Basic Ultrasound Flashcards
1
Q
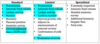
Levels of ultrasound procedures
A
- Standard/Basic
- Limited
- Specialized (when fetal anomaly suspected)
2
Q
AWHONN Scope of Practice
1st trimester ultrasound
A
- +/- gestational sac
- Fetal #
- +/- cardiac activity
- Estimated GA via CRL
- +/- IUP
- Identify 1st tri complications:
- Anembryonic pregnancy
- Ectopic pregnancy
- Threatened, incomplete, complete, or misses AB
- Molar pregnancy
- Multiple gestation
3
Q
AWHONN Scope of Practice
2nd+3rd trimester ultrasounds
A
- fetal #
- +/- cardiac activity
- Fetal presentation
- Placental location
- Amniotic fluid volume
- BPP and modified BPP
- Biometric measurements: EFA and EFW
- Cervical length measurements
- Adjunct to US guided procedures
4
Q
Common ultrasound indications
A
- Evaluation of fetal growth
- Suspected fetal abnormality
- Adjunct to special procedures (le amnio)
- Uterine evaluation
5
Q
Which 2 probes do we use the most in OB/GYN
A
- 3.5 MHz convex probe (abdomen, OB/GYN)
- 6.5 MHz transvaginal probe
6
Q
Where do you orient the transducer notch?
A
- Notch oriented towards person’s head
- Left side of ultrasound screen = head
- Right side = feet
7
Q
What are the different ultrasound modes?
A
- B-mode: “Brightness mode”
- 2D ultrasound in grey scale using real time.
- Used 99% of time
- M-mode: “Motion mode”
- Cursor line on fetal heart and shows motion of fetal heart, estimates FHR
- Doppler
- Color - shows direction of flow
- Towards transducer = red
- Away from transducer = blue
- Power - amplitude
- Spectral - velocity
- Color - shows direction of flow
8
Q
Define: echogenic
A
The ability of a structure to produce echos
9
Q
Define: anechoic
A
- No echos
- Appears black on ultrasound
10
Q
Define: hypoechoic
A
- Less reflective and low amount of echoes when compared with neighboring structures
- Appears as varying shades of darker gray
11
Q
Define: hyperechoic
A
- Highly reflective & echo rich when compared with neighboring structures
- Appears as varying shades of gray
- Echogenic is often used interchangeably
12
Q
Define: isoechoic
A
- Having similar echogenicity to a neighboring structure
13
Q
Define: homogenous (texture)
A
- Organ parenchyma is uniform in echogenicity
14
Q
Define: inhomogenous/heterogenous (texture)
A
- Organ parenchyma is not uniform in echogenicity
15
Q
Define: reverberation
A
- Artifacts that appear as multiple equally spaced lines along a ray line.
- Caused by the sound bouncing back and forth between tissue boundaries and then returning to the receiver



