptosis of capillary endothelial cells
What are the classes of diabetic retinopathy?
Preproliferative and proliferative
In preproliferative diabetic retinopathy there is increased size and number of intraretinal hemorrhages. What does most vision loss occur from?
How do we treat?
Macular degeneration
Would not treat unless clinically significant
Proliferative diabetic retinopathy includes the formation of new blood vessels. What does this neovascularization lead to?
»Can protrude into vitreous
- Hemorrhage here and cloud vision
- Detach retina
»Can eventually extend into and grow from other structures in the eye
- Causing secondary forms of blindness
How do we detect diabetic retinopathy?
Fundoscopy (opthalmoscopy)
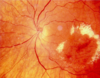
What type of diabetic retinopathy?
What key features are seen?

Nonproliferative
Hemorrhages and exudates
What type of DR is this?
Key features shown here?
Nonproliferative
Ring of exudates around the macula
Type of DR?
Key features?

Proliferative DR
Neovascularization of disc and other structures
What type of DR is this?
Key features shown here?

Nonproliferative
Flame shaped hemorrhages
What type of DR is this?
Key features shown here?

Proliferative
Boat shaped hemorrhages
(under internal limiting membrane)
What type of DR is this?
Key features shown here?

Proliferative DR
Fibrous vitreous bands
What type of DR is this?
Key features shown here?

Nonproliferative DR
Tortuous vessels
How can we visualize hemorrhages and neovascularization that are difficult to see with the human eye?
Fluorescein angiography
–Sodium fluorescein dye is injected into a vein in the patient’s arm
–Retinal photography captures green fluorescence in the retina
How does optical coherence tomography work?
What does it detect?
–Uses the interference pattern of infrared beams to create a cross section of the retina
–Retinal thickness increases in DR and ME


