Atherosclerosis/Vascular Disease Flashcards
Triphasic wave form
- strong forward component of blood flow during systole
- short reversal of blood flow during early diastole
- low amplitude foward blood flow during remaining diastole (loses vacuum, going back)
INACTIVE - when exercise - both systolic and diastolic flow increase

Bernoulli’s
as speed of a moving fluid increass, pressure within fluid decreases (and speed increases)
75% - flow begins to decreases and pressure downstream decreases to form a pressure gradient

aneurysm vs diffuse ectasia
smaller increase generaly in diameter = de
aneurysm - widen, dilate (at least 50% increase over normal arterial diameter)
AAA
cystic medial degeneration - of elastic fibers
acuumulation of collagenous and mucoid material in the medial layer
mostly with aging and hypertension (marfan, ehlers danlos)
Type A Aortic Dissection
involves part of ascendinga aorta
surgical!
emergency and high mortality
lower BP in all

Type B Aortic Dissection
does not involve ascending aorta
complicated - surgical
uncomplicated - medical
AAA risk factors
increasing age
smoking
male
genetic
aortic wall tension
variation in wall tension in aneurysm
proportional to the product of pressure and radius
bigger radius = more tension = bigger chance of ruptiur
P is the same
AAA therapy
medican (smoking HTN)
endovascular/open therapy
PAD mechanism
if stenosis - high resistance
turbulent flow - pressure drops across stenosis and impaired endothelial function
inapility to increase flow with execise
mismatched O2 supply and demand (IC)
inefficient oxidation
can’t dilate because endothelial dysfunction - angina and claudation

claudication
cramping tightness aching fatigue
bluttock, hip, thigh, calf, foot
exercise induced
not with stating (relief)
less than 5 min
ABI
Under .90 is PAD!
measure P in both arms and legs
put highest angle P over highest arm P on eich side
add 2 numbers together

Toe Brachial Pressure
divide te pressure by higher of the two brachial ressures
when ABI not possible because calcified
PAD therapy
exercise
smoking cessation
STATINS
HTN
antiplatelets
symtomatic relief
revascularization (if gangrene, non healing ulcers, ischemic rest paid, bad claudication)
Raynauds Disease
rare disease that causes vasospasm of the arteries and reduces blood flow to fingers and toes
idiopathic or secondary (lupus, sjogrens)
vascular constriction - white/blue/numb extremities
Treatment for Raynauds Disease
CCBs
Alpha block
ARBs (vasodilate)
surgery (rare)
varicose veins
dilated tortuous veins
reflux bc valvular insufficiency
obesity, prenancy, familial
usually cosmetic - can be stasis dermatitis
Carotid artery disease therapy
can lead to stroke!
antiplatelet/anticoagulation
statins
risk factor modification (smoking, HTN, diabetes)
revascularization (stenting)
arteriovenous malformation
embryonic/fetal development
direct connections between arteries and veins! more common in brain or SC
risk factors for CAD
herediatry
lipids (high LDL)
smoking
diabetes
HTN
obesity
CRP
inflammation marker
predictor of first MI/ischemic stroke (also high if another stressor)
Atherosclerosis Pathway
- endothelial injury
- LDLs enter, smoooth muscle cells migrate
- macrophages roll and enter epithelial cell and eat LDL and turn into foam cell
- secrete cytokines to recruit more
- more macrophages enter - fatty streak
- TGF beta increases collagen
macrophages make MMP-9 which breaks down fatty cap

Thinning of fibrous cap
degraded by foam cells secreting MMP
rupture!!

synthesis of fibrous cap
smooth muscle cless promote collagen and elastin

NO mechanism
ACH/sheer stress - cleave cNOS to NO
moves across wall and increases cGMP to stim smooth muscle cell relaxation

CT scan
regular scan or use for coronary calcium studies
characteristics of angina
intermittent, recurrent
strangling, pain, pressure, tightness
location - retrosternal, shoulders - arms
dyspnea
30 s - 10 min
plaque and ischemic impact
stenotic - few, fibrotic, thick cap, less compensatory enlargement (ischemia - angina, postive stress test)
non-stenotic - many, lipid rich, thin cap, compensatory enlargement (infarction)
therapeutic targets
lower LDL (source of inflammation and building blocks of plaques) - stop progression and decrease chance of rupture
dampen inflammation and restore homeostasis
restore fibrous cap
intima
where everything happens
pathophysiology of atherosclerosis
- endothelial dysfunction (increased permeability, WBC adhesion)
- smooth muscleemigration from media to intima, macrophage activation
- liids from blood enter intima and phagocytosesd by macrophages in intima
- smooth muscle proliferation, collagen and other ecm deposition, extracellular lipid
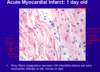
1-2 don’t see anything, 3-4 do see

complications from atherosclerosis
thrombosis
embolism
aneurysm and rupture
dissection
true aneurysm
dilation of segment of vessel
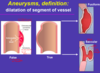
false aneurysm
dissection
extravasation of blood
looks like true aneurysm

fusiform aneurysm
true aneurysm
in the brain
saccular aneurysm
brain
true aneurysm

etiologies of aneurysms
atherosclerotic**
infectious
inflammatiory
autoimmune
degenerative
traumatic
Giant Cell Arteritis
large vessels - head
headches
visual problems
steroids!
usually older people, inflammation of arteries around forehead
Polyarteritis Nodosa
middle vessels
transmural inflammation
necrossis and thickening
fever, weight loss, abdominal pain
corticosteroids
Wegener Granulomatosis
respirator involvement
acute necrotizing granulomas and vasculitis
fever, mucosal alterations
80% death if unreaed
thromboangiitis obliterans (Buerger’s disease)
smokers,
segmntal thrombising infammation of distal limb arteries
ulcerations of toes, feet, fingers, gangrene
smoking cessation is only thing that helps!
DVT etiology
OCP
dehydration
inactivity
surgery
trauma
MI
strok
DVT therapy
Heparin
chylomicron
absorbed cholesterl from brush border into lymph to liver
primordial prevention
prevent the development of risk factors for CVD
primary prevention
prevent the first CVD event
secondary prevention
prevent subsequent CVD events (decrease LDL)
Bile Acids Mechanism
breakdown product of cholesterol - most is reabsorbed in the small bowel
act as a detergent - make cholesterol soluble
Bile Acid Resins
i.e. WelChol
No outcomes data!!
Used as add on for additional LDL lowering
inhibits cholesterol absorption
They disrupt the enterohepatic circulation of bile acids by combining with bile constituents and preventing their reabsorption from the gut
Liver makes more bile acids since it is not reabsorbled, which uses a lot of LDL cholesterol (liver compensates so not as effective)
Bile acid resin Side Effects
bloating
interfere with absorption of vitamins or meds
can raise TG
Ezetimibe
selective cholesterol absorption inhibitor
acts on brush border to inhibit reabsorption of cholesterol itself
Liver has to absorb more cholesterol from blood
** mainly add on to statins
Ezitimide - decreases events?
yes!
with a statin
Niacin
decreases VLDL production, LDL formation, increases hepatic clearance of LDL precursors
raises HDL
NO decrease in events
Niacin side effects
gout!! elevated uric acid levls
hepatic toxicity
flushing and pruritis
Fibrates Indications
lowers TG by a lot! no real effect on LDL, raises HDL a little
used for severe hypertriglyceridemia
hgih TH or low LDL
Fibrates Mechanism
activate PPAR alpha - activates lipoprotein lipase and increases lipoysis in the plasma
Fibrates side effects
avoid in patients wiht hepatic/renal function issues
increased risk with statins of rhabdomyolysis
HMG-CoA Reductase Inhibitor Mechanism
Statin!!
if inhibit - increase HMG-CoA to make more cholesterol but also increase transcription of LDL R so take more out of blood and decrease LDL by a lot

Statin - decrease events?
yes!!
Statin side effects
increase in transaminasess
muscle pain or weakness
Statin studies
primary prevention!
educe morbidity and mortality
cost effective
lifestyle also needed
PCSK9 mechanism
antibody to LDL -R that allows it to be destroyed - dysfunctional!
more LDL-R because it is recycled
decrease LDL by a olot - decrease events!
PCSK9 Side Effects
injection site swelling
how to lower TGs?
fibrates
niacin
fish oil
(not as important as LDL)
how to lower LDL?
statins
ezetimibe
pcsk9 abs
bile acid resins
niacin
what happens from vessel injury?
vasoconstriction (reduced blood flow)
platelet adhesion/activation/aggregation
blood coagulation cascade
local control of vasoconstriction
thromboxane and other local controls released
systemic control of vasoconstriction
epinephrine
extrinsic pathway
damage to tissue outside the vessel activates factor X
first pathway to start but turns off when a little factor Xa is made
vessel injury
triggered by tissue factor
intrinsic pathway
after extrinsic pathway makes a little Xa and is turned off
most fibrin is made from intrinsic pathway
initation of the clotting cascade
interaction of plasma bound TF exposed by vascular injury
interacts with factor 7 (extrinsic)
activates factor 10
10a acivates a small amount of thrombin and TFPI which rapidly inactivates the pathway!

Extrinsic Xase
TF + VIIa
activates factor XI and facor X
thrombin generation
primed by extrinsic pathway but becomes reliant on intrinsic pathway to make Xa
Intrinsic Xase
IXa + VIIIa
greatly amplifies Xa
Prothrombinase Complex
Xa + Va
explosive generation of thrombin

Factor v Leiden
mutated form of factor V cannot be inactivated by protein C
tons of V –> clots
What does thrombin activate?
XI, V, 13

formation and stabilization of fibrin
thrombin hydrolyzes fibrinogen to fibrin
calcium - acts like glue to hold fibrin monomers together (loose insoluble fibrin polymer - clot)
factor XII also activated by thrombin and stabilizes the fibrin polymers

what does thrombin do?
- activate protein C (anti inflammatory - helps dissolve clot)
- activate platelests
- form fibrin
Vitamin K dependent factors
thrombin, Vii, IX, X
protein C and S
TFPI
synthesized in endothelial cells
present in plasma and platelets
inhibits Xa, VIIa and TF

Antithrombin
circulating plasma protease inhibotr
neutralizes many enzymes in the clotting cascade (esp thrombin and factor Xa)

Protein C/Protein S
inhibit coagulation cofactors V and VIII (inactivate prothrombinase and Intrinsic Xase

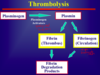
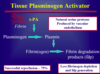
fibrinolysis
normal hemostatic response to vascular injury (body doesn’t need clot anymore
plasminogen –> plasmin (intrinsic and extrinsic factors
release of tPA from endothelial cells!
plasmin digest many of the proteins cleave peptide bonds

intrinsic activation of plamsin
XIIa
extrinsic activation of plasmin
tPA and urokinase
activate plasmin
activate fibrin
d dimer
major fibrin degredation factors
sign that high clot burden
tissue factor
initates coagulation
prostacyclin
vasodilation/inhibition of platelet aggregation
NO
vasodilation/inhibition of platelet aggregation
vWF
platelet collagen adhesion - complex with factor VIII
AT
inhibition of blood coagulation